Abstract
Purpose
To describe the clinical and multimodal imaging (MMI) features of age-related macular degeneration (AMD) eyes presenting with intraretinal exudation and no evidence of neovascularization or structural alterations of native retinal vessels.
Methods
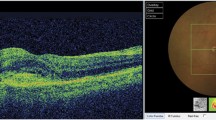
This was a retrospective review of the MMI and electronic health records for 3 consecutive patients presenting with unilateral exudative non-neovascular age-related macular degeneration. MMI included confocal color fundus photography (CFP), fundus autofluorescence (FAF), fluorescein angiography (FA), spectral domain optical coherence tomography (SD-OCT), swept-source optical coherence tomography angiography (SS-OCTA), and spectral domain optical coherence tomography angiography (SD-OCTA). Dense B-scan OCTA (DB-OCTA) patterns and implemented image post-processing were used to improve spatial resolution in the OCTA analysis and remove projection artifacts.
Results
Three eyes of 3 patients (1 male and 2 females, ages 72–87) developed intraretinal fluid (IRF) producing retinal edema during regular follow-up for non-neovascular AMD. FA, SS-OCTA, and DB-OCTA demonstrated no evidence of macular neovascularization or discrete retinal vascular abnormalities that could explain the IRF accumulation. Two eyes received intravitreal anti-VEGF therapy and demonstrated prompt resolution of IRF with periodic recurrences over time.
Conclusion
Exudative non-neovascular AMD is a novel clinical phenotype characterized by the presence of non-neovascular intraretinal exudation producing macular edema. Differentiating this condition from other manifestations of AMD requires appropriate use of MMI. Further study is needed to assess the clinical impact and optimal management of exudative non-neovascular AMD.









Similar content being viewed by others
Data availability
Not applicable.
References
Daruich A, Matet A, Moulin A et al (2018) Mechanisms of macular edema: beyond the surface. Prog Retin Eye Res 63:20–68. https://doi.org/10.1016/j.preteyeres.2017.10.006
Schmidt-Erfurth U, Waldstein SM (2016) A paradigm shift in imaging biomarkers in neovascular age-related macular degeneration. Prog Retin Eye Res 50:1–24. https://doi.org/10.1016/j.preteyeres.2015.07.007
Spaide RF, Jaffe GJ, Sarraf D et al (2020) Consensus nomenclature for reporting neovascular age-related macular degeneration data: consensus on neovascular age-related macular degeneration nomenclature study group. Ophthalmology 127:616–636. https://doi.org/10.1016/j.ophtha.2019.11.004
Nagiel A, Sarraf D, Sadda SR et al (2015) Type 3 neovascularization: evolution, association with pigment epithelial detachment, and treatment response as revealed by spectral domain optical coherence tomography. Retina (Philadelphia, PA) 35:638–647. https://doi.org/10.1097/IAE.0000000000000488
Querques G, Kuhn D, Massamba N et al (2011) Perifoveal exudative vascular anomalous complex. J Fr Ophtalmol 34:559.e1–559.e4. https://doi.org/10.1016/j.jfo.2011.03.002
Sacconi R, Freund KB, Yannuzzi LA et al (2017) The expanded spectrum of perifoveal exudative vascular anomalous complex. Am J Ophthalmol 184:137–146. https://doi.org/10.1016/j.ajo.2017.10.009
Dansingani KK, Naysan J, Freund KB (2015) En face OCT angiography demonstrates flow in early type 3 neovascularization (retinal angiomatous proliferation). Eye (Lond) 29:703–706. https://doi.org/10.1038/eye.2015.27
Miere A, Querques G, Semoun O et al (2015) Optical coherence tomography angiography in early type 3 neovascularization. Retina (Philadelphia, Pa) 35:2236–2241. https://doi.org/10.1097/IAE.0000000000000834
Miere A, Querques G, Semoun O et al (2017) Optical coherence tomography angiography changes in early type 3 neovascularization after anti-vascular endothelial growth factor treatment. Retina (Philadelphia, PA) 37:1873–1879. https://doi.org/10.1097/IAE.0000000000001447
Sacconi R, Sarraf D, Garrity S et al (2018) Nascent type 3 neovascularization in age-related macular degeneration. Ophthalmol Retina 2:1097–1106. https://doi.org/10.1016/j.oret.2018.04.016
Spaide RF (2019) New proposal for the pathophysiology of type 3 neovascularization as based on multimodal imaging findings. Retina (Philadelphia, PA) 39:1451–1464. https://doi.org/10.1097/IAE.0000000000002412
Bacci T, Freund KB (2020) High-resolution OCT angiography features of an early type 3 neovascularization. Ophthalmology 127:887. https://doi.org/10.1016/j.ophtha.2020.03.036
Breazzano MP, Bacci T, Curcio CA, Freund KB (2020) Novel multimodal imaging and volume rendering of type 3 macular neovascularization. Retina (Philadelphia, Pa). https://doi.org/10.1097/IAE.0000000000002892
Sacconi R, Borrelli E, Sadda S et al (2020) Nonexudative perifoveal vascular anomalous complex: the subclinical stage of perifoveal exudative vascular anomalous complex? Am J Ophthalmol 218:59–67. https://doi.org/10.1016/j.ajo.2020.04.025
Freund KB, Gattoussi S, Leong BCS (2018) Dense B-scan optical coherence tomography angiography. Am J Ophthalmol 190:78–88. https://doi.org/10.1016/j.ajo.2018.03.029
Cohen SY, Dubois L, Nghiem-Buffet S et al (2010) Retinal pseudocysts in age-related geographic atrophy. Am J Ophthalmol 150:211–217.e1. https://doi.org/10.1016/j.ajo.2010.02.019
Abegg M, Dysli M, Wolf S et al (2014) Microcystic macular edema: retrograde maculopathy caused by optic neuropathy. Ophthalmology 121:142–149. https://doi.org/10.1016/j.ophtha.2013.08.045
Gelfand JM, Nolan R, Schwartz DM et al (2012) Microcystic macular oedema in multiple sclerosis is associated with disease severity. Brain 135:1786–1793. https://doi.org/10.1093/brain/aws098
Hilely A, Au A, Freund KB et al (2020) Non-neovascular age-related macular degeneration with subretinal fluid. Br J Ophthalmol bjophthalmol-2020-317326. https://doi.org/10.1136/bjophthalmol-2020-317326
Linsenmeier RA, Zhang HF (2017) Retinal oxygen: from animals to humans. Prog Retin Eye Res 58:115–151. https://doi.org/10.1016/j.preteyeres.2017.01.003
Borrelli E, Shi Y, Uji A et al (2018) Topographic analysis of the choriocapillaris in intermediate age-related macular degeneration. Am J Ophthalmol 196:34–43. https://doi.org/10.1016/j.ajo.2018.08.014
Jackson TL, Danis RP, Goldbaum M et al (2014) Retinal vascular abnormalities in neovascular age-related macular degeneration. Retina (Philadelphia, PA) 34:568–575. https://doi.org/10.1097/IAE.0b013e3182a487be
Spaide RF, Armstrong D, Browne R (2003) Continuing medical education review: choroidal neovascularization in age-related macular degeneration--what is the cause? Retina (Philadelphia, PA) 23:595–614. https://doi.org/10.1097/00006982-200310000-00001
Scharf J, Freund KB, Sadda S, Sarraf D (2020) Paracentral acute middle maculopathy and the organization of the retinal capillary plexuses. Prog Retin Eye Res 100884. https://doi.org/10.1016/j.preteyeres.2020.100884
Fine BS, Zimmerman LE (1962) Muller’s cells and the “middle limiting membrane” of the human retina. An electron microscopic study. Investig Ophthalmol 1:304–326
Tolentino MJ, Miller JW, Gragoudas ES et al (1996) Intravitreous injections of vascular endothelial growth factor produce retinal ischemia and microangiopathy in an adult primate. Ophthalmology 103:1820–1828. https://doi.org/10.1016/s0161-6420(96)30420-x
Querques G, Querques L, Forte R et al (2013) Precursors of type 3 neovascularization: a multimodal imaging analysis. Retina (Philadelphia, PA) 33:1241–1248. https://doi.org/10.1097/IAE.0b013e31827b639e
Dolz-Marco R, Balaratnasingam C, Messinger JD et al (2018) The border of macular atrophy in age-related macular degeneration: a clinicopathologic correlation. Am J Ophthalmol 193:166–177. https://doi.org/10.1016/j.ajo.2018.06.020
Li M, Huisingh C, Messinger J et al (2018) Histology of geographic atrophy secondary to age-related macular degeneration: a multilayer approach. Retina (Philadelphia, Pa) 38:1937–1953. https://doi.org/10.1097/IAE.0000000000002182
Li M, Dolz-Marco R, Messinger JD et al (2018) Clinicopathologic correlation of anti-vascular endothelial growth factor-treated type 3 neovascularization in age-related macular degeneration. Ophthalmology 125:276–287. https://doi.org/10.1016/j.ophtha.2017.08.019
Eichler W, Yafai Y, Wiedemann P, Reichenbach A (2004) Angiogenesis-related factors derived from retinal glial (Müller) cells in hypoxia. Neuroreport 15:1633–1637. https://doi.org/10.1097/01.wnr.0000133071.00786.a4
Yafai Y, Lange J, Wiedemann P et al (2007) Pigment epithelium-derived factor acts as an opponent of growth-stimulatory factors in retinal glial-endothelial cell interactions. Glia 55:642–651. https://doi.org/10.1002/glia.20495
Ou K, Mertsch S, Theodoropoulou S et al (2019) Müller cells stabilize microvasculature through hypoxic preconditioning. Cell Physiol Biochem 52:668–680. https://doi.org/10.33594/000000047
Bringmann A, Wiedemann P (2012) Müller glial cells in retinal disease. Ophthalmologica 227:1–19. https://doi.org/10.1159/000328979
Querques G, Srour M, Massamba N et al (2013) Functional characterization and multimodal imaging of treatment-naive “quiescent” choroidal neovascularization. Invest Ophthalmol Vis Sci 54:6886–6892. https://doi.org/10.1167/iovs.13-11665
de Oliveira Dias JR, Zhang Q, Garcia JMB et al (2018) Natural history of subclinical neovascularization in nonexudative age-related macular degeneration using swept-source OCT angiography. Ophthalmology 125:255–266. https://doi.org/10.1016/j.ophtha.2017.08.030
Chen L, Messinger JD, Sloan KR et al (2020) Nonexudative macular neovascularization supporting outer retina in age-related macular degeneration: a clinicopathologic correlation. Ophthalmology 127:931–947. https://doi.org/10.1016/j.ophtha.2020.01.040
Code availability
Not applicable.
Funding
This work was supported by The Macula Foundation Inc., New York, NY.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K.B. Freund is a consultant for Heidelberg Engineering, Zeiss, Allergan, Regeneron, Bayer, and Novartis. He receives research support from Genentech/Roche. T. Bacci, J.O. Essilfie, and B.C.S. Leong have no disclosures.
Ethics approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Disclaimer
The funders had no role in the study design, collection, analysis and interpretation of data, writing the report, or the decision to submit the report for publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bacci, T., Essilfie, J.O., Leong, B.C.S. et al. Exudative non-neovascular age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 259, 1123–1134 (2021). https://doi.org/10.1007/s00417-020-05021-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-05021-y