Abstract
Background
Patients with anterior circulation ischemic strokes due to large vessel occlusion (AIS-LVO) and very severe neurological deficits (National Institutes of Health Stroke Scale (NIHSS) score > 25) were under-represented in clinical trials on endovascular treatment (EVT). We aimed to evaluate safety and outcomes of EVT in patients with very severe vs. severe (NIHSS score 15–25) neurological deficits.
Methods
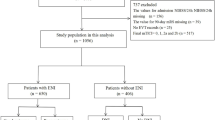
We included consecutive patients undergoing EVT for AIS-LVO between January 2015 and December 2019 at Lille University Hospital. We compared rates of parenchymal hemorrhage (PH), symptomatic intracranial hemorrhage (SICH), procedural complications, and 90-day mortality between patients with very severe vs. severe neurological deficit using univariable and multivariable logistic regression analyses. Functional outcome (90-days modified Rankin Scale) was compared between groups using ordinal logistic regression analysis.
Results
Among 1484 patients treated with EVT, 108 (7%) had pre-treatment NIHSS scores > 25, 873 (59%) with NIHSS scores 15–25 and 503 (34%) with NIHSS scores < 15. Rates of PH, SICH, successful recanalization, and procedural complications were similar in patients with NIHSS scores > 25 and NIHSS 15–25. Patients with NIHSS > 25 had a lower likelihood of improved functional outcome (adjcommon OR 0.31[95% CI 0.21–0.47]) and higher odds of mortality at 90 days (adjOR 2.3 [95% CI 1.5–3.7]) compared to patients with NIHSS 15–25. Successful recanalization was associated with better functional outcome (adjcommon OR 3.8 [95% CI 1.4–10.4]), and lower odds of mortality (adjOR 0.3 [95% CI 0.1–0.9]) in patients with very severe stroke. The therapeutic effect of recanalization on functional outcome and mortality was similar in both groups.
Conclusions
In patients with very severe neurological deficit, EVT was safe and successful recanalization was strongly associated with better functional outcome at 90 days.





Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Turc G, Bhogal P, Fischer U et al (2019) European Stroke Organisation (ESO)- European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg 11:535–538. https://doi.org/10.1136/neurintsurg-2018-014568
Powers WJ, Rabinstein AA, Teri A et al (2019) Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 50:e344–e418. https://doi.org/10.1161/STR.0000000000000211
Bracard S, Ducrocq X, Mas JL et al (2016) Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol 15:1138–1147. https://doi.org/10.1016/S1474-4422(16)30177-6
Saver JL, Goyal M, Bonafe A et al (2015) Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 372:2285–2295. https://doi.org/10.1056/NEJMoa1415061
Goyal M, Menon BK, van Zwam WH et al (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. The Lancet 387:1723–1731. https://doi.org/10.1016/S0140-6736(16)00163-X
Wahlgren N, Ahmed N, Dávalos A et al (2007) Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. Lancet 369:275–282. https://doi.org/10.1016/S0140-6736(07)60149-4
Whiteley WN, Slot KB, Fernandes P et al (2012) Risk factors for intracranial hemorrhage in acute ischemic stroke patients treated with recombinant tissue plasminogen activator: a systematic review and meta-analysis of 55 studies. Stroke 43:2904–2909. https://doi.org/10.1161/STROKEAHA.112.665331
Jiang S, Fei A, Peng Y et al (2015) Predictors of outcome and hemorrhage in patients undergoing endovascular therapy with solitaire stent for acute ischemic stroke. PLoS ONE 10:e0144452. https://doi.org/10.1371/journal.pone.0144452
Kaesmacher J, Kaesmacher M, Maegerlein C et al (2017) Hemorrhagic transformations after thrombectomy: risk factors and clinical relevance. Cerebrovasc Dis 43:294–304. https://doi.org/10.1159/000460265
Leys D, Dequatre-Ponchelle N, Ferrigno M et al (2019) Access to mechanical thrombectomy for cerebral ischaemia: a population-based study in the North-of-France. Rev Neurol (Paris) 175:519–527. https://doi.org/10.1016/j.neurol.2018.12.010
Ducroquet A, Leys D, Al Saabi A et al (2013) Influence of chronic ethanol consumption on the neurological severity in patients with acute cerebral ischemia. Stroke 44:2324–2326. https://doi.org/10.1161/STROKEAHA.113.001355
van Swieten JC, Koudstaal PJ, Visser MC et al (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19:604–607. https://doi.org/10.1161/01.str.19.5.604
Organisation ES, (ESO) Executive Committee, ESO Writing Committee, (2008) Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis 25:457–507. https://doi.org/10.1159/000131083
Albers GW, Marks MP, Kemp S et al (2018) Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 378:708–718. https://doi.org/10.1056/NEJMoa1713973
Nogueira RG, Jadhav AP, Haussen DC et al (2018) Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 378:11–21. https://doi.org/10.1056/NEJMoa1706442
Adams HP, Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41. https://doi.org/10.1161/01.str.24.1.35
Barber PA, Hill MD, Eliasziw M et al (2005) Imaging of the brain in acute ischaemic stroke: comparison of computed tomography and magnetic resonance diffusion-weighted imaging. J Neurol Neurosurg Psychiatry 76:1528–1533. https://doi.org/10.1136/jnnp.2004.059261
von Kummer R, Broderick JP, Campbell BCV et al (2015) The Heidelberg bleeding classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke 46:2981–2986. https://doi.org/10.1161/STROKEAHA.115.010049
Hacke W, Kaste M, Bluhmki E et al (2008) Thrombolysis with Alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 359:1317–1329. https://doi.org/10.1056/NEJMoa0804656
Higashida RT, Furlan AJ (2003) Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke 34:e109–e137. https://doi.org/10.1161/01.STR.0000082721.62796.09
Tomsick T, Broderick J, Carrozella J et al (2008) Revascularization results in the interventional management of stroke II trial. AJNR Am J Neuroradiol 29:582–587. https://doi.org/10.3174/ajnr.A0843
Saver JL (2007) Novel end point analytic techniques and interpreting shifts across the entire range of outcome scales in acute stroke trials. Stroke 38:3055–3062. https://doi.org/10.1161/STROKEAHA.107.488536
Majhadi L, Leys D, Bodenant M et al (2013) Mortality in patients treated by intra-venous thrombolysis for ischaemic stroke. J Neurol 260:1637–1648. https://doi.org/10.1007/s00415-013-6847-9
Mazya MV, Lees KR, Collas D et al (2015) IV thrombolysis in very severe and severe ischemic stroke: results from the SITS-ISTR Registry. Neurology 85:2098–2106. https://doi.org/10.1212/WNL.0000000000002199
Balami JS, White PM, McMeekin PJ et al (2018) Complications of endovascular treatment for acute ischemic stroke: prevention and management. Int J Stroke 13:348–361. https://doi.org/10.1177/1747493017743051
Karen S, Emily A, Marijana L et al (2015) Quality of life and functional outcomes 12 months after out-of-hospital cardiac arrest. Circulation 131:174–181. https://doi.org/10.1161/CIRCULATIONAHA.114.011200
Broderick JP, Berkhemer OA, Palesch YY et al (2015) Endovascular therapy is effective and safe for patients with severe ischemic stroke. Stroke 46:3416–3422. https://doi.org/10.1161/STROKEAHA.115.011397
Funding
The authors received no financial support for the research, authorship, and publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no competing interest concerning this manuscript.
Ethical approval
The registry was approved by the relevant ethical committee (Comité de Protection des Personnes Nord Ouest IV Lille, France, March 9th, 2010, registration number 10.677). Patients were managed according to local rules without any investigation or treatment specifically performed for the purpose of this study. Patients gave consent themselves or via a close relative for the follow-up.
Rights and permissions
About this article
Cite this article
Bala, F., Bricout, N., Nouri, N. et al. Safety and outcomes of endovascular treatment in patients with very severe acute ischemic stroke. J Neurol 269, 2493–2502 (2022). https://doi.org/10.1007/s00415-021-10807-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-021-10807-z