Abstract
Background and purpose
To investigate the retina thickness assessed using optical coherence tomography in atypical parkinsonism in comparison with health controls (HC) and patients with Parkinson’s disease (PD).
Methods
PubMed and EMBASE were searched for potentially eligible studies that reported retina thickness in atypical parkinsonism
[including progressive supranuclear palsy (PSP), multiple system atrophy (MSA) and corticobasal degeneration] in comparison with that of HC and PD patients from their dates of inception to Jan 24, 2021. Mean difference (μm) of the thickness of peripapillary retinal nerve fiber layer (pRNFL) and central macular thickness (CMT) were pooled with random effects model.
Results
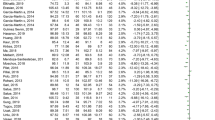
We included ten studies eligible for inclusion criteria. Average pRNFL thickness and average CMT were thinner in PSP [pooled mean difference (μm) of − 4.71, 95% CI (− 7.15, − 2.27); − 15.12, 95% CI (− 16.93, − 13.30)] and in MSA [− 5.37, 95% CI (− 6.59, − 4.15); − 5.93, 95% CI (− 11.00, − 0.87)] compared with HC, and were thinner in PSP [− 5.81, 95% CI (− 8.92, − 2.69); − 10.63, 95% CI (− 20.29, − 0.98)] and in MSA [− 0.35 μm, 95% CI (− 5.72, 5.01); − 7.42 μm [95% CI (− 12.46, − 2.38)] compared with PD. The pRNFL thickness was thinning in superior, inferior and nasal quadrants, and CMT was thinning in outer sectors in MSA compared with HC.
Conclusions
The retina thickness was significantly thinner in PSP and MSA than those in HC and PD. The specific patterns of retina thinning in MSA could be clinical importance for differentiation among atypical parkinsonism.





Similar content being viewed by others
Data availability
The data relative to the study are available from the corresponding author upon reasonable request.
References
Koziorowski D, Figura M, Milanowski ŁM et al (2021) Mechanisms of neurodegeneration in various forms of parkinsonism-similarities and differences. Cells 10:656
Fanciulli A, Wenning GK (2015) Multiple-system atrophy. N Engl J Med 372:249–263
Beyer K, Ariza A (2007) Protein aggregation mechanisms in synucleinopathies: commonalities and differences. J Neuropathol Exp Neurol 66:965–974
Low PA, Reich SG, Jankovic J et al (2015) Natural history of multiple system atrophy in the USA: a prospective cohort study. Lancet Neurol 14:710–719
Wenning GK, Geser F, Krismer F et al (2013) The natural history of multiple system atrophy: a prospective European cohort study. Lancet Neurol 12:264–274
Respondek G, Levin J, Höglinger GU (2018) Progressive supranuclear palsy and multiple system atrophy: clinicopathological concepts and therapeutic challenges. Curr Opin Neurol 31:448–454
Mendoza-Santiesteban CE, Palma JA, Ortuño-Lizarán I, Cuenca N, Kaufmann H (2017) Pathologic confirmation of retinal ganglion cell loss in multiple system atrophy. Neurology 88:2233–2235
Dickson DW, Ahmed Z, Algom AA, Tsuboi Y, Josephs KA (2010) Neuropathology of variants of progressive supranuclear palsy. Curr Opin Neurol 23:394–400
Boxer AL, Yu JT, Golbe LI, Litvan I, Lang AE, Höglinger GU (2017) Advances in progressive supranuclear palsy: new diagnostic criteria, biomarkers, and therapeutic approaches. Lancet Neurol 16:552–563
Stemplewitz B, Kromer R, Vettorazzi E, Hidding U, Frings A, Buhmann C (2017) Retinal degeneration in progressive supranuclear palsy measured by optical coherence tomography and scanning laser polarimetry. Sci Rep 7:5357
Dickson DW, Bergeron C, Chin SS et al (2002) Office of Rare diseases neuropathologic criteria for corticobasal degeneration. J Neuropathol Exp Neurol 61:935–946
Valentino RR, Koga S, Walton RL et al (2020) MAPT subhaplotypes in corticobasal degeneration: assessing associations with disease risk, severity of tau pathology, and clinical features. Acta Neuropathol Commun 8:218
Bak TH, Caine D, Hearn VC, Hodges JR (2006) Visuospatial functions in atypical Parkinsonian syndromes. J Neurol Neurosurg Psychiatry 77:454–456
Wang L, Kuroiwa Y, Kamitani T et al (2000) Visual event-related potentials in progressive supranuclear palsy, corticobasal degeneration, striatonigral degeneration, and Parkinson’s disease. J Neurol 247:356–363
Miller N, Drachman DA (2006) The optic nerve: a window into diseases of the brain? Neurology 67:1742–1743
Huang D, Swanson EA, Lin CP et al (1991) Optical coherence tomography. Science 254:1178–1181
Albrecht P, Müller AK, Südmeyer M et al (2012) Optical coherence tomography in parkinsonian syndromes. PLoS ONE 7:e34891
Alkabie S, Lange A, Manogaran P, Stoessl AJ, Costello F, Barton JJS (2020) Optical coherence tomography of patients with Parkinson’s disease and progressive supranuclear palsy. Clin Neurol Neurosurg 189:105635
Gulmez Sevim D, Unlu M, Gultekin M, Karaca C, Mirza M, Mirza GE (2018) Evaluation of retinal changes in progressive supranuclear palsy and Parkinson Disease. J Neuroophthalmol 38:151–155
Pula JH, Towle VL, Staszak VM, Cao D, Bernard JT, Gomez CM (2011) Retinal nerve fibre layer and macular thinning in spinocerebellar ataxia and cerebellar multisystem atrophy. Neuroophthalmology 35:108–114
Fischer MD, Synofzik M, Heidlauf R et al (2011) Retinal nerve fiber layer loss in multiple system atrophy. Mov Disord 26:914–916
Fischer MD, Synofzik M, Kernstock C et al (2013) Decreased retinal sensitivity and loss of retinal nerve fibers in multiple system atrophy. Graefes Arch Clin Exp Ophthalmol 251:235–241
Ahn J, Lee JY, Kim TW (2016) Retinal thinning correlates with clinical severity in multiple system atrophy. J Neurol 263:2039–2047
Shamseer L, Moher D, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 350:g7647
Higgins JPT, Green S (2011) Cochrane Handbook for systematic reviews of interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, www.cochrane-handbook.org.
Huang L, Wang C, Wang W, Wang Y, Zhang R (2020) The specific pattern of retinal nerve fiber layer thinning in Parkinson’s disease: a systematic review and meta-analysis. J Neurol. https://doi.org/10.1007/s00415-020-10094-0
Huang L, Zhang D, Ji J, Wang Y, Zhang R (2020) Central retina changes in Parkinson’s disease: a systematic review and meta-analysis. J Neurol. https://doi.org/10.1007/s00415-020-10304-9
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605
Cruz-Herranz A, Balk LJ, Oberwahrenbrock T et al (2016) The APOSTEL recommendations for reporting quantitative optical coherence tomography studies. Neurology 86:2303–2309
Schneider M, Müller HP, Lauda F et al (2014) Retinal single-layer analysis in Parkinsonian syndromes: an optical coherence tomography study. J Neural Transm (Vienna) 121:41–47
Mendoza-Santiesteban CE, Palma JA, Martinez J, Norcliffe-Kaufmann L, Hedges TR 3rd, Kaufmann H (2015) Progressive retinal structure abnormalities in multiple system atrophy. Mov Disord 30:1944–1953
Gilman S, Wenning GK, Low PA et al (2008) Second consensus statement on the diagnosis of multiple system atrophy. Neurology 71:670–676
Delalande I, Hache JC, Forzy G, Bughin M, Benhadjali J, Destée A (1998) Do visual-evoked potentials and spatiotemporal contrast sensitivity help to distinguish idiopathic Parkinson’s disease and multiple system atrophy? Mov Disord 13:446–4452
Sartucci F, Orlandi G, Bonuccelli U et al (2006) Chromatic pattern-reversal electroretinograms (ChPERGs) are spared in multiple system atrophy compared with Parkinson’s disease. Neurol Sci 26:395–401
Kolb H (2012) Simple anatomy of the retina, In: Kolb H, Fernandez E, Nelson R, (Eds), Webvision: The Organization of the Retina and Visual System. Salt Lake City, UT: University of Utah Health Sciences Center; 1995–2005 [updated 2012 Jan 31]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/21413391
Ahmed Z, Asi YT, Sailer A et al (2012) The neuropathology, pathophysiology and genetics of multiple system atrophy. Neuropathol Appl Neurobiol 38:4–24
Satue M, Rodrigo MJ, Obis J et al (2017) Evaluation of progressive visual dysfunction and retinal degeneration in patients With Parkinson’s Disease. Invest Ophthalmol Vis Sci 58:1151–1157
Ho WL, Leung Y, Tsang AW, So KF, Chiu K, Chang RC (2012) Review: tauopathy in the retina and optic nerve: does it shadow pathological changes in the brain? Mol Vis 18:2700–2710
Kovacs GG, Lukic MJ, Irwin DJ et al (2020) Distribution patterns of tau pathology in progressive supranuclear palsy. Acta Neuropathol 140:99–119
Sung KR, Wollstein G, Bilonick RA et al (2009) Effects of age on optical coherence tomography measurements of healthy retinal nerve fiber layer, macula, and optic nerve head. Ophthalmology 116:1119–1124
Jabbari E, Holland N, Chelban V et al (2020) Diagnosis across the spectrum of progressive supranuclear palsy and corticobasal syndrome. JAMA Neurol 77:377–387
Schrag A, Ben-Shlomo Y, Quinn N (2002) How valid is the clinical diagnosis of Parkinson’s disease in the community? J Neurol Neurosurg Psychiatry 73:529–534
Wermuth L, Lassen CF, Himmerslev L, Olsen J, Ritz B (2012) Validation of hospital register-based diagnosis of Parkinson’s disease. Dan Med J 59:A4391
Murueta-Goyena A, Del Pino R, Galdós M et al (2021) Retinal thickness predicts the risk of cognitive decline in Parkinson Disease. Ann Neurol 89:165–176
Miki Y, Tsushima E, Foti SC et al (2021) Identification of multiple system atrophy mimicking Parkinson’s disease or progressive supranuclear palsy. Brain 144:1138–1151
Miki Y, Foti SC, Asi YT et al (2019) Improving diagnostic accuracy of multiple system atrophy: a clinicopathological study. Brain 142:2813–2827
Joutsa J, Gardberg M, Röyttä M, Kaasinen V (2014) Diagnostic accuracy of parkinsonism syndromes by general neurologists. Parkinsonism Relat Disord 20:840–844
Funding
No.
Author information
Authors and Affiliations
Contributions
RJZ and YJW contributed to the study conception and design. RJZ and YJW did the systematic literature search, selected studies for inclusion, extracted data, and statistical analyses, made figures. XLM, NW, RJZ and YJW interpreted data. YJW, RJZ, XLM wrote the first draft of the manuscript. All authors revised the manuscript for important intellectual content, approved the final draft.
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no conflicts of interest or no disclosures relevant to the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ma, X., Wang, Y., Wang, N. et al. Retina thickness in atypical parkinsonism: a systematic review and meta-analysis. J Neurol 269, 1272–1281 (2022). https://doi.org/10.1007/s00415-021-10703-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-021-10703-6