Abstract
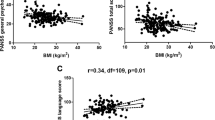
There is increasing evidence that sex differences exist in many clinical manifestations of patients with schizophrenia, including suicidal ideation (SI) and neurocognitive function. The present study was performed to explore the sex differences in the association between SI and neurocognitive function in Chinese patients with schizophrenia. A total of 1188 inpatients with schizophrenia were recruited from multicenter psychiatric hospitals. The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) was utilized to evaluate the neurocognitive function of all patients. The Positive and Negative Syndrome Scale (PANSS) was utilized to assess the psychopathology of patients. The Beck Scale for Suicide Ideation (BSSI) was used to assess the severity of SI. In male patients, the suicide risk score was significantly associated with PANSS negative symptoms (r = 0.167, p = 0.043), visuospatial subscale (r = − 0.261, p = 0.001), and RBANS total scores (r = − 0.172, p = 0.037). Furthermore, multivariate linear regression analysis showed that the visuospatial subscale (β = − 0.490, t = − 3.273, p = 0.001) was independently associated with the suicide risk score in male patients. In female patients, the suicide risk score was significantly correlated with PANSS positive symptoms (r = 0.249, p = 0.021), negative symptoms (r = 0.394, p < 0.001), general psychopathology (r = 0.276, p = 0.01) and PANSS total score (r = 0.365, p = 0.001). Multivariate linear regression analysis showed that PANSS negative symptoms (β = 1.849, t = 3.933, p = 0.001) were significantly associated with suicide risk scores in female patients. Our findings indicate that there are sex differences in the association between SI and neurocognitive function in patients with schizophrenia. Based on the findings of our study, gender-specific prevention and intervention strategies may make a difference in reducing SI in Chinese schizophrenia patients.
Similar content being viewed by others
Data availability
The authors declare that data would be available on request from the authors.
References
Sher L, Kahn RS (2019) Suicide in schizophrenia: an educational overview. Medicina (Kaunas) 55(7):361
Crump C, Winkleby MA, Sundquist K, Sundquist J (2013) Comorbidities and mortality in persons with schizophrenia: a Swedish national cohort study. Am J Psychiatry 170(3):324–333
Saha S, Chant D, McGrath J (2007) A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry 64(10):1123–1131
Laursen TM, Munk-Olsen T, Vestergaard M (2012) Life expectancy and cardiovascular mortality in persons with schizophrenia. Curr Opin Psychiatry 25(2):83–88
Bushe CJ, Taylor M, Haukka J (2010) Mortality in schizophrenia: a measurable clinical endpoint. J psychopharmacol (Oxford, England) 24(4 Suppl):17–25
Hubers AAM, Moaddine S, Peersmann SHM, Stijnen T, van Duijn E, van der Mast RC et al (2018) Suicidal ideation and subsequent completed suicide in both psychiatric and non-psychiatric populations: a meta-analysis. Epidemiol Psychiatric Sci 27(2):186–198
Bai W, Liu ZH, Jiang YY, Zhang QE, Rao WW, Cheung T et al (2021) Worldwide prevalence of suicidal ideation and suicide plan among people with schizophrenia: a meta-analysis and systematic review of epidemiological surveys. Transl Psychiatry 11(1):552
Hor K, Taylor M (2010) Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol (Oxford, England) 24(4 Suppl):81–90
Masedo Gutiérrez AI, Grandón Fernández P, Bustos C, Moreno-Küstner B (2017) Considerations about the assessment of stigma towards persons with schizophrenia: the question of gender. Asian J Psychiatr 28:148–149
Zhu MH, Liu ZJ, Hu QY, Yang JY, Jin Y, Zhu N et al (2022) Amisulpride augmentation therapy improves cognitive performance and psychopathology in clozapine-resistant treatment-refractory schizophrenia: a 12-week randomized, double-blind, placebo-controlled trial. Mil Med Res 9(1):59
Huang Y, Wu K, Jiang R, Zeng X, Zhou S, Guo W et al (2021) Suicide attempts, neurocognitive dysfunctions and clinical correlates in middle-aged and elderly chinese schizophrenia patients. Front Psych 12:684653
Delaney C, McGrane J, Cummings E, Morris DW, Tropea D, Gill M et al (2012) Preserved cognitive function is associated with suicidal ideation and single suicide attempts in schizophrenia. Schizophr Res 140(1–3):232–236
Villa J, Choi J, Kangas JL, Kaufmann CN, Harvey PD, Depp CA (2018) Associations of suicidality with cognitive ability and cognitive insight in outpatients with Schizophrenia. Schizophr Res 192:340–344
Fernández-Sevillano J, González-Pinto A, Rodríguez-Revuelta J, Alberich S, Gónzalez-Blanco L, Zorrilla I et al (2021) Suicidal behaviour and cognition: a systematic review with special focus on prefrontal deficits. J Affect Disord 278:488–496
Tarrier N, Kelly J, Maqsood S, Snelson N, Maxwell J, Law H et al (2014) The cognitive behavioural prevention of suicide in psychosis: a clinical trial. Schizophr Res 156(2–3):204–210
Barrett EA, Sundet K, Simonsen C, Agartz I, Lorentzen S, Mehlum L et al (2011) Neurocognitive functioning and suicidality in schizophrenia spectrum disorders. Compr Psychiatry 52(2):156–163
Li Z, Liu X, Xu H, Zhao L, Zhou Y, Wu X et al (2021) Sex difference in comorbid depression in first-episode and drug-naive patients with schizophrenia: baseline results from the depression in schizophrenia in China Study. Psychosom Med 83(9):1082–1088
Zhou Y, Song X, Guo Y, Lang X, Li Z, Zhang XY (2021) Sex differences in metabolic disorder patterns of first-episode drug-naive patients with schizophrenia. Psychoneuroendocrinology 124:105061
Zhu M, Liu Z, Guo Y, Sultana MS, Wu K, Lang X et al (2021) Sex difference in the interrelationship between TNF-α and oxidative stress status in first-episode drug-naïve schizophrenia. J Neuroinflammation 18(1):202
Huang X, Bao C, Lv Q, Zhao J, Wang Y, Lang X et al (2020) Sex difference in cognitive impairment in drug-free schizophrenia: association with miR-195 levels. Psychoneuroendocrinology 119:104748
Clapham E, Bodén R, Brandt L, Jönsson EG, Bahmanyar S, Ekbom A et al (2019) Suicide ideation and behavior as risk factors for subsequent suicide in schizophrenia: a nested case-control study. Suicide Life Threat Behav 49(4):996–1005
Dong M, Wang SB, Wang F, Zhang L, Ungvari GS, Ng CH et al (2019) Suicide-related behaviours in schizophrenia in China: a comprehensive meta-analysis. Epidemiol Psychiatric Sci 28(3):290–299
Denney JT, Rogers RG, Krueger PM, Wadsworth T (2009) Adult suicide mortality in the United States: marital status, family size, socioeconomic status, and differences by sex. Soc Sci Q 90(5):1167
Brébion G, Stephan-Otto C, Ochoa S, Nieto L, Contel M, Usall J (2018) Verbal fluency in male and female schizophrenia patients: Different patterns of association with processing speed, working memory span, and clinical symptoms. Neuropsychology 32(1):65–76
Leger M, Neill JC (2016) A systematic review comparing sex differences in cognitive function in schizophrenia and in rodent models for schizophrenia, implications for improved therapeutic strategies. Neurosci Biobehav Rev 68:979–1000
Mendrek A, Mancini-Marïe A (2016) Sex/gender differences in the brain and cognition in schizophrenia. Neurosci Biobehav Rev 67:57–78
Ko YS, Tsai HC, Chi MH, Su CC, Lee IH, Chen PS et al (2018) Higher mortality and years of potential life lost of suicide in patients with schizophrenia. Psychiatry Res 270:531–537
Fuller-Thomson E, Hollister B (2016) Schizophrenia and suicide attempts: findings from a representative community-based canadian sample. Schizophr Res Treat 2016:3165243
Pu C, Qiu Y, Zhou T, Yang F, Lu Z, Wang C et al (2019) Gender differences of neurocognitive functioning in patients with first-episode schizophrenia in China. Compr Psychiatry 95:152132
Ittig S, Studerus E, Papmeyer M, Uttinger M, Koranyi S, Ramyead A et al (2015) Sex differences in cognitive functioning in at-risk mental state for psychosis, first episode psychosis and healthy control subjects. Eur Psychiatry 30(2):242–250
Hamson DK, Roes MM, Galea LA (2016) Sex hormones and cognition: neuroendocrine influences on memory and learning. Compr Physiol 6(3):1295–1337
Kay SR, Fiszbein A, Opler LA (1987) The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13(2):261–276
Beck AT, Kovacs M, Weissman A (1979) Assessment of suicidal intention: the scale for suicide ideation. J Consult Clin Psychol 47(2):343–352
Zhang J, Lester D, Zhao S, Zhou C (2013) Suicidal ideation and its correlates: testing the interpersonal theory of suicide in Chinese students. Arch Suicide Res 17(3):236–241
Turecki G, Brent DA, Gunnell D, O’Connor RC, Oquendo MA, Pirkis J et al (2019) Suicide and suicide risk. Nat Rev Dis Primers 5(1):74
Beautrais AL (2003) Understanding suicidal behaviour: the suicidal process approach to research, treatment and prevention. Aust N Z J Psychiatry 37(1):128–129
Zhang BH, Tan YL, Zhang WF, Wang ZR, Zhou DF (2008) Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) as a screening test in Chinese: reliability and validity. Chin Ment Health J 22(12):865–869
Zhu R, Wang D, Tian Y, Du Y, Chen J, Zhou H et al (2022) Sex difference in association between insomnia and cognitive impairment in patients with chronic schizophrenia. Schizophr Res 240:143–149
Roesch-Ely D, Hornberger E, Weiland S, Hornstein C, Parzer P, Thomas C et al (2009) Do sex differences affect prefrontal cortex associated cognition in schizophrenia? Schizophr Res 107(2–3):255–261
Zhang B, Han M, Tan S, De Yang F, Tan Y, Jiang S et al (2017) Gender differences measured by the MATRICS consensus cognitive battery in chronic schizophrenia patients. Sci Rep 7(1):11821
Zhao N, Wang XH, Kang CY, Zheng Y, Yang LY, Guan TF et al (2021) Sex differences in association between cognitive impairment and clinical correlates in Chinese patients with first-episode drug-naïve schizophrenia. Ann Gen Psychiatry 20(1):26
Dong R, Zhao NO, Wu HE, Yu L, Zhang XY (2021) Sex differences in the association between serum BDNF and cognitive impairment in schizophrenia patients using various antipsychotics. J Psychiatr Res 138:492–499
Wei CW, Chen YQ, Ma M, Xiu MH, Zhang XY (2020) Sex differences in the association of body mass index with symptoms and cognitive deficits in Chinese patients with chronic schizophrenia. Transl Psychiatry 10(1):18
Han M, Huang XF, Chen DC, Xiu MH, Hui L, Liu H et al (2012) Gender differences in cognitive function of patients with chronic schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 39(2):358–363
Koolschijn PC, Crone EA (2013) Sex differences and structural brain maturation from childhood to early adulthood. Dev Cogn Neurosci 5:106–118
Jollant F, Bellivier F, Leboyer M, Astruc B, Torres S, Verdier R et al (2005) Impaired decision making in suicide attempters. Am J Psychiatry 162(2):304–310
McGirr A, Dombrovski AY, Butters MA, Clark L, Szanto K (2012) Deterministic learning and attempted suicide among older depressed individuals: cognitive assessment using the Wisconsin card sorting task. J Psychiatr Res 46(2):226–232
Bredemeier K, Miller IW (2015) Executive function and suicidality: a systematic qualitative review. Clin Psychol Rev 40:170–183
Davis RN, Nolen-Hoeksema S (2000) Cognitive inflexibility among ruminators and nonruminators. Cogn Ther Res 24(6):699–711
Donohoe G, Hayden J, McGlade N, O’Gráda C, Burke T, Barry S et al (2009) Is “clinical” insight the same as “cognitive” insight in schizophrenia? J Int Neuropsychol Soc 15(3):471–475
Crumlish N, Whitty P, Kamali M, Clarke M, Browne S, McTigue O et al (2005) Early insight predicts depression and attempted suicide after 4 years in first-episode schizophrenia and schizophreniform disorder. Acta Psychiatr Scand 112(6):449–455
Amore M, Murri MB, Calcagno P, Rocca P, Rossi A, Aguglia E et al (2020) The association between insight and depressive symptoms in schizophrenia: undirected and Bayesian network analyses. Eur Psychiatry 63(1):1–21
Lien YJ, Chang HA, Kao YC, Tzeng NS, Yeh CB, Loh CH (2018) Self-stigma mediates the impact of insight on current suicide ideation in suicide attempters with schizophrenia: results of a moderated mediation approach. Suicide Life Threat Behav 48(6):661–676
Verma D, Srivastava MK, Singh SK, Bhatia T, Deshpande SN (2016) Lifetime suicide intent, executive function and insight in schizophrenia and schizoaffective disorders. Schizophr Res 178(1–3):12–16
Potkin SG, Anand R, Alphs L, Fleming K (2003) Neurocognitive performance does not correlate with suicidality in schizophrenic and schizoaffective patients at risk for suicide. Schizophr Res 59(1):59–66
MacLusky NJ, Hajszan T, Prange-Kiel J, Leranth C (2006) Androgen modulation of hippocampal synaptic plasticity. Neuroscience 138(3):957–965
Martin SJ, Grimwood PD, Morris RG (2000) Synaptic plasticity and memory: an evaluation of the hypothesis. Annu Rev Neurosci 23:649–711
Beauchet O (2006) Testosterone and cognitive function: current clinical evidence of a relationship. Eur J Endocrinol 155(6):773–781
Moffat SD (2005) Effects of testosterone on cognitive and brain aging in elderly men. Ann N Y Acad Sci 1055:80–92
Tan S, Sohrabi HR, Weinborn M, Tegg M, Bucks RS, Taddei K et al (2019) Effects of testosterone supplementation on separate cognitive domains in cognitively healthy older men: a meta-analysis of current randomized clinical trials. Am J Geriatr Psychiatry 27(11):1232–1246
Moore L, Kyaw M, Vercammen A, Lenroot R, Kulkarni J, Curtis J et al (2013) Serum testosterone levels are related to cognitive function in men with schizophrenia. Psychoneuroendocrinology 38(9):1717–1728
Cherrier MM, Matsumoto AM, Amory JK, Asthana S, Bremner W, Peskind ER et al (2005) Testosterone improves spatial memory in men with Alzheimer disease and mild cognitive impairment. Neurology 64(12):2063–2068
Tripodianakis J, Markianos M, Rouvali O, Istikoglou C (2007) Gonadal axis hormones in psychiatric male patients after a suicide attempt. Eur Arch Psychiatry Clin Neurosci 257(3):135–139
Duca Y, Aversa A, Condorelli RA, Calogero AE, La Vignera S (2019) Substance abuse and male hypogonadism. J clin Med 8(5):732
Sher L (2012) Testosterone and suicidal behavior. Expert Rev Neurother 12(3):257–259
Lundh LG, Simonsson-Sarnecki M (2001) Alexithymia, emotion, and somatic complaints. J Pers 69(3):483–510
Koh KB, Kim DK, Kim SY, Park JK, Han M (2008) The relation between anger management style, mood and somatic symptoms in anxiety disorders and somatoform disorders. Psychiatry Res 160(3):372–379
Zhou X, Peng Y, Zhu X, Yao S, Dere J, Chentsova-Dutton YE et al (2016) From culture to symptom: testing a structural model of “Chinese somatization.” Transcult Psychiatry 53(1):3–23
Player MJ, Proudfoot J, Fogarty A, Whittle E, Spurrier M, Shand F et al (2015) What interrupts suicide attempts in men: a qualitative study. PLoS ONE 10(6):e0128180
Chang Q, Wu D, Rong H, Wu Z, Tao W, Liu H et al (2019) Suicide ideation, suicide attempts, their sociodemographic and clinical associates among the elderly Chinese patients with schizophrenia spectrum disorders. J Affect Disord 256:611–617
Tarrier N, Gooding P, Gregg L, Johnson J, Drake R (2007) Suicide schema in schizophrenia: the effect of emotional reactivity, negative symptoms and schema elaboration. Behav Res Ther 45(9):2090–2097
Segalovich J, Doron A, Behrbalk P, Kurs R, Romem P (2013) Internalization of stigma and self-esteem as it affects the capacity for intimacy among patients with schizophrenia. Arch Psychiatr Nurs 27(5):231–234
Kring AM, Elis O (2013) Emotion deficits in people with schizophrenia. Annu Rev Clin Psychol 9:409–433
Corrigan PW, Rao D (2012) On the self-stigma of mental illness: stages, disclosure, and strategies for change. Can J Psychiatry 57(8):464–469
Baca-García E, Diaz-Sastre C, Ceverino A, Saiz-Ruiz J, Diaz FJ, de Leon J (2003) Association between the menses and suicide attempts: a replication study. Psychosom Med 65(2):237–244
Baca-Garcia E, Diaz-Sastre C, Ceverino A, Perez-Rodriguez MM, Navarro-Jimenez R, Lopez-Castroman J et al (2010) Suicide attempts among women during low estradiol/low progesterone states. J Psychiatr Res 44(4):209–214
Saunders KE, Hawton K (2006) Suicidal behaviour and the menstrual cycle. Psychol Med 36(7):901–912
McGregor C, Riordan A, Thornton J (2017) Estrogens and the cognitive symptoms of schizophrenia: possible neuroprotective mechanisms. Front Neuroendocrinol 47:19–33
Farage MA, Osborn TW, MacLean AB (2008) Cognitive, sensory, and emotional changes associated with the menstrual cycle: a review. Arch Gynecol Obstet 278(4):299–307
Hoff AL, Kremen WS, Wieneke MH, Lauriello J, Blankfeld HM, Faustman WO et al (2001) Association of estrogen levels with neuropsychological performance in women with schizophrenia. Am J Psychiatry 158(7):1134–1139
Acknowledgements
Thank you to all the participants.
Funding
This study was funded by the Science and Technology Program of Guangzhou (202206060005, 202201010093, 2023A03J0856, 2023A03J0839), Guangdong Basic and Applied Basic Research Foundation Outstanding Youth Project (2021B1515020064), Medical Science and Technology Research Foundation of Guangdong (A2023224), the Natural Science Foundation Program of Guangdong (2023A1515011383), the Health Science and Technology Program of Guangzhou(20231A010036), Guangzhou Municipal Key Discipline in Medicine (2021-2023), Guangzhou High-level Clinical Key Specialty and Guangzhou Research-oriented Hospital.The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
XZ, FW, ZL and YH designed the study. HL, YF, SF, SZ screened the pateints and collected the data. YL, QC, LL and HY collected the literatures and cleaned the data. FW and YY performed the statistical analysis. FW, YY, YH, ZL and XZ wrote the manuscript. All authors discussed the results and reviewed the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The author(s) declare that they have no competing interests.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, F., Yi, Y., Lian, Y. et al. Sex differences in the association between suicidal ideation and neurocognitive function in Chinese patients with schizophrenia. Eur Arch Psychiatry Clin Neurosci (2023). https://doi.org/10.1007/s00406-023-01616-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00406-023-01616-8