Abstract
Background
Lateral lymph node metastasis (LLNM) is associated with poor prognosis in patients with papillary thyroid cancer (PTC). The purpose of this study was to determine the risk factors for LLNM and establish prediction models that could individually assessed the risk of LLNM.
Methods
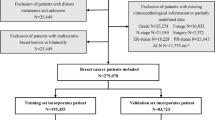
A total of 619 PTC patients were retrospectively analyzed in our study. Univariate and multivariate analysis were performed for male and female patients, respectively, to assess relationships between clinicopathological features and LLNM. By integrating independent predictors selected by binary logistic regression modeling, preoperative and postoperative nomograms were developed to estimate the risk of LLNM.
Results
LLNM was detected in 80 of 216 male patients. Of 403 female patients, 114 had LLNM. The preoperative nomogram of male patients included three clinical variables: the number of foci, tuner size, and echogenic foci. In addition to the above three variables, the postoperative nomogram of male patients included extrathyroidal extension (ETE) detected in surgery, central lymph node metastasis (CLNM) and high-volume CLNM. The preoperative nomogram of female patients included the following variables: age, chronic lymphocytic thyroiditis (CLT), BRAF V600E, the number of foci, tumor size and echogenic foci. Variables such as CLT, BRAF V600E, the number of foci, tumor size, ETE detected in surgery, CLNM, high-volume CLNM and central lymph node ratio were included in the postoperative nomogram. Above Nomograms show good discrimination.
Conclusions
Considering the difference in the incidence rate of LLNM between men and women, a separate prediction system should be established for patients of different genders. These nomograms are helpful in promoting the risk stratification of PTC treatment decision-making and postoperative management.




Similar content being viewed by others
Data availability statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
Liu S, Liu C, Zhao L et al (2021) A prediction model incorporating the BRAF(V600E) protein status for determining the risk of cervical lateral lymph node metastasis in papillary thyroid cancer patients with central lymph node metastasis. Eur J Surg Oncol 47(11):2774–2780
Hei H, Song Y, Qin J (2019) Individual prediction of lateral neck metastasis risk in patients with unifocal papillary thyroid carcinoma. Eur J Surg Oncol 45(6):1039–1045
Dong W, Horiuchi K, Tokumitsu H et al (2019) Time-varying pattern of mortality and recurrence from papillary thyroid cancer: lessons from a long-term follow-up. Thyroid 29(6):802–808
Suh YJ, Kwon H, Kim SJ et al (2015) Factors affecting the locoregional recurrence of conventional papillary thyroid carcinoma after surgery: a retrospective analysis of 3381 patients. Ann Surg Oncol 22(11):3543–3549
Haugen BR, Alexander EK, Bible KC et al (2016) 2015 American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26(1):1–133
Lim YS, Lee JC, Lee YS et al (2011) Lateral cervical lymph node metastases from papillary thyroid carcinoma: predictive factors of nodal metastasis. Surgery 150(1):116–121
Alabousi M, Alabousi A, Adham S et al (2022) Diagnostic test accuracy of ultrasonography vs computed tomography for papillary thyroid cancer cervical lymph node metastasis: a systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg 148(2):107–118
Xu SY, Yao JJ, Zhou W et al (2019) Clinical characteristics and ultrasonographic features for predicting central lymph node metastasis in clinically node-negative papillary thyroid carcinoma without capsule invasion. Head Neck 41(11):3984–3991
Li F, Pan D, He Y et al (2020) Using ultrasound features and radiomics analysis to predict lymph node metastasis in patients with thyroid cancer. BMC Surg 20(1):315
Grani G, Carbotta G, Nesca A et al (2015) A comprehensive score to diagnose Hashimoto’s thyroiditis: a proposal. Endocrine 49(2):361–365
Gršić K, Bumber B, CurićRadivojević R et al (2020) Prophylactic central neck dissection in well-differentiated thyroid cancer. Acta Clin Croat 59(Suppl 1):87–95
Song Y, Xu G, Wang T et al (2022) Indications of superselective neck dissection in patients with lateral node metastasis of papillary thyroid carcinoma. Otolaryngol Head Neck Surg 166(5):832–839
Carmel-Neiderman NN, Duek I, Amsterdam D et al (2020) Total thyroidectomy with therapeutic level II–IV neck dissection for papillary thyroid carcinoma: level VI recurrence patterns. Eur Arch Otorhinolaryngol 277(12):3449–3455
Ye L, Hu L, Liu W et al (2021) Capsular extension at ultrasound is associated with lateral lymph node metastasis in patients with papillary thyroid carcinoma: a retrospective study. BMC Cancer 21(1):1250
Frasoldati A, Toschi E, Zini M et al (1999) Role of thyroglobulin measurement in fine-needle aspiration biopsies of cervical lymph nodes in patients with differentiated thyroid cancer. Thyroid 9(2):105–111
Cañadas-Garre M, Becerra-Massare P, López-de-la-Torre-Casares M et al (2012) Reduction of false-negative papillary thyroid carcinomas by the routine analysis of BRAF(T1799A) mutation on fine-needle aspiration biopsy specimens: a prospective study of 814 thyroid FNAB patients. Ann Surg 255(5):986–992
So YK, Kim MJ, Kim S et al (2018) Lateral lymph node metastasis in papillary thyroid carcinoma: a systematic review and meta-analysis for prevalence, risk factors, and location. Int J Surg 50:94–103
Zhang X, Zhang L, Xue S et al (2019) Predictive factors of lateral lymph node metastasis in solitary papillary thyroid microcarcinoma without gross extrathyroidal extension. Asian J Surg 42(4):563–570
Nixon IJ, Kuk D, Wreesmann V et al (2016) Defining a valid age cutoff in staging of well-differentiated thyroid cancer. Ann Surg Oncol 23(2):410–415
Zhang L, Wei WJ, Ji QH et al (2012) Risk factors for neck nodal metastasis in papillary thyroid microcarcinoma: a study of 1066 patients. J Clin Endocrinol Metab 97(4):1250–1257
Wang W, Wang H, Teng X et al (2010) Clonal analysis of bilateral, recurrent, and metastatic papillary thyroid carcinomas. Hum Pathol 41(9):1299–1309
Zhu F, Shen YB, Li FQ et al (2016) The effects of hashimoto thyroiditis on lymph node metastases in unifocal and multifocal papillary thyroid carcinoma: a retrospective Chinese cohort study. Medicine (Baltimore) 95(6):e2674
Ieni A, Vita R, Magliolo E et al (2017) One-third of an archivial series of papillary thyroid cancer (years 2007–2015) has coexistent chronic lymphocytic thyroiditis, which is associated with a more favorable tumor-node-metastasis staging. Front Endocrinol (Lausanne) 8:337
Lee JH, Kim Y, Choi JW et al (2013) The association between papillary thyroid carcinoma and histologically proven Hashimoto’s thyroiditis: a meta-analysis. Eur J Endocrinol 168(3):343–349
Ma YJ, Deng XL, Li HQ (2015) BRAF(V600E) mutation and its association with clinicopathological features of papillary thyroid microcarcinoma: a meta-analysis. J Huazhong Univ Sci Technolog Med Sci 35(4):591–599
Kim SJ, Lee KE, Myong JP et al (2012) BRAF V600E mutation is associated with tumor aggressiveness in papillary thyroid cancer. World J Surg 36(2):310–317
Xing M, Alzahrani AS, Carson KA et al (2013) Association between BRAF V600E mutation and mortality in patients with papillary thyroid cancer. JAMA 309(14):1493–1501
Zhu Y, Zheng K, Zhang H et al (2016) The clinicopathologic differences of central lymph node metastasis in predicting lateral lymph node metastasis and prognosis in papillary thyroid cancer associated with or without Hashimoto’s thyroiditis. Tumour Biol 37(6):8037–8045
Ryu YJ, Cho JS, Park MH et al (2019) Identifying risk factors of recurrence for clinically node negative papillary thyroid carcinoma with pathologic N1a. BMC Surg 19(1):78
Wang X, Lei J, Wei T et al (2019) Clinicopathological characteristics and recurrence risk of papillary thyroid microcarcinoma in the elderly. Cancer Manag Res 11:2371–2377
Balachandran VP, Gonen M, Smith JJ et al (2015) Nomograms in oncology: more than meets the eye. Lancet Oncol 16(4):e173-180
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
W-XW and L-ZH: writing—original draft, software, data curation. S-YL: validation, formal analysis, data curation. FW and G-FQ: conceptualization. JY: validation, investigation. J-WF and YJ: writing—review and editing, visualization, supervision.
Corresponding author
Ethics declarations
Conflict of interest
This manuscript has not been published nor submitted for publication elsewhere. All authors have contributed significantly, and agree with the content of the manuscript. The authors reported no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Ethical approval
This study has been approved by the Institutional Review Board of Changzhou First People’s Hospital ethics committee, and has been performed according to the ethical standards laid down in the 1964 Declaration of Helsinki.
Informed consent
Due to the retrospective nature of this study, the need for informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, WX., Qi, GF., Feng, JW. et al. Construction of prediction models for determining the risk of lateral lymph node metastasis in patients with thyroid papillary carcinoma based on gender stratification. Eur Arch Otorhinolaryngol 280, 2511–2523 (2023). https://doi.org/10.1007/s00405-022-07812-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07812-x