Abstract
Purpose
Although reconstruction techniques after endoscopic skull base surgery have been improved, there are difficulties in reconstructing the skull base with a nasoseptal flap (NSF), especially in the case of high-flow cerebrospinal fluid (CSF) leak. The aim of this study was to analyze risk factors for the development of postoperative CSF leaks in terms of less experienced surgeon practices.
Methods
Retrospective review of medical records was performed for 125 patients who underwent endoscopic skull base surgery for intradural pathology with intraoperative high-flow CSF leakage between Oct 2012 and Apr 2017. Basic demographic data were collected, including body mass index (BMI), tumor pathology, comorbidities, and outcomes. To assess the learning curve effect, patients were divided into early cohort (n = 30) and late cohort (n = 95) groups.
Results
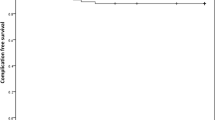
Overall postoperative CSF leakage was 10.4% (13/125) in this series. There were no significant risk factors for postoperative CSF leakage among the demographic data including BMI, comorbidities, or radiation history. Postoperative CSF leakage was most prevalent in the transclival approach than in other approaches, but the difference was not statistically significant (20.8%, p = 0.351). When dividing the results by timetable, the patients who underwent skull base reconstruction in the early cohort experienced more postoperative CSF leakage (23.3%, 7 cases out of 30) than in the late cohort (6.3%, 6 cases out of 95, p = 0.014). The learning curve was steeper in the early cohort (30 early cases 23.3%, 31–60 10%, 61–90 6.7%, 91–125 2.9%).
Conclusions
To improve the success rate of endoscopic skull base reconstruction, surgeons have to keep the basic technical details in mind to reduce the learning curve.



Similar content being viewed by others
References
Hadad G, Bassagasteguy L, Carrau RL, Mataza JC, Kassam A, Snyderman CH, Mintz A (2006) A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope 116:1882–1886
Harvey RJ, Parmar P, Sacks R, Zanation AM (2012) Endoscopic skull base reconstruction of large dural defects: a systematic review of published evidence. Laryngoscope 122:452–459
Eloy JA, Patel SK, Shukla PA, Smith ML, Choudhry OJ, Liu JK (2013) Triple-layer reconstruction technique for large cribriform defects after endoscopic endonasal resection of anterior skull base tumors. Int Forum Allergy Rhinol 3:204–211
Fraser S, Gardner PA, Koutourousiou M, Kubik M, Fernandez-Miranda JC, Snyderman CH, Wang EW (2018) Risk factors associated with postoperative cerebrospinal fluid leak after endoscopic endonasal skull base surgery. J Neurosurg 128:1066–1071
Zanation AM, Carrau RL, Snyderman CH, Germanwala AV, Gardner PA, Prevedello DM, Kassam AB (2009) Nasoseptal flap reconstruction of high flow intraoperative cerebral spinal fluid leaks during endoscopic skull base surgery. Am J Rhinol Allergy 23:518–521
Kim JS, Hong SD (2021) Risk factors for postoperative CSF leakage after endonasal endoscopic skull base surgery: a meta-analysis and systematic review. Rhinology 59:10–20
Younus I, Gerges MM, Uribe-Cardenas R, Morgenstern P, Kacker A, Tabaee A, Anand VK, Schwartz TH (2020) The slope of the learning curve in 600 consecutive endoscopic transsphenoidal pituitary surgeries. Acta Neurochir (Wien) 162:2361–2370
Jalisi S, O’Gara B, Toshkezi G, Chin L (2015) Local vascularized flap reconstruction of the skull base-clinical outcomes and analysis. World Neurosurg 83:87–92
Garcia-Navarro V, Anand VK, Schwartz TH (2013) Gasket seal closure for extended endonasal endoscopic skull base surgery: efficacy in a large case series. World Neurosurg 80:563–568
Kshettry VR, Do H, Elshazly K, Farrell CJ, Nyquist G, Rosen M, Evans JJ (2016) The learning curve in endoscopic endonasal resection of craniopharyngiomas. Neurosurg Focus 41:E9
Author information
Authors and Affiliations
Contributions
Conception and design: SDH, DK. Acquisition of data: WP, KEL. Analysis and interpretation of data: WP, SDH. Drafting the article: WP, SDH. Critically revising the article: DN, HYK, SC, YGJ. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript: all authors. Administrative/technical/material support: DK, KEL.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Park, W., Nam, DH., Kong, DS. et al. Learning curve and technical nuances of endoscopic skull base reconstruction with nasoseptal flap to control high-flow cerebrospinal fluid leakage: reconstruction after endoscopic skull base surgery other than pituitary surgery. Eur Arch Otorhinolaryngol 279, 1335–1340 (2022). https://doi.org/10.1007/s00405-021-06877-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-06877-4