Abstract
Purpose
The implementation of the universal two-child policy contributes to adverse pregnancy outcomes, but how the policy change leads to adverse pregnancy outcomes is not well elaborated. In this study, we aimed to compare maternal characteristics and complications, accessed the change in the proportion of maternal characteristics and maternal complications, and evaluated the mediation of maternal characteristics on maternal complications.
Methods
Demographic and clinical data of three-level sample facilities were extracted from China’s National Maternity Near Miss Obstetrics Surveillance System from Jan 1, 2012 to May 31, 2021. The associations between the universal two-child policy and maternal risk factors, the universal two-child policy and maternal complications, and maternal risk factors and maternal complications were evaluated using multivariate logistic regression analyses, with odds ratios (ORs) and 95% confidence intervals (CIs). Mediation analysis was used to estimate the potential mediation effects on the associations between the policy and maternal complications. Population-attributable fractions (PAF) were conducted to quantify the maternal complications burden attributable to the implementation of the universal two-child policy.
Results
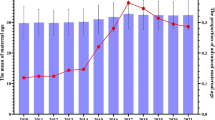
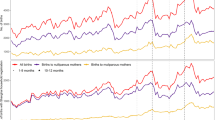
In the context of the universal two-child policy, the incidence of maternal near miss, antepartum or intrapartum complication, and post-partum complication increased at municipal- and county-level sample facilities. After adjusting for covariables, there were significant associations between the universal two-child policy and maternal risk factors (P < 0.001), the universal two-child policy and an increased risk of maternal complications (P < 0.001), and maternal risk factors and maternal complications(P < 0.001). The effects of the universal two-child policy on maternal near miss and medical disease were significantly mediated by maternal risk factors with mediation proportions of 19.77% and 4.07% at the municipal-level sample facility, and mediation proportions for 2.72% at the county-level sample facility on medical disease. The universal two-child policy contributed 19.34%, 5.82%, 8.29%, and 46.19% in the incidence of the maternal near miss, antepartum or intrapartum complication, post-partum complication, and medical disease at municipal-level sample facility, respectively. The corresponding PAF% at county-level sample facility was 40.49% for maternal near miss, 32.39% for the antepartum or intrapartum complication, 61.44% for post-partum complication, and 77.72% for medical disease. For provincial-level sample facility, the incidence of maternal near miss, antepartum or intrapartum complications, and medical diseases decreased (P < 0.05) and no statistically significant difference occurred in the incidence of post-partum complications.
Conclusions
In the context of the universal two-child policy, the incidence of maternal near miss, antepartum or intrapartum complication, and post-partum complication increased at municipal- and county-level sample facility. Maternal risk factors may play a mediating role in the effect of policy change and maternal complications. Provincial hospitals have been able to improve the quality of perinatal health care and reduce adverse pregnancy outcomes by adjusting their obstetric service strategies in the context of the new birth policy.
Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- NMNMSS:
-
National Maternal Near-Miss Surveillance System
- NOMCHS:
-
National Office for Maternal and Child Health Surveillance
- aOR:
-
Adjusted odds ratio
- CI:
-
Confidence intervals
- PAF:
-
Population-attributable fractions
References
Zeng Y, Hesketh T (2016) The effects of China’s universal two-child policy. Lancet 388(10054):1930–1938
Hesketh T, Zhu WX (1997) The one child family policy: the good, the bad, and the ugly. BMJ 314(7095):1685–1687
Zhang X, Lou H, Tang X et al (2021) Socio-demographic characteristics and outcomes of pregnant women who delivered prior to and after the termination of the one-child policy in China: a comparative study. BMC Pregnancy Childbirth 21(1):318
Feng W, Gu B, Cai Y (2016) The end of China’s one-child policy. Stud Fam Plann 47(1):83–86
Sun W, Gordon J, Pacey A (2016) From one to two: the effect of women and the economy on China’s one child policy. Hum Fertil (Camb) 19(1):1–2
Li HT, Xue M, Hellerstein S et al (2019) Association of China’s universal two child policy with changes in births and birth related health factors: national, descriptive comparative study. BMJ 366:l4680
Zhang HX, Zhao YY, Wang YQ (2018) Analysis of the characteristics of pregnancy and delivery before and after implementation of the two-child policy. Chin Med J (Engl) 131(1):37–42
Zhao F, Xu Y, Chen YT et al (2020) Influence of the universal two-child policy on obstetric issues. Eur J Obstet Gynecol Reprod Biol 252:479–82
Zeng C, Yang M, Ding Y et al (2018) Placenta accreta spectrum disorder trends in the context of the universal two-child policy in China and the risk of hysterectomy. Int J Gynaecol Obste Off Organ Int Fed Gynaecol Obste 140(3):312–318
Zhang X, Chen L et al (2020) Changes in maternal age and prevalence of congenital anomalies during the enactment of China’s universal two-child policy (2013–2017) in Zhejiang Province, China: An observational study. PLoS Med 17(2):e1003047
Sauer MV (2015) Reproduction at an advanced maternal age and maternal health. Fertil Steril 103(5):1136–1143
Cheng PJ (2016) Duan T China’s new two-child policy: maternity care in the new multiparous era. Bjog 123(Suppl 3):7–9
Teng X, Shane MI, Pan S (2020) The changing situation about maternal age, risk factors and pregnancy outcomes after the two-child policy: a retrospective cohort study. Ann Palliat Med 9(3):824–834
Yan J, Wang L, Yang Y et al (2020) The trend of caesarean birth rate changes in China after ‘universal two-child policy’ era: a population-based study in2013-2018. BMC Med 18(1):249
Li H, Fan C et al (2022) 2022 Changes in adverse pregnancy outcomes in women with advanced maternal age (AMA) after the enactment of China’s universal two-child policy. Sci Rep 12(1):5048
Zhang J, Williams GJ, Wang G et al (2021) Early-term birth and its association with universal two-child policy: a national cross-sectional study in China. BMJ Open 11(12):e054959
Fan SL, Xiao CN, Zhang YK et al (2020) How does the two-child policy affect the sex ratio at birth in China? A cross-sectional study. 20(1):789
Zhu J, Liang J, Mu Y et al (2016) Sociodemographic and obstetric characteristics of stillbirths in China: a census of nearly 4 million health facility births between 2012 and 2014. Lancet Glob Health 4(2):e109–e118
Say L, Souza JP, Pattinson RC (2009) Maternal near miss–towards a standard tool for monitoring quality of maternal health care. Best Pract Res Clin Obstet Gynaecol 23(3):287–296
Valeri L, Vanderweele TJ (2013) Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods 18(2):137–150
Bandoli G, Singh N (2020) Mediation of adverse pregnancy outcomes in autoimmune conditions by pregnancy complications: a mediation analysis of autoimmune conditions and adverse pregnancy outcomes. Arthritis Care Res (Hoboken) 72(2):256–264
Graubard BI, Fears TR (2005) Standard errors for attributable risk for simple and complex sample designs. Biometrics 61(3):847–855
Cakmak Celik F, Aygun C, Kucukoduk S et al (2017) Maternal and neonatal outcomes in advanced maternal age: a retrospective cohort study. J Matern Fetal Neonatal Med Off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet 30(20):2452–2456
Shan D, Qiu PY, Wu YX et al (2018) Pregnancy outcomes in women of advanced maternal age: a retrospective cohort study from China. Sci Rep 8(1):12239
Liu Y, Qin Q, Xiao Y et al (2019) Changes of second-time mothers and their infants under the universal two-child policy in Changsha, China. Midwifery 77:32–36
Lin PD, Bromage S, Mostofa MG et al (2019) Mediating role of arsenic in the relationship between diet and pregnancy outcomes: prospective birth cohort in Bangladesh. Environ Health Glob Access Sci Source 18(1):10
Singh PM, Rodrigues C, Gupta AN (1981) Placenta previa and previous cesarean section. Acta Obstet Gynecol Scand 60(4):367–368
Brenner WE, Edelman DA, Hendricks CH (1978) Characteristics of patients with placenta previa and results of “expectant management.” Am J Obstet Gynecol 132(2):180–191
Berchuck A, Sokol RJ (1983) Previous cesarean section, placenta increta, and uterine rupture in second-trimester abortion. Am J Obstet Gynecol 145(6):766–767
Hemminki E, Meriläinenb J (1996) Long-term effects of cesarean sections: ectopic pregnancies and placental problems. Am J Obstet Gynecol 174(5):1569–74
Deneux-Tharaux C (2012) Women with previous caesarean or other uterine scar: epidemiological features. J Gynecol Obstet Biol Reprod 41(8):697–707
Hofmeyr GJ, Say L, Gülmezoglu AM (2005) WHO systematic review of maternal mortality and morbidity: the prevalence of uterine rupture. Bjog 112(9):1221–8
Zwart JJ, Richters JM, Ory F et al (2009) Uterine rupture in The Netherlands: a nationwide population-based cohort study. Bjog 116(8):1069–78 (Discussion 78-80)
Fitzpatrick KE, Kurinczuk JJ, Alfirevic Z et al (2012) Uterine rupture by intended mode of delivery in the UK: a national case-control study. PLoS Med 9(3):e1001184
Rotas MA, Haberman S, Levgur M (2006) Cesarean scar ectopic pregnancies: etiology, diagnosis, and management. Obstet Gynecol 107(6):1373–1381
Hemminki E (1991) Long term maternal health effects of caesarean section. J Epidemiol Community Health 45(1):24–28
Smith GC, Pell JP, Dobbie R (2003) Caesarean section and risk of unexplained stillbirth in subsequent pregnancy. Lancet 362(9398):1779–1784
Kennare R, Tucker G, Heard A et al (2007) Risks of adverse outcomes in the next birth after a first cesarean delivery. Obstet Gynecol 109(2 Pt 1):270–276
Hemminki E, Shelley J, Gissler M (2005) Mode of delivery and problems in subsequent births: a register-based study from Finland. Am J Obstet Gynecol 193(1):169–177
Oliveira FC Jr, Costa ML, Cecatti JG et al (2013) Maternal morbidity and near miss associated with maternal age: the innovative approach of the 2006 Brazilian demographic health survey. Clinics (Sao Paulo, Brazil) 68(7):922–7
Blomberg M, Birch Tyrberg R, Kjølhede P (2014) Impact of maternal age on obstetric and neonatal outcome with emphasis on primiparous adolescents and older women: a Swedish medical birth register study. BMJ open 4(11):e005840
Liu J, Song L, Qiu J, et al (2020) Reducing maternal mortality in China in the era of the two-child policy. BMJ Glob Health 5(2):e002157
Liu X, Huang D, Wang Y et al (2020) Birth and birth-related obstetrical characteristics in southwestern China associated with the current adjustment of family planning policy: a 7-year retrospective study. Sci Rep 10(1):15949
Acknowledgements
We sincerely thank the department of obstetrics of 14 hospitals for their help in data collection and staff of maternal and child health institutions for data manage.
Funding
This work was supported by the Starup Fund for scientific research, Fujian Medical University (Grant number:2021 QH1170); Sponsored by Fujian provincial health technology project(Grant number:2020GGA021).
Author information
Authors and Affiliations
Contributions
LHL: project development, data analysis, manuscript writing. QPL: project development, manuscript editing. XMW: data collection, data analysis. RHZ: data management. LHZ: data management. HBZ: project development, manuscript editing. All authors read and approved the final manuscript as submitted.
Corresponding authors
Ethics declarations
Conflict of interests
All the authors declared they have no conflicts of interest.
Ethics approval and consent to participate
There was no direct interaction with patients and all the needed data are extracted from China’s National Maternal Near-Miss Surveillance System and the data used in the study containing no personally identifiable information. Therefore, there was unnecessary to get informed consent from individual patients. This study was approved by the ethics committee of the Fujian Maternity and Child Hospital. All methods were carried out in accordance with relevant guidelines and regulations. Need for informed consent to participate was waived by the ethics committee of the Fujian Provincial Maternity and Children Hospital.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, Lh., Lin, Q., Wang, Xm. et al. The possible impact of the universal two-child policy on pregnancy outcomes. Arch Gynecol Obstet (2023). https://doi.org/10.1007/s00404-023-07283-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00404-023-07283-3