Abstract
Background
Pain control is essential to successful total shoulder arthroplasty (TSA).
Materials and methods
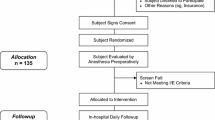
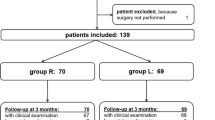
This non-blinded, randomized clinical trial compared shoulder pain, narcotic use, interscalene (IS) block application time, and costs in 76 subjects who were randomly assigned to receive either a single injection IS nerve block of 10 cc (133 mg) liposomal bupivacaine mixed with 10 cc of 0.5% bupivacaine (Group 1), or 20 cc of 0.5% ropivacaine direct injection combined with an indwelling IS nerve block catheter delivering 0.2% ropivacaine at a continual 4 cc/h infusion for the initial 3 post-operative days (Group 2). Surgical time, local anesthesia duration, hospital stay length, morphine milligram equivalents (MME) consumed, worst shoulder pain at 24, 48 and 72 h, and complications were recorded. Patient reported function, pain and activity level surveys were completed before, and 6-week post-TSA (P < 0.05).
Results
Group 1 had less pain 24-h (0.72 ± 0.8 vs. 3.4 ± 2.9, p < 0.0001) and 48-h (2.5 ± 2.2 vs. 4.8 ± 2.6, p = 0.005) post-TSA. At 24-h post-TSA, MME consumption was similar (Group 1 = 4.5 ± 6.4 vs. Group 2 = 3.7 ± 3.8, p = 0.54), but was lower for Group 1 at 48 h (0.0 ± 0.0 vs. 0.64 ± 0.99, p = 0.001). Group 2 had longer IS block application time (10.00 ± 4.6 min vs. 4.84 ± 2.7 min, p < 0.0001). Only group 2 had a strong relationship between MME consumption over the first 24-h post-TSA and pain 24-h post-TSA (r = 0.76, p < 0.0001), a moderate relationship with pain 48-h post-TSA (r = 0.59, P = 0.001), and a weak relationship with pain 72-h post-TSA (r = 0.44, P = 0.02). Significant relationships for these variables were not observed for Group 1 (r ≤ 0.30, p ≥ 0.23). Group 1 IS block costs were less/patient than Group 2 ($190.17 vs. $357.12 USD).
Conclusion
A single shot, liposomal bupivacaine interscalene nerve block provided better post-TSA pain control with less narcotic consumption, less time for administration and less healthcare system cost compared to interscalene nerve block using a continuous indwelling catheter.
Level of evidence
Level I, Prospective, Randomized.


Similar content being viewed by others
References
Chahar P, Cummings KC 3rd (2012) Liposomal bupivacaine: a review of a new bupivacaine formulation. J Pain Res 5:257–264. https://doi.org/10.2147/JPR.S27894
Xiao M, Cohen SA, Cheung EV, Freehill MT, Abrams GD (2021) Pain management in shoulder arthroplasty: A systematic review and network meta-analysis of randomized controlled trials. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2021.06.008
Bishop JY, Sprague M, Gelber J et al (2005) Interscalene regional anesthesia for shoulder surgery. J Bone Joint Surg Am 87(5):974–979. https://doi.org/10.2106/JBJS.D.02003
YaDeau JT, Dines DM, Liu SS et al (2019) What pain levels do TSA patients experience when given a long-acting nerve block and multimodal analgesia? Clin Orthop Relat Res 477(3):622–632. https://doi.org/10.1097/CORR.0000000000000597
Kim N, Matzon JL, Abboudi J et al (2016) A prospective evaluation of opioid utilization after upper-extremity surgical procedures: Identifying consumption patterns and determining prescribing guidelines. J Bone Joint Surg Am 98(20):e89. https://doi.org/10.2106/JBJS.15.00614
Bjørnholdt KT, Jensen JM, Bendtsen TF, Søballe K, Nikolajsen L (2015) Local infiltration analgesia versus continuous interscalene brachial plexus block for shoulder replacement pain: a randomized clinical trial. Eur J Orthop Surg Traumatol 25(8):1245–1252. https://doi.org/10.1007/s00590-015-1678-2
Verdecchia NM, Rodosky MW, Kentor M, Orebaugh SL (2021) Liposomal bupivacaine infiltration in the surgical site for analgesia after rotator cuff repair: A randomized, double-blinded, placebo-controlled trial. J Shoulder Elbow Surg 30(5):986–993. https://doi.org/10.1016/j.jse.2020.10.035
Panchamia JK, Amundson AW, Jacob AK et al (2019) A 3-arm randomized clinical trial comparing interscalene blockade techniques with local infiltration analgesia for total shoulder arthroplasty. J Shoulder Elbow Surg 28(10):e325–e338. https://doi.org/10.1016/j.jse.2019.05.013
Kolade O, Patel K, Ihejirika R et al (2019) Efficacy of liposomal bupivacaine in shoulder surgery: A systematic review and meta-analysis. J Shoulder Elbow Surg 28(9):1824–1834. https://doi.org/10.1016/j.jse.2019.04.054
Namdari S, Nicholson T, Abboud J, Lazarus M, Steinberg D, Williams G (2017) Randomized controlled trial of interscalene block compared with injectable liposomal bupivacaine in shoulder arthroplasty. J Bone Joint Surg Am 99(7):550–556. https://doi.org/10.2106/JBJS.16.00296
Banghu M, Mutter T, Dubberley J, MacDonald P, Dufault B, Amadeo R (2017) Single-injection interscalene bupivacaine and dexamethasone for same-day discharge total shoulder arthroplasty: A case series. Can J Anaesth 64(4):435–437. https://doi.org/10.1007/s12630-016-0788-6
Sun H, Li S, Wang K et al (2018) Do liposomal bupivacaine infiltration and interscalene nerve block provide similar pain relief after total shoulder arthroplasty: A systematic review and meta-analysis. J Pain Res 11:1889–1900. https://doi.org/10.2147/JPR.S177716
YaDeau JT, Gordon MA, Goytizolo EA et al (2016) Buprenorphine, clonidine, dexamethasone, and ropivacaine for interscalene nerve blockade: A prospective, randomized, blinded, ropivacaine dose-response study. Pain Med 17(5):940–960. https://doi.org/10.1093/pm/pnv010
Wang K, Zhang H-X (2017) Liposomal bupivacaine versus interscalene nerve block for pain control after total shoulder arthroplasty: A systematic review and meta-analysis. Int J Surg 46:61–70. https://doi.org/10.1016/j.ijsu.2017.08.569
Tetzlaff JE, Yoon HJ, Brems J (1994) Interscalene brachial plexus block for shoulder surgery. Reg Anesth 19(5):339–343
Routman HD, Israel LR, Moor MA, Boltuch AD (2017) Local injection of liposomal bupivacaine combined with intravenous dexamethasone reduces postoperative pain and hospital stay after shoulder arthroplasty. J Shoulder Elbow Surg 26(4):641–647. https://doi.org/10.1016/j.jse.2016.09.033
Auyong DB, Yuan SC, Choi DS, Pahang JA, Slee AE, Hanson NA (2017) A double-blind randomized comparison of continuous interscalene, supraclavicular, and suprascapular blocks for total shoulder arthroplasty. Reg Anesth Pain Med 42(3):302–309. https://doi.org/10.1097/AAP.0000000000000578
Chalmers PN, Salazar D, Fingerman ME, Keener JD, Chamberlain A (2017) Continuous interscalene brachial plexus blockade is associated with reduced length of stay after shoulder arthroplasty. Orthop Traumatol Surg Res 103(6):847–852. https://doi.org/10.1016/j.otsr.2017.06.007
Bojaxhi E, Lumermann LA, Mazer LS, Howe BL, Ortiguera CJ, Clendenen SR (2019) Interscalene brachial plexus catheter versus single-shot interscalene block with periarticular local infiltration analgesia for shoulder arthroplasty. Minerva Anestesiol 85(8):840–845. https://doi.org/10.23736/S0375-9393.19.13387-1
McNaught A, McHardy P, Awad IT (2010) Posterior interscalene block: an ultrasound-guided case series and overview of history, anatomy and techniques. Pain Res Manag 15(4):219–223. https://doi.org/10.1155/2010/758174
Gabriel RA, Nagrebetsky A, Kaye AD, Dutton RP, Urman RD (2016) The patterns of utilization of interscalene nerve blocks for total shoulder arthroplasty. Anesth Analg 123(3):758–761. https://doi.org/10.1213/ANE.0000000000001472
Updegrove GF, Stauch CM, Ponnuru P, Kunselman AR, Armstrong AD (2020) Efficacy of local infiltration anesthesia versus interscalene nerve blockade for total shoulder arthroplasty. JSES Int 4(2):357–361. https://doi.org/10.1016/j.jseint.2019.12.007
Thompson M, Simonds R, Clinger B et al (2017) Continuous versus single shot brachial plexus block and their relationship to discharge barriers and length of stay. J Shoulder Elbow Surg 26(4):656–661. https://doi.org/10.1016/j.jse.2016.09.026
Choi S, Rodseth R, McCartney CJ (2014) Effects of dexamethasone as a local anaesthetic adjuvant for brachial plexus block: a systematic review and meta-analysis of randomized trials. Br J Anaesth 112(3):427–439. https://doi.org/10.1093/bja/aet417
Wells N, Pasero C, McCaffery M (2008) Improving the quality of care through pain assessment and management. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US) Chapter 17
Vorobeichik L, Brull R, Bowry R, Laffey JG, Abdallah FW (2018) Should continuous rather than single-injection interscalene block be routinely offered for major shoulder surgery? A meta-analysis of the analgesic and risk-effects profiles. Br J Anaesth 120(4):679–692. https://doi.org/10.1016/j.bja.2017.11.104
Codding JL, Getz CL (2018) Pain management strategies in shoulder arthroplasty. Orthop Clin North Am 49:81–91. https://doi.org/10.1016/j.ocl.2017.08.010
Budge M, Orvets N, Shields E (2020) Single-shot liposomal bupivacaine interscalene nerve block provides equivalent pain relief compared to continuous catheter interscalene nerve block in total shoulder arthroplasty. JSESArthro 30(4):285–290. https://doi.org/10.1053/j.sart.2020.09.003
Ilfeld BM, Viscusi ER, Hadzic A et al (2015) Safety and side effect profile of liposome bupivacaine (exparel) in peripheral nerve blocks. Reg Anesth Pain Med 40(5):572–582. https://doi.org/10.1097/AAP.0000000000000283
Sicard J, Klouche S, Conso C et al (2019) Local infiltration analgesia versus interscalene nerve block for postoperative pain control after shoulder arthroplasty: A prospective, randomized, comparative noninferiority study involving 99 patients. J Shoulder Elbow Surg 28(2):212–219. https://doi.org/10.1016/j.jse.2018.09.026
Hattrup SJ, Chung AS, Rosenfeld DM et al (2021) Liposomal bupivacaine interscalene nerve block in shoulder arthroplasty is not superior to plain bupivacaine: A double-blinded prospective randomized control trial. J Shoulder Elbow Surg 30(3):587–598. https://doi.org/10.1016/j.jse.2020.09.017
Abildgaard JT, Lonergan KT, Tolan SJ et al (2017) Liposomal bupivacaine versus indwelling interscalene nerve block for postoperative pain control in shoulder arthroplasty: A prospective randomized controlled trial. J Shoulder Elbow Surg 26(7):1175–1181. https://doi.org/10.1016/j.jse.2017.03.012
Yan Z, Chen Z, Ma C (2017) Liposomal bupivacaine versus interscalene nerve block for pain control after shoulder arthroplasty: A meta-analysis. Medicine (Baltimore) 96(27):e7226. https://doi.org/10.1097/MD.000000000000722634
Weir TB, Simpson N, Aneizi A et al (2020) Single-shot liposomal bupivacaine interscalene block versus continuous interscalene catheter in total shoulder arthroplasty: Opioid administration, pain scores, and complications. J Orthop 22:261–267. https://doi.org/10.1016/j.jor.2020.05.006
Cao X, Pan F (2017) Comparison of liposomal bupivacaine infiltration versus interscalene nerve block for pain control in total shoulder arthroplasty: A meta-analysis of randomized control trails. Medicine (Baltimore) 96(39):e8079. https://doi.org/10.1097/MD.0000000000008079
Angerame MR, Ruder JA, Odum SM, Hamid N (2017) Pain and opioid use after total shoulder arthroplasty with injectable liposomal bupivacaine versus interscalene block. Orthop 40(5):e806–e811. https://doi.org/10.3928/01477447-20170608-01
Sethi PM, Brameier DT, Mandava NK, Miller SR (2019) Liposomal bupivacaine reduces opiate consumption after rotator cuff repair in a randomized controlled trial. J Shoulder Elbow Surg 28(5):819–827. https://doi.org/10.1016/j.jse.2019.01.008
Patel MA, Gadsden JC, Nedeljkovic SS et al (2020) Brachial plexus block with liposomal bupivacaine for shoulder surgery improves analgesia and reduces opioid consumption: Results from a multicenter, randomized, double-blind, controlled trial. Pain Med 21(2):387–400. https://doi.org/10.1093/pm/pnz103
Namdari S, Nicholson T, Abboud J, Lazarus M, Steinberg D, Williams G (2018) Interscalene block with and without intraoperative local infiltration with liposomal bupivacaine in shoulder arthroplasty: A randomized controlled trial. J Bone Joint Surg Am 100(16):1373–1378. https://doi.org/10.2106/JBJS.17.01416
Kocher M, Horan MP, Briggs KK, Richardson TR, O’Holleran J, Hawkins RJ (2005) Reliability, validity, and responsiveness of the American Shoulder and Elbow Surgeons subjective shoulder scale in patients with shoulder instability, rotator cuff disease, and glenohumeral arthritis. J Bone Joint Surg 87(9):2006–2011. https://doi.org/10.2106/JBJS.C.01624
Furtado R, MacDermid J (2019) Clinimetrics: Single assessment numeric evaluation. Bone Joint Institute 65(2):111. https://doi.org/10.1016/j.jphys.2019.02.001
Thigpen CA, Shanley E, Momaya AM, Kissenberth MJ, Tolan SJ, Tokish JM, Hawkins RJ (2018) Validity and responsiveness of the single alpha-numeric evaluation for shoulder patients. Am J Sports Med 46(14):3480–3485. https://doi.org/10.1177/0363546518807924
Bijur PE, Silver W, Gallagher EJ (2001) Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med 8:1153–1157. https://doi.org/10.1111/j.1553-2712.2001.tb01132.x
Mukaka MM (2012) Statistics Corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med J 24(3):69–71
Harjula JNE, Paloneva J, Haapakoski J, Kukkonen J, Äärimaa V (2018) Increasing incidence of primary shoulder arthroplasty in Finland - a nationwide registry study. BMC Musculoskelet Disord 19(1):245. https://doi.org/10.1186/s12891-018-2150-3
Kim SH, Wise BL, Zhang Y, Szabo RM (2011) Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am 93(24):2249–2254. https://doi.org/10.2106/JBJS.J.01994
Best MJ, Aziz KT, Wilckens JH, McFarland EG, Srikumaran U (2021) Increasing incidence of primary reverse and anatomic total shoulder arthroplasty in the United States. J Shoulder Elbow Surg 30(5):1159–1166. https://doi.org/10.1016/j.jse.2020.08.010
Charles MD, Cvetanovich G, Sumner-Parilla S, Nicholson GP, Verma N, Romeo AA (2019) Outpatient shoulder arthroplasty: outcomes, complications, and readmissions in 2 outpatient settings. J Shoulder Elbow Surg 28(6S):S118–S123. https://doi.org/10.1016/j.jse.2019.04.006
Sabesan VJ, Shahriar R, Petersen-Fitts GR, Whaley JD, Bou-Akl T, Sweet M, Milia M (2017) A prospective randomized controlled trial to identify the optimal postoperative pain mangement in shoulder arthroplasty: Liposomal bupivacaine versus continuous interscalene catheter. J Shoulder Elbow Surg 26:1810–1817. https://doi.org/10.1016/j.jse.2017.06.044
Malik O, Kaye AD, Kaye A, Belani K, Urman RD (2017) Emerging roles of liposomal bupivacaine in anesthesia practice. J Anaesthesiol Clin Pharmacol 33:151–156. https://doi.org/10.4103/joacp.JOACP_375_15
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study with human subjects by approved by a medical institutional review board.
Informed consent
All study subjects provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Krupp, R., Smith, A., Nyland, J. et al. Liposomal bupivacaine nerve block provides better pain control post-total shoulder arthroplasty than continuous indwelling catheter. Arch Orthop Trauma Surg 143, 1895–1902 (2023). https://doi.org/10.1007/s00402-022-04386-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04386-5