Abstract
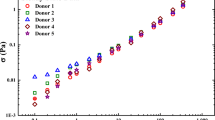
Hemorheology is the study of blood flow and the mechanical stresses and kinematics involved. The Casson constitutive equation is a popular and simple model used to describe the steady shear rheology of blood, with only two parameters that specify an infinite shear viscosity and a yield stress that depend on blood physiology. Previous literature has identified hematocrit and fibrinogen concentration as the two most important physiological factors that affect blood flow, but previous parameterizations of the Casson model may not be reliable due to the use of non-standardized data sets. This study uses machine learning and the largest standardized dataset to improve the parameterization of the Casson model with respect to hematocrit and fibrinogen concentration for healthy individuals. The study also employs machine learning to identify a potential additional factor, the mean corpuscular hemoglobin (MCH), that may affect blood rheology. The proposed approach demonstrates the potential for machine learning to improve the connection between physiology and blood rheology with possible implications in cardiovascular diagnostics.










Similar content being viewed by others
Data availability
A GitHub repository contains the code used for predictions made in this paper at: https://github.com/FarringtonSM/Hemostatistics_BloodRheology_and_MachineLearning. The data (Horner 2020) used in this work is found at: https://sites.udel.edu/wagnergroup/files/2016/06/Horner-Thesis-Data.xlsx
References
Apostolidis AJ, Armstrong MJ, Beris AN (2015) Modeling of human blood rheology in transient shear flows. J Rheol 59(1):275–298
Apostolidis AJ, Beris AN (2014) Modeling of the blood rheology in steady-state shear flows. J Rheol 58(3):607–633
Apostolidis AJ, Beris AN (2016) The effect of cholesterol and triglycerides on the steady state shear rheology of blood. Rheol Acta 55(6):497–509
Armstrong M, Pincot A, Jariwala S, Horner J, Wagner N, Beris A (2022) Tensorial formulations for improved thixotropic viscoelastic modeling of human blood. J Rheol 66(2):327–347
Ashraf C, Joshi N, Beck DAC, Pfaendtner J (2021) Data science in chemical engineering: applications to molecular science. Annu Rev Chem Biomol Eng 12(1):15–37
Baskurt O, Neu B, Meiselman HJ (2011) Red Blood Cell Aggregation. CRC Press
Baskurt OK, Meiselman HJ (2008) RBC aggregation: more important than RBC adhesion to endothelial cells as a determinant of in vivo blood flow in health and disease. Microcirculation 15(7):585–590
Benjamin RJ, McLaughlin LS (2012) Plasma components: properties, differences, and uses. Transfusion 52:9S–19S
Beris AN, Horner JS, Jariwala S, Armstrong MJ, Wagner NJ (2021) Recent advances in blood rheology: a review. Soft Matter 17(47):10591–10613
Blair GWS (1959) An equation for the flow of blood, plasma and serum through glass capillaries. Nature 183(4661):613–614
Casson N (1959) A flow equation for pigment-oil suspensions of the printing ink type. Rheol Dis Sys:84–104
CDC. (2022). “Heart disease facts.” Retrieved 03/01/2022, from https://www.cdc.gov/heartdisease/facts.htm.
Chicco D, Warrens MJ, Jurman G (2021) The coefficient of determination R-squared is more informative than SMAPE, MAE, MAPE, MSE and RMSE in regression analysis evaluation. PeerJ Comput Sci 7:e623
Chien S (1975) Biophysical behavior of red cells in suspensions. Red Blood Cell 2:1031–1133
Chien S (1986) Blood rheology in myocardial-infarction and hypertension. Biorheology 23(6):633–653
Choi D, Waksman O, Shaik A, Mar P, Chen Q, Cho DJ, Kim H, Smith RL, Goonewardena SN, Rosenson RS (2022) Association of blood viscosity with mortality among patients hospitalized with COVID-19. J Am Coll Cardiol 80(4):316–328
Çınar T, Hayıroğlu Mİ, Selçuk M, Çiçek V, Doğan S, Kılıç Ş, Yavuz S, Babaoğlu M, Uzun M, Orhan AL (2022) Association of whole blood viscosity with thrombus presence in patients undergoing transoesophageal echocardiography. Int J Cardiovasc Imaging 38(3):601–607
Connes P, Alexy T, Detterich J, Romana M, Hardy-Dessources MD, Ballas SK (2016) The role of blood rheology in sickle cell disease. Blood Rev 30(2):111–118
Coppola L, Caserta F, De Lucia D, Guastafierro S, Grassia A, Coppola A, Marfella R, Varricchio M (2000) Blood viscosity and aging. Arch Gerontol Geriatr 31(1):35–42
Dintenfass L (1974) Blood rheology as diagnostic and predictive tool in cardiovascular diseases: effect of ABO Blood groups. Angiology 25(6):365–372
Fedosov DA, Pan WX, Caswell B, Gompper G, Karniadakis GE (2011) Predicting human blood viscosity in silico. Proceedings of the National Academy of Sciences of the United States of America 108(29):11772–11777
Fryar CD, Chen TC, Li X (2012) Prevalence of uncontrolled risk factors for cardiovascular disease: United States, 1999-2010. NCHS Data Brief 103
Gahleitner M (1999) Rheology as a quality control instrument. J Macromol Sci A 36(11):1731–1741
Gustavsson CG, Persson SU, Larsson H, Persson S (1994) Blood-viscosity in relation to blood hemoglobin concentration in healthy-subjects and in patients with different cardiovascular-diseases. Clin Hemorheol 14(5):677–683
Hitsumoto T (2017) Relationship between cardiovascular risk factors and hemorheology assessed by microchannel method in patients with type 2 diabetes mellitus. Diabetol Int 8:316–322
Hoore M, Yaya F, Podgorski T, Wagner C, Gompper G, Fedosov DA (2018) Effect of spectrin network elasticity on the shapes of erythrocyte doublets. Soft Matter 14(30):6278–6289
Horner JS (2020) An experimental and theoretical investigation of blood rheology. University of Delaware
Horner JS, Armstrong MJ, Wagner NJ, Beris AN (2019) Measurements of human blood viscoelasticity and thixotropy under steady and transient shear and constitutive modeling thereof. J Rheol 63(5):799–813
Horner JS, Beris AN, Woulfe DS, Wagner NJ (2018) Effects of ex vivo aging and storage temperature on blood viscosity. Clin Hemorheol Microcirc 70(2):155–172
Hutton RD (1979) The effect of iron deficiency on whole blood viscosity in polycythaemic patients. British J Haematol 43(2):191–199
Jariwala S, Wagner NJ, Beris AN (2022) A thermodynamically consistent, microscopically-based, model of the rheology of aggregating particles suspensions. Entropy 24(5):717
Javadi E, Li H, Gallastegi AD, Frydman GH, Jamali S, Karniadakis GE (2022) Circulating cell clusters aggravate the hemorheological abnormalities in COVID-19. Biophys J 121(18):3309–3319
Korculanin O, Kochetkova T, Lettinga MP (2021) Competition between red blood cell aggregation and breakup: depletion force due to filamentous viruses vs. shear flow. Front Phys 9:721368
Kyrle P, Eichinge S (2005) Deep vein thrombosis. Lancet 365:1163–1174
Le Devehat C, Vimeux M, Khodabandehlou T (2004) Blood rheology in patients with diabetes mellitus. Clin Hemorheol Microcirc 30(3-4):297–300
Lemonne N, Lamarre Y, Romana M, Hardy-Dessources MD, Lionnet F, Waltz X, Tarer V, Mougenel D, Tressieres B, Lalanne-Mistrih ML, Etienne-Julan M, Connes P (2014) Impaired blood rheology plays a role in the chronic disorders associated with sickle cell-hemoglobin C disease. Haematologica 99(5):74–75
Lowe G, Rumley A, Norrie J, Ford I, Shepherd J, Cobbe S, Macfarlane P, Packard C (2000) Blood rheology, cardiovascular risk factors, and cardiovascular disease: the West of Scotland Coronary Prevention Study. Thromb Haemost 84(10):553–558
Magzoub MI, Kiran R, Salehi S, Hussein IA, Nasser MS (2021) Assessing the relation between mud components and rheology for loss circulation prevention using polymeric gels: a machine learning approach. Energies 14(5):1377
Mahmoudabadbozchelou M, Caggioni M, Shahsavari S, Hartt WH, Em Karniadakis G, Jamali S (2021) Data-driven physics-informed constitutive metamodeling of complex fluids: a multifidelity neural network (MFNN) framework. J Rheol 65(2):179–198
MayoClinic. (2021). “Heart disease: diagnosis & treatment.” Retrieved 07/01/2022, from https://www.mayoclinic.org/diseases-conditions/heart-disease/diagnosis-treatment/drc-20353124.
Merrill EW (1969) Yield stress of normal human blood as a function of endogenous fibrinogen. J Appl Physiol 26(1):1–3
Merrill EW, Gilliland ER, Cokelet G, Shin H, Britten A, Wells RE (1963a) Rheology of human blood, near and at zero flow: effects of temperature and hematocrit level. Biophys J 3(3):199–213
Merrill EW, Wells RE, Cokelet GC, Britten A (1963b) Non-Newtonian rheology of human blood-effect of fibrinogen deduced by subtraction. Circ Res 13(1):48
Merrill EW, Gilliland ER, Lee TS, Salzman EW (1966) Blood rheology: effect of fibrinogen deduced by addition. Circ Res 18(4):437–446
Moreno L, Calderas F, Sanchez-Olivares G, Medina-Torres L, Sanchez-Solis A, Manero O (2015) Effect of cholesterol and triglycerides levels on the rheological behavior of human blood. Korea Aust Rheol J 27(1):1–10
Mujumdar A, Beris AN, Metzner AB (2002) Transient phenomena in thixotropic systems. J Nonnewton Fluid Mech 102(2):157–178
Nwose EU, Richards RS (2011) Whole blood viscosity extrapolation formula: Note on appropriateness of units. North American Journal of Medical Sciences 3(8):384–386
Padilla O, Abadie J (2021) Blood tests: normal values. https://www.merckmanuals.com/professional/resources/normal-laboratory-values/blood-tests-normal-values. Accessed 09/01/2022
Pedregosa F, Varoquaux G, Gramfort A, Michel V, Thirion B, Grisel O, Blondel M, Prettenhofer P, Weiss R, Dubourg V, Vanderplas J, Passos A, Cournapeau D, Brucher M, Perrot M, Duchesnay É (2011) Scikit-learn: machine learning in Python. J Mach Learn Res 12:2825–2830
Rasmussen CE, Williams CKI (2006) Gaussian Processes for Machine Learning. The MIT Press
Ratner B (2009) The correlation coefficient: Its values range between +1/−1, or do they. J Target Meas Anal Mark 17(2):139–142
Rosenson RS, Wolff D, Green D, Boss AH, Kensey KR (2004) Aspirin. J Thromb Haemost 2(2):340–341
Saadat M, Mahmoudabadbozchelou M, Jamali S (2022) Data-driven selection of constitutive models via rheology-informed neural networks (RhINNs). Rheol Acta 61(10):721–732
Tabesh H, Poorkhalil A, Akbari H, Rafiei F, Mottaghy K (2022) Phenomenological characterization of blood’s intermediate shear rate: a new concept for hemorheology. Phys Eng Sci Med
Torpy JM, Glass TJ, Glass RM (2007) Retinopathy. JAMA 298(8):944
Von de Pette JEW, Guthrie DL, Pearson TC (1986) Whole blood viscosity in polycythaemia: the effect of iron deficiency at a range of haemoglobin and packed cell volumes. British J Haematol 63(2):369–375
Wagner NJ, Mewis J (2021) Theory and Applications of Colloidal Suspension Rheology. Cambridge University Press, Cambridge
Wells RE, Merrill EW (1961) Shear rate dependence of the viscosity of whole blood and plasma. Science 133(3455):763–764
Wells RE, Merrill EW (1962) Influence of flow properties of blood upon viscosity-hematocrit relationships*. J Clin Investig 41(8):1591–1598
Yazdani A, Deng Y, Li H, Javadi E, Li Z, Jamali S, Lin C, Humphrey JD, Mantzoros CS, Em Karniadakis G (2021) Integrating blood cell mechanics, platelet adhesive dynamics and coagulation cascade for modelling thrombus formation in normal and diabetic blood. J R Soc Interface 18(175):20200834
Zitnik M, Nguyen F, Wang B, Leskovec J, Goldenberg A, Hoffman MM (2019) Machine learning for integrating data in biology and medicine: principles, practice, and opportunities. Inf Fusion 50:71–91
Acknowledgements
We would like to acknowledge the NRT Midas program at the University of Delaware for assistance with data science in soft materials. Funding from the National Science Foundation (NSF) through the award CBET 1804911 is also gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human or animal participants performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Farrington, S., Jariwala, S., Armstrong, M. et al. Physiology-based parameterization of human blood steady shear rheology via machine learning: a hemostatistics contribution. Rheol Acta 62, 491–506 (2023). https://doi.org/10.1007/s00397-023-01402-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00397-023-01402-2