Abstract
Purpose
Time-related eating patterns have been associated with metabolic and nutritional diseases such as obesity. However, there is a lack of representative studies on this subject. This study's aim was to assess the association between the timing of eating and obesity in a large and representative sample of the Brazilian adult population (POF 2008–2009 survey).
Methods
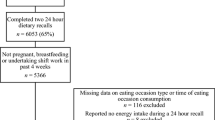
Two days of adults’ food diary (n = 21,020) were used to estimate tertiles of first and last meal intake times, eating midpoint, caloric midpoint time, and calories consumed from 18:00 h onwards. BMI was estimated and its values, as well as excess weight (BMI ≥ 25 kg/m2) and obesity (BMI ≥ 30 kg/m2) were used as outcomes. Multiple linear and logistic regressions were performed.
Results
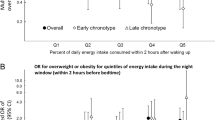
The first (β = 0.65, 95% CI 0.37–0.93) and last food intake time (β = 0.40, 95% CI 0.14–0.66), eating midpoint (β = 0.61, 95% CI 0.34–0.88) and calories consumed after 21:00 h (β = 0.74, 95% CI 0.32–1.16) and 22:00 h (β = 0.75, 95% CI 0.18–1.32) were positively associated with BMI. The likelihood of having excess weight or obesity was significantly higher in the third tertile of the first food intake time (OR = 1.28, 95% CI 1.13–1.45 and OR = 1.34, 95% CI 1.13–1.58, respectively), last food intake time (OR = 1.16, 95% CI 1.03–1.32; and OR = 1.18, 95% CI 1.00–1.41, respectively), eating midpoint (OR = 1.28, 95% CI 1.13–1.45; and OR = 1.35, 95% CI 1.14–1.59, respectively) and energy consumption after 21:00 h (OR = 1.33, 95% CI 1.10–1.59).
Conclusion
Chrononutrition meal patterns indicative of late meal intake were significantly associated with high BMI, excess weight and obesity in the Brazilian population.

Similar content being viewed by others
Data availability
The datasets analyzed in the current study are freely available on the IBGE website (https://www.ibge.gov.br/estatisticas/sociais/saude/24786-pesquisa-de-orcamentos-familiares-2.html).
References
NCD Risk Factor Collaboration (NCD-RisC) (2017) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 390(10113):2627–2642
Boutari CI, Mantzoros CS (2022) A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metab Clin Exp 133:155217
Boutari CI, Mantzoros CS (2022) Pesquisa nacional de saúde: 2019: atenção primária à saúde e informações antropométricas: Brasil/IBGE, Coordenação de Trabalho e Rendimento. Rio de Janeiro: IBGE 2020:66p
Bo S, Musso G, Beccuti G, Fadda M, Fedele D, Gambino R (2014). Consuming more of daily caloric intake at dinner predisposes to obesity. A 6-year population-based prospective cohort study. PLoS ONE 9(9):e108467
Eicher-Miller HA, Khanna N, Boushey CJ, Gelfand SB, Delp EJ (2016) Temporal dietary patterns derived among the adult participants of the national health and nutrition examination survey 1999–2004 are associated with diet quality. J Acad Nutr Diet 116:283–291
Oike H, Oishi K, Kobori M (2014) Nutrients, clock genes, and chrononutrition. Curr Nutr Rep 3:204–212
Oda H (2015) Chrononutrition. J Nutr Sci Vitaminol 61:S92–S94
Van Cauter E, Polonsky KS, Scheen AJ (1997) Roles of circadian rhythmicity and sleep in human glucose regulation. Endocr Rev 18(5):716–738
Morgan L, Hampton S, Gibbs M, Arendt J (2003) Circadian aspects of postprandial metabolism. Chronobiol Int 20(5):795–808
Wehrens SMT et al (2017) Meal timing regulates the human circadian system. Curr Biol 27(12):1768–1775
Garaulet M, Gómez-Abellán P, Alburquerque-Béjar JJ, Lee Y-C, Ordovás JM, Scheer FAJL (2013) Timing of food intake predicts weight loss effectiveness. Int J Obes 37:604–611
Fong M, Caterson ID, Madigan CD (2017) Are large dinners associated with excess weight, and does eating a smaller dinner achieve greater weight loss? A systematic review and meta-analysis. Br J Nutr 118(8):616–628
Leung GKW, Huggins CE, Ware RS, Bonham MP (2020). Time of day difference in postprandial glucose and insulin responses: systematic review and meta-analysis of acute postprandial studies. Chronobiol Int 37(3):311–326
Zitting KM, Vujovic N, Yuan RK et al (2018) Human resting energy expenditure varies with circadian phase. Curr Biol 28(22):3685–90. 19e3.
Gill S, Panda SA (2015) Smartphone App reveals erratic diurnal eating patterns in humans that can be modulated for health benefits. Cell Metab 22:789–798
Chaix A, Zarrinpar A, Miu P, Panda S (2014) Time-restricted feeding is a preventative and therapeutic intervention against diverse nutritional challenges. Cell Metab 20:991–1005
Ruiz-Lozano T, Vidal J, De Hollanda A, Scheer FA, Garaulet M, Izquierdo-Pulido M (2016) Timing of food intake is associated with weight loss evolution in severe obese patients after bariatric surgery. Clin Nutr 35(6):1308–1314
Estivaleti JM, Guzman-HabingerJ LJ et al (2022) Time trends and projected obesity epidemic in Brazilian adults between 2006 and 2030. Sci Rep 12(1):1–8
Cuevas García-Dorado S, Cornselsen L, Smith R, Walls H (2019) Economic globalization, nutrition and health: a review of quantitative evidence. Glob Health 15(1):1–19
Instituto Brasileiro de Geografia e Estatística (IBGE) (2011) Pesquisa de orçamentos familiares 2008–2009: análise do consumo alimentar pessoal no Brasil/IBGE, Coordenação de Trabalho e Rendimento.—Rio de Janeiro: IBGE, 2011.150 p
Willett W (2012) Nutritional epidemiology. Oxford University Press, Oxford
McHill AW, Phillips AJ, Czeisler CA et al (2017) Later circadian timing of food intake is associated with increased body fat. Am J Clin Nutr 106(5):1213–1219
Brasileiro I, de Geografia e Estatística, (2010) Pesquisa de Orçamentos Familiares 2008–2009—Antropometria e estado nutricional de crianças, adolescentes e adultos no Brasil. IBGE, Rio de Janeiro
Teixeira GP, Mota MC, Crispim CA (2018) Eveningness is associated with skipping breakfast and poor nutritional intake in Brazilian undergraduate students. Chronobiol Int 35(3):358–367
Monzani A, Ricotti R, Caputo M et al (2019) A systematic review of the association of skipping breakfast with weight and cardiometabolic risk factors in children and adolescents. What should we better investigate in the future? Nutrients 11(2):387
Ma X, Chen Q, Pu Y et al (2020) Skipping breakfast is associated with overweight and obesity: a systematic review and meta-analysis. Obes Res Clin Pract Jan-Feb 14(1):1–8
Palomar-Cro A, Srour B, Andreeva VA, Fezeu LK, Bellicha A, Kesse-Guyot E, Touvier M (2023) Associations of meal timing, number of eating occasions and night-time fasting duration with incidence of type 2 diabetes in the NutriNet-Santé cohort. Int J Epidemiol 2023:dyad081
Cahill LE, Chiuve SE, Mekary RA et al (2013) Prospective study of breakfast eating and incident coronary heart disease in a cohort of male US health professionals. Circ J 128(4):337–343
Kubota Y, Iso H, Sawada N, Tsugane S, JPHC Study Group (2016) Association of breakfast intake with incident stroke and coronary heart disease: the Japan Public Health Center-Based Study. Stroke 47(2):477–481
Reutrakul S, Hood MM, Crowley SJ, Morgan MK, Teodori M, Knutson KL (2014) The relationship between breakfast skipping, chronotype, and glycemic control in type 2 diabetes. Chronobiol Int 31(1):64–71
Betts JA, Richardson JD, Chowdhury EA et al (2014) The causal role of breakfast in energy balance and health: a randomized controlled trial in lean adults. The Am J Clin Nutr 100(2):539–547
Li QM, Wu CK, Ma PC et al (2022) Breakfast consumption frequency is associated with dyslipidemia: a retrospective cohort study of a working population. Lipids Health Di 21(1):1–11
Matthys C, De Henauw S, Bellemans M, De Maeyer M, De Backer G (2007) Breakfast habits affect overall nutrient profiles in adolescents. Public Health Nutr 10(4):413–421
Astbury NM, Taylor MA, Macdonald IA (2011) Breakfast consumption affects appetite, energy intake, and the metabolic and endocrine responses to foods consumed later in the day in male habitual breakfast eaters. J Nutr 141(7):1381–1389
Bonnet JP, Cardel MI, Cellini J, Hu FB, Guasch-Ferré M (2020) Breakfast skipping, body composition, and cardiometabolic risk: a systematic review and meta-analysis of randomized trials. Obesity 28(6):1098–1109
Ha K, Song Y (2019) Associations of meal timing and frequency with obesity and metabolic syndrome among Korean adults. Nutrients 11(10):2437
Poggiogalle E, Jamshed H, Peterson CM (2018) Circadian regulation of glucose, lipid, and energy metabolism in humans. Metab Clin Exp 84:11–27
Spiegel K, Leproult R, L’Hermite-Balériaux M, Copinschi G, Penev PD, Van Cauter E (2004) Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocr 89(11):5762–5771
De Castro JM (2004) The time of day of food intake influences overall intake in humans. J Nutr 134(1):104–111
Heitmann BL, Lissner L (1995) Dietary underreporting by obese individuals—Is it specific or non-specific? BMJ 311(7011):986–989
Xiao Q, Bauer C, Layne T, Playdon M (2021) The association between overnight fasting and body mass index in older adults: the interaction between duration and timing. Int J Obes 45(3):555–564
Horn C, Laupsa-Borge J, Andersen AI, Dyer L, Revheim I, Leikanger T, Dankel SN (2022) Meal patterns associated with energy intake in people with obesity. Br J Nutr 128(2):334–344
Wirth MD, Zhao L, Turner-McGrievy GM, Ortaglia A (2021) Associations between fasting duration, timing of first and last meal, and cardiometabolic endpoints in the national health and nutrition examination survey. Nutrients 13(8):2686
Popkin BM, Corvalan C, Grummer-Strawn LM (2020) Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 395(10217):65–74
Huseinovic E, Winkvist A, Freisling H et al (2019) Timing of eating across ten European countries—results from the European Prospective Investigation into Cancer and Nutrition (EPIC) calibration study. Public Health Nutr 22(2):324–335
Acknowledgements
We thank the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) and the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CAC and CRCM are CNPq fellows; CAC: #401761/2022-3 and 312309/2020-1; CRCM: #311278/2019) for financial support and the scholarship, and the University of Surrey for the IAS Fellowship to CAC in 2022.
Funding
This work was supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and the Institute of Advanced Studies (IAS) of the University of Surrey. CAC and CRCM are CNPq fellows—CAC: #401761/2022-3 and 312309/2020-1; CRCM: #311278/2019); CAC was awarded the IAS Fellowship by the University of Surrey in 2022.
Author information
Authors and Affiliations
Contributions
CAC, CRCM and DJS participated in the planning, interpretation of results and writing of the manuscript. CAC performed the statistical analysis. CMA and AEMR participated in the interpretation of results, support on the statistical analysis and writing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Crispim, C.A., Rinaldi, A.E.M., Azeredo, C.M. et al. Is time of eating associated with BMI and obesity? A population-based study. Eur J Nutr 63, 527–537 (2024). https://doi.org/10.1007/s00394-023-03282-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-023-03282-x