Abstract
Purpose
The study aimed to investigate the clinical characteristics, prognostic factors, survival times, and therapy outcomes of brain metastases (BM) from colorectal cancer (CRC).
Methods
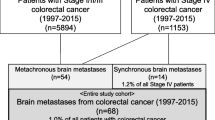
The clinical characteristics of 25 patients with BM from CRC were retrospectively analyzed. The time of the occurrence of BM after diagnosis of CRC was recorded. Meanwhile, the time from the occurrence of lung, bone, liver, and other extracranial metastases to the occurrence of BM was also recorded. We evaluate the time factors affecting the length of the occurrence of BM and the potential prognostic factors after BM diagnosis. The influences of patients undergoing surgery-based comprehensive treatment, radiotherapy-based comprehensive treatment, and co-medication were also assessed.
Results
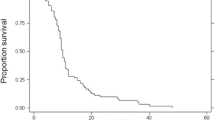
In patients with BM from CRC, lung metastases (13/25) occurred at a higher frequency than liver metastases (8/25) and bone metastases (6/25). The median time to the development of BM was much shorter (3.7 vs. 25.3 months, p = 0.027), with the brain being the origin site for the metastasis. The median overall survival reached 9.9 months. The interval between diagnosis of BM and bone, liver, and lung metastasis remains 3, 6.5, and 11 months, respectively. The brain lesions of patients with BM alone had higher rates in supratentorial (88.9%), while those with extracranial metastasis had a 62.5% incidence of infratentorial metastasis. The difference was statistically significant (p < 0.05). The time of occurrence of BM in patients aged 67 years and younger was 16.1 and 30.1 months, respectively. The differences between them were statistically significant (p = 0.043). The BM time for left- and right-sided colon cancer were 26.5 and 7.8 months, representing a statistically significant difference (p = 0.015). The time to onset of BM for patients with and without the resection of primary lesions was 25.4 and 4.5 months. Statistically significant differences are shown (p = 0.007). Univariate analysis demonstrated that the prognosis of patients was related to the KPS score, the number of BM, the treatment methods, and the occurrence of lung metastasis (p < 0.05). The multivariate analysis revealed that the treatment modality and lung metastasis were independent prognostic factors for CRC patients with BM. Right-sided CRC patients with BM have a poor prognosis (8.1 vs. 10.2 months, p = 0.31). Although median survival time was not significantly different between patients with and without bevacizumab combination therapy, bevacizumab therapy is associated with a better survival time (9.9 vs. 7.1 months, p = 0.27).
Conclusion
Patients with left-sided CRC, especially those with lung metastases, are prone to brain metastases, and patients with brain metastases as the first metastatic site have a higher rate of supratentorial metastases. Young patients with right hemicolon cancer and patients who have not undergone primary lesion resection have a shorter time for the occurrence of BM. Patients with colorectal lung metastases, especially those young with right-sided CRC, require close imaging surveillance of BM. The prognosis of CRC patients with BM and lung metastases is poor, and comprehensive treatment based on surgery could significantly prolong patients’ survival time.




Similar content being viewed by others
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Siegel RL, Wagle NS, Cercek A et al (2023) Colorectal cancer statistics, 2023. CA: Cancer J Clin 73(3):233–54. https://doi.org/10.3322/caac.21772
Sedlak JC, Yilmaz ÖH, Roper J (2023) Metabolism and colorectal cancer. Ann Rev Pathol 18:467–92. https://doi.org/10.1146/annurev-pathmechdis-031521-041113
Siegel RL, Mpller KD, Fuchs HE et al (2022) Cancer statistics, 2022. CA: Cancer J Clin 72(1):7–33. https://doi.org/10.3322/caac.21708
Cervantes A, Adam R, Roselló S et al (2023) Metastatic colorectal cancer: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Ann Oncol Off J Eur Soc Med Oncol 34(1):10–32. https://doi.org/10.1016/j.annonc.2022.10.003
Müller S, Köhler F, Hendricks A et al (2021) Brain metastases from colorectal cancer: a systematic review of the literature and meta-analysis to establish a guideline for daily treatment. Cancers 13(4). https://doi.org/10.3390/cancers13040900
Chen PC, Yeh YM, Chu CT et al (2023) HER2 amplification in colorectal cancer with brain metastasis: a propensity score matching study. Eur J Cancer (Oxford, England: 1990) 181:62–9. https://doi.org/10.1016/j.ejca.2022.12.019
Christensen TD, Palshof JA, Larsen FO et al (2017) Risk factors for brain metastases in patients with metastatic colorectal cancer. Acta oncologica (Stockholm, Sweden) 56(5):639–645. https://doi.org/10.1080/0284186x.2017.1290272
Chang Y, Wong CE, Lee PH et al (2022) Survival outcome of surgical resection vs. radiotherapy in brain metastasis from colorectal cancer: a meta-analysis. Front Med 9:768896. https://doi.org/10.3389/fmed.2022.768896
Li W, Wang T, Zhu Y et al (2022) Brain metastasis from colorectal cancer: treatment, survival, and prognosis. Medicine 101(40):e30273. https://doi.org/10.1097/md.0000000000030273
Li Y, Wu J, Liu F et al Single-fraction SRS and multiple-fraction SRT for brain metastases from colorectal cancer. Front Oncol 12:1060570. https://doi.org/10.3389/fonc.2022.1060570
Liu X, Liu Q, Wu X et al (2023) Efficacy of various adjuvant chemotherapy methods in preventing liver metastasis from potentially curative colorectal cancer: a systematic review network meta-analysis of randomized clinical trials. Cancer Med 12(3):2238–2247. https://doi.org/10.1002/cam4.5157
Cagney DN, Martin AM, Catalano PJ et al (2017) Incidence and prognosis of patients with brain metastases at diagnosis of systemic malignancy: a population-based study. Neuro Oncol 19(11):1511–1521. https://doi.org/10.1093/neuonc/nox077
Lei S, Ge Y, Tian S et al (2020) Colorectal cancer metastases to brain or bone and the relationship to primary tumor location: a population-based study. J Gastrointest Surg off J Soc Surg Aliment Tract 24(8):1833–1842. https://doi.org/10.1007/s11605-019-04308-8
Mjahed RB, Astaras C, Roth A et al (2022) Where are we now and where might we be headed in understanding and managing brain metastases in colorectal cancer patients? Curr Treat Options Oncol 23(7):980–1000. https://doi.org/10.1007/s11864-022-00982-0
Rades D, Nnguyen T, Janssen S et al (2020) An easy-to-use survival score compared to existing tools for older patients with cerebral metastases from colorectal cancer. Cancers 12(4). https://doi.org/10.3390/cancers12040833
Lu X, Cai Y, Xia L et al (2019) Treatment modalities and relative survival in patients with brain metastasis from colorectal cancer. Biosci Trends 13(2):182–188. https://doi.org/10.5582/bst.2019.01044
Bergen ES, Scherleitner P, Ferreira P et al (2021) Primary tumor side is associated with prognosis of colorectal cancer patients with brain metastases. ESMO Open 6(3):100168. https://doi.org/10.1016/j.esmoop.2021.100168
Quan J, Ma C, Sun P et al (2019) Brain metastasis from colorectal cancer: clinical characteristics, timing, survival and prognostic factors. Scand J Gastroenterol 54(11):1370–1375. https://doi.org/10.1080/00365521.2019.1686056
Gu XD, Cai YT, Zhou YM et al (2015) Prognostic factors and multidisciplinary treatment modalities for brain metastases from colorectal cancer: analysis of 93 patients. BMC Cancer 15:902. https://doi.org/10.1186/s12885-015-1933-2
Patel AR, Neddzi L, Lau S et al (2018) Neoadjuvant stereotactic radiosurgery before surgical resection of cerebral metastases. World Neurosurg 120:e480-e7. https://doi.org/10.1016/j.wneu.2018.08.107
Paix A, Antoni D, Adeduntan R et al (2017) Stereotactic radiation therapy of brain metastases from colorectal cancer: a single institution cohort. Cancer radiotherapie : journal de la Societe francaise de radiotherapie oncologique 21(3):199–204. https://doi.org/10.1016/j.canrad.2017.01.010
Kim DY, Ryu CG, Jung EJ et al (2018) Brain metastasis from colorectal cancer: a single center experience. Ann Surg Treat Res 94(1):13–18. https://doi.org/10.4174/astr.2018.94.1.13
Chen X, Momin A, Wanggou S et al (2023) Mechanosensitive brain tumor cells construct blood-tumor barrier to mask chemosensitivity. Neuron 111(1):30-48.e14. https://doi.org/10.1016/j.neuron.2022.10.007
Łazarczyk M, Mickael ME, Sliba D et al (2023) The journey of cancer cells to the brain: challenges and opportunities. Int J Mol Sci 24(4). https://doi.org/10.3390/ijms24043854
Kotecha R, Ahluwalia MS, Siomin V et al (2022) Surgery, stereotactic radiosurgery, and systemic therapy in the management of operable brain metastasis. Neurol Clin 40(2):421–436. https://doi.org/10.1016/j.ncl.2021.11.002
Perlow HK, Ho C, Matsui JK et al (2023) Comparing pre-operative versus post-operative single and multi-fraction stereotactic radiotherapy for patients with resectable brain metastases. Clin Transl Radiat Oncol 38:117–22. https://doi.org/10.1016/j.ctro.2022.11.004
Xu M, Song K, Zhou Z et al (2022) Survival and prognostic factors in patients undergoing the resection of solitary brain metastasis from non-small cell lung cancer: a retrospective cohort study. J Thorac Dis 14(10):4113–24. https://doi.org/10.21037/jtd-22-1279
Jin Z, Breen W, Jin R et al (2020) Multimodality management of brain metastasis from colorectal cancer. 38(4_suppl):204
Majd N, Simon M, Wagman R et al (2022) A rare case of colon cancer metastasis to the brain anda brief review of its treatment and prognosis. Radiol Case Rep 17(3):696–699. https://doi.org/10.1016/j.radcr.2021.11.047
Cai J, Zheng J, Shen J et al (2020) A radiomics model for predicting the response to bevacizumab in brain necrosis after radiotherapy. Clin Cancer Res An Off J Am Assoc Cancer Res 26(20):5438–5447. https://doi.org/10.1158/1078-0432.Ccr-20-1264
Garci J, Hurwitz I, Sandler AB et al (2020) Bevacizumab (Avastin®) in cancer treatment: a review of 15 years of clinical experience and future outlook. Cancer Treat Rev 86:102017. https://doi.org/10.1016/j.ctrv.2020.102017
Finkelmeier F, You SJ, Waidmann O et al (2016) Bevacizumab in combination with chemotherapy for colorectal brain metastasis. J Gastrointest Cancer 47(1):82–88. https://doi.org/10.1007/s12029-015-9795-z
Acknowledgements
We are grateful to the patients and their families for supporting the study.
Funding
The study was funded by National Project for Clinical Key Specialty Development.
Author information
Authors and Affiliations
Contributions
The first draft of the manuscript was written by Zhao Gao, and all authors commented on previous versions of the manuscript. Shikai Wu and Xuan Jin conceived of the review and edited the manuscript. Zhao Gao collected and analyzed the data. Xuan Jin analyzed the data and drafted the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study has been approved by the Ethics Committee of the Peking University First Hospital.
Consent to participate
Not required.
Consent for publication
Not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gao, Z., Jin, X. & Wu, S. Clinical features and prognostic factors of brain metastases from colorectal cancer: a single center experience. Int J Colorectal Dis 38, 198 (2023). https://doi.org/10.1007/s00384-023-04451-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-023-04451-4