Abstract
Background and aims
This study aimed to investigate the incidence and the risk factors of incidence for second primary malignancies (SPMs) onset among survivors diagnosed with colorectal cancer (CRC).
Methods
A large population-based cohort study was performed. Data of patients diagnosed with CRC was identified and extracted from 8 cancer registries of Surveillance, Epidemiology, and End Results database from January 1990 to December 2017. The outcome of interest was percentage and common sites of SPM onset after primary CRC diagnosis. The cumulative incidence and standardize incidence rates (SIRs) were also reported. Afterwards, we estimated sub-distribution hazards ratios (SHRs) and relative risks (RRs) for SPM occurrence using multivariable competing-risk and Poisson regression models, respectively.
Results
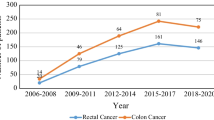
A total of 152,402 patients with CRC were included to analyze. Overall, 23,816 patients of all CRC survivors (15.6%) were reported SPM occurrence. The highest proportion of SPMs development after primary CRC diagnosis was second CRC, followed by lung and bronchus cancer among all survivors. Also, CRC survivors were more susceptible to develop second gastrointestinal cancers (GICs). Besides, pelvic cancers were analyzed with a relative high proportion among patients who received RT in comparison to those without RT. The cumulative incidence of all SPMs onset was 22.16% (95% CI: 21.82–22.49%) after near 30-year follow-up. Several factors including older age, male, married status, and localized stage of CRC were related to the high risk of SPMs onset. In treatment-specific analyses, RT was related to a higher cumulative incidence of SPMs occurrence (all SPMs: 14.08% vs. 8.72%; GICs: 2.67% vs. 2.04%; CRC: 1.01% vs. 1.57%; all p < 0.01). Furthermore, the increased risk of SPMs onset was found among patients who received RT than patients within the NRT group (SHR: 1.50, 95% CI: 1.32–1.71), p < 0.01; RR: 1.61, 95% CI: 1.45–1.79, p < 0.01).
Conclusion
The present study described the incidence pattern of SPM among CRC survivors and identified the risk factors of the SPM onset. RT treatment for patients diagnosed with CRC may increase the risk of SPMs occurrence. The findings suggest the need for long-term follow-up surveillance for these patients.





Similar content being viewed by others
Data availability
The datasets during the current study are available in SEER database.
References
Siegel RL, Miller KD, Jemal A et al (2019) Cancer statistics. CA: Cancer J Clin 69(1):7–34
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin 71(3):209–249
Siegel RL, Miller KD, Goding Sauer A et al (2020) Colorectal cancer statistics, 2020. CA: Cancer J Clin 70(3):145–164
Miller KD, Nogueira L, Devasia T et al (2022) Cancer treatment and survivorship statistics, 2022. CA: Cancer J Clin 72(5):409–436
Jayasekara H, Reece JC, Buchanan DD et al (2017) Risk factors for metachronous colorectal cancer or polyp: a systematic review and meta-analysis. J Gastroenterol Hepatol 32(2):301–326
Jayasekara H, Reece JC, Buchanan DD et al (2016) Risk factors for metachronous colorectal cancer following a primary colorectal cancer: a prospective cohort study. Int J Cancer 139(5):1081–1090
Guan X, Jin Y, Chen Y et al (2015) The incidence characteristics of second primary malignancy after diagnosis of primary colon and rectal cancer: a population based study. PLoS ONE 10(11):e0143067
Jia H, Li Q, Yuan J, Sun X, Wu Z (2020) Second primary malignancies in patients with colorectal cancer: a population-based analysis. Oncologist 25(4):e651–e658
Broman KK, Bailey CE, Parikh AA (2019) Sidedness of colorectal cancer impacts risk of second primary gastrointestinal malignancy. Ann Surg Oncol 26:2037–2043
Wu M, Huang M, He C et al (2021) Risk of second primary malignancies based on the histological subtypes of colorectal cancer. Front Oncol 11:650937
Tiritilli A, Ko C (2022) Patients with early-onset colorectal cancer have an increased risk of second primary malignancy. Dig Dis Sci 1–9
Guan X, Wei R, Yang R et al (2021) Association of radiotherapy for rectal cancer and second gynecological malignant neoplasms. JAMA Netw Open 4(1):e2031661–e2031661
He X, Wu W, Ye D, Li Y, Si J, Sun L (2018) Excessive risk of second primary cancers in young-onset colorectal cancer survivors. Cancer Med 7(4):1201–1210
Ahmed F, Goodman MT, Kosary C et al (2006) Excess risk of subsequent primary cancers among colorectal carcinoma survivors, 1975–2001. Cancer 107(S5):1162–1171
Jack A, Percy CL, Sobin L, Whelan S (2000) International classification of diseases for oncology: ICD-O: World Health Organization
Han SS, Rivera GA, Tammemägi MC et al (2017) Risk stratification for second primary lung cancer. J Clin Oncol 35(25):2893
Li Q, Lin J, Chi A, Davies S (2020) Practical considerations of utilizing propensity score methods in clinical development using real-world and historical data. Contemp Clin Trials 97:106123
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94(446):496–509
Siegel RL, Jemal A, Ward EM (2009) Increase in incidence of colorectal cancer among young men and women in the United States. Cancer Epidemiol Biomark Prev 18(6):1695–1698
Dwyer AJ, Murphy CC, Boland CR et al (2019) A summary of the fight colorectal cancer working meeting: exploring risk factors and etiology of sporadic early-age onset colorectal cancer. Gastroenterology 157(2):280–288
George A, Stead TS, Ganti L (2020) What’s the risk: differentiating risk ratios, odds ratios, and hazard ratios? Cureus 12(8)
Doubeni CA (2014) The impact of colorectal cancer screening on the US population: is it time to celebrate? (Vol. 120, pp. 2810–2813): Wiley Online Library
Kim TJ, Kim ER, Hong SN, Chang DK, Kim Y-H (2016) Long-term outcome and prognostic factors of sporadic colorectal cancer in young patients: a large institutional-based retrospective study. Medicine 95(19)
Enwerem N, Cho MY, Demb J et al (2021) Systematic review of prevalence, risk factors, and risk for metachronous advanced neoplasia in patients with young-onset colorectal adenoma. Clin Gastroenterol Hepatol 19(4):680–689.e612
Chen FW, Yang L, Cusumano VT et al (2021) Early-onset colorectal cancer is associated with a lower risk of metachronous advanced neoplasia than traditional-onset colorectal cancer. Dig Dis Sci 1–9
Kozak V, Kalady M, Gamaleldin M, Liang J, Church J (2017) Colorectal surveillance after segmental resection for young-onset colorectal cancer: is there evidence for extended resection? Colorectal Dis 19(11):O386–O392
De Gonzalez AB, Curtis RE, Kry SF et al (2011) Proportion of second cancers attributable to radiotherapy treatment in adults: a cohort study in the US SEER cancer registries. Lancet Oncol 12(4):353–360
Schairer C, Hisada M, Chen BE et al (2007) Comparative mortality for 621 second cancers in 29356 testicular cancer survivors and 12420 matched first cancers. J Natl Cancer Inst 99(16):1248–1256
Fokas E, Allgäuer M, Polat B et al (2019) Randomized phase II trial of chemoradiotherapy plus induction or consolidation chemotherapy as total neoadjuvant therapy for locally advanced rectal cancer: CAO/ARO/AIO-12. J Clin Oncol 37(34):3212–3222
Breugom A, Van Gijn W, Muller E et al (2015) Adjuvant chemotherapy for rectal cancer patients treated with preoperative (chemo) radiotherapy and total mesorectal excision: a Dutch Colorectal Cancer Group (DCCG) randomized phase III trial. Ann Oncol 26(4):696–701
Halamkova J, Kazda T, Pehalova L et al (2021) Second primary malignancies in colorectal cancer patients. Sci Rep 11(1):1–12
Zhu X, Zhou J, Zhou L, Zhang M, Gao C, Tao L (2022) Association between postoperative radiotherapy for young-onset head and neck cancer and long-term risk of second primary malignancy: a population-based study. J Transl Med 20(1):405
Selby JV, Friedman GD, Quesenberry CP Jr, Weiss NS (1992) A case–control study of screening sigmoidoscopy and mortality from colorectal cancer. N Engl J Med 326(10):653–657
Green RJ, Metlay JP, Propert K et al (2002) Surveillance for second primary colorectal cancer after adjuvant chemotherapy: an analysis of Intergroup 0089. Ann Intern Med 136(4):261–269
Teufel A, Li M, Gerken M et al (2022) Second cancer after additive chemotherapy in patients with colon cancer. Clin Colorectal Cancer 21(4):354–361
Murthy GSG, Abedin S (2019) Myeloid malignancies after treatment for solid tumours. Best Pract Res Clin Haematol 32(1):40–46
Yang J, Li S, Lv M et al (2017) Risk of subsequent primary malignancies among patients with prior colorectal cancer: a population-based cohort study. Onco Targets Ther 10:1535
Zhang B, Guo K, Zheng X, Sun L, Shen M, Ruan S (2020) Risk of second primary malignancies in colon cancer patients treated with colectomy. Front Oncol 10:1154
Donin N, Filson C, Drakaki A et al (2016) Risk of second primary malignancies among cancer survivors in the United States, 1992 through 2008. Cancer 122(19):3075–3086
Papageorge MV, Woods AP, de Geus SW et al (2022) The persistence of poverty and its impact on cancer diagnosis, treatment and survival. Ann Surg 10.1097
Acknowledgements
The authors thank the National Cancer Institute for providing the Surveillance, Epidemiology, and End Results (SEER) dataset.
Author information
Authors and Affiliations
Contributions
Conceptualization: HG. Methodology, formal analysis, and investigation: JY and FW. Data curation and writing the manuscript: JY, FW, and HA. Supervision: HG. Project administration: HG. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, J., Wu, F., An, H. et al. Incidence and risk outcomes of second primary malignancy of patients with post-operative colorectal cancer. Int J Colorectal Dis 38, 88 (2023). https://doi.org/10.1007/s00384-023-04366-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-023-04366-0