Abstract
Purpose
Nutritional and inflammatory status have been associated with postoperative recurrence and poor survival in patients with colorectal cancer. The aim of the present study is to investigate the relationship between serum cholinesterase levels and postoperative outcomes among patients who underwent curative resection for colorectal cancer.
Methods
The study comprised 174 patients who had undergone curative resection for colorectal cancer. We explored the relationship between preoperative serum cholinesterase levels and disease-free survival and overall survival after curative resection. Then patients were divided into the high-cholinesterase group (n = 102) and the low-cholinesterase group (n = 72) to analyze their clinicopathological variables including other nutritional markers and systemic inflammatory responses.
Results
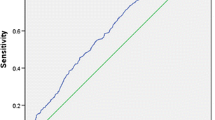
In multivariate analysis, lymph node metastasis (P = 0.011) and serum cholinesterase levels (P < 0.01) were independent predictors of disease-free survival, while lymph node metastasis (P = 0.013), serum cholinesterase levels (P < 0.01), and carbohydrate antigen19-9 (P = 0.022) were independent predictors of overall survival. In the low-cholinesterase group, neutrophil to lymphocyte ratio, (P = 0.021), C-reactive protein to albumin ratio (P < 0.01), and distant metastasis (P < 0.01) were higher, and prognostic nutritional index (P < 0.01) was lower compared with the high-cholinesterase group.
Conclusion
Preoperative low serum cholinesterase levels can be a prognostic factor for postoperative recurrence and poor prognosis in patients after curative resection for colorectal cancer, suggesting an important role of cholinesterase in the assessment of nutritional and inflammatory status in cancer patients.



Similar content being viewed by others
Availability of data and material
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASA-PS:
-
American Society of Anesthesiologists physical status
- BMI:
-
Body mass index
- CAR:
-
C-reactive protein to albumin ratio
- CA19-9:
-
Carbohydrate antigen 19–9
- CEA:
-
Carcinoembryonic antigen
- ChE:
-
Cholinesterase
- CRC:
-
Colorectal cancer
- NLR:
-
Neutrophil to lymphocyte ratio
- N.S.:
-
Not significant
- PNI:
-
Prognostic nutritional index
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:E359–E386. https://doi.org/10.1002/ijc.29210
Dienstmann R, Vermeulen L, Guinney J, Kopetz S, Tejpar S, Tabernero J (2017) Consensus molecular subtypes and the evolution of precision medicine in colorectal cancer. Nat Rev Cancer 17:79–92. https://doi.org/10.1038/nrc.2016.126
Vallribera Valls F, Landi F, Espín Basany E, Sánchez García JL, Jiménez Gómez LM, Martí Gallostra M, Salgado Cruz L, Armengol Carrasco M (2014) Laparoscopy-assisted versus open colectomy for treatment of colon cancer in the elderly: morbidity and mortality outcomes in 545 patients. Surg Endosc 28:3373–3378. https://doi.org/10.1007/s00464-014-3597-4
Riihimaki M, Hemminki A, Sundquist J, Hemminki K (2016) Patterns of metastasis in colon and rectal cancer. Sci Rep 6:29765. https://doi.org/10.1038/srep29765
Neki K, Eto K, Kosuge M, Ohkuma M, Ito D, Takeda Y, Yatabe S, Sugano H, Yanaga K (2019) Identification of the risk factors for recurrence of stage III colorectal cancer. Anticancer Res 39:5721–5724. https://doi.org/10.21873/anticanres.13772
van Gestel YR, de Hingh IH, van Herk-Sukel MP, van Erning FN, Beerepoot LV, Wijsman JH, Slooter GD, Rutten HJ, Creemers GJ, Lemmens VE (2014) Patterns of metachronous metastases after curative treatment of colorectal cancer. Cancer Epidemiol 38:448–454. https://doi.org/10.1016/j.canep.2014.04.004
Gamsjager T, Brenner L, Sitzwohl C, Weinstabl C (2008) Half-lives of albumin and cholinesterase in critically ill patients. Clin Chem Lab Med 46:1140–1142. https://doi.org/10.1515/CCLM.2008.220
Wang Y, Wang H, Chen HZ (2016) AChE Inhibition-based multi-target-directed ligands, a novel pharmacological approach for the symptomatic and disease-modifying therapy of Alzheimer’s disease. Curr Neuropharmacol 14:364–375. https://doi.org/10.2174/1570159x14666160119094820
Ramachandran J, Sajith KG, Priya S, Dutta AK, Balasubramanian KA (2014) Serum cholinesterase is an excellent biomarker of liver cirrhosis. Trop Gastroenterol 35:15–20. https://doi.org/10.7869/tg.158
Seo M, Yamada T, Tamaki S, Hikoso S, Yasumura Y, Higuchi Y, Nakagawa Y, Uematsu M, Abe H, Fuji H, Mano T, Nakatani D, Fukunami M, Sakata Y (2020) Prognostic significance of serum cholinesterase level in patients with acute decompensated heart failure with preserved ejection fraction: insights from the PURSUIT-HFpEF registry. J Am Heart Assoc 9:e014100. https://doi.org/10.1161/JAHA.119.014100
Khalil SN, Dudrick SJ, Mathieu A, Rigor BMS, Fody EP (1980) Low level of pseudocholinesterase in patient with Crohn’s disease. Lancet 2:267–268. https://doi.org/10.1016/s0140-6736(80)90160-9
Santarpia L, Grandone I, Contaldo F, Pasanisi F (2013) Butyrylcholinesterase as a prognostic marker: a review of the literature. J Cachexia Sarcopenia Muscle 2:267–268. https://doi.org/10.1007/s13539-012-0083-5
Cheng BN, Jin YL, Chen BQ, Zhu LY, Xu ZC, Shen T (2016) Serum cholinesterase: a potential assistant biomarker for hand, foot, and mouth disease caused by enterovirus 71 infection. Infect Dis Poverty 5:27-y. https://doi.org/10.1186/s40249-016-0124-y
Gu SZ, Zhao XH, Quan P, Li SB, Pan BR (2005) Alterations of serum cholinesterase in patients with gastric cancer. World J Gastroenterol 11:4604–4606. https://doi.org/10.3748/wjg.v11.i29.4604
Camarero Gonzalez E, Munoz Leira V, Iglesias Guerrero M, Fernandez Alvarez JA, Cabezas-Cerrato J (1995) Protein-energy malnutrition: its effects on 4 metabolic parameters. Nutr Hosp 10:158–160
De Simone V, Franzè E, Ronchetti G, Colantoni A, Fantini MC, Di Fusco D, Sica GS, Sileri P, MacDonald TT, Pallone F, Monteleone G, Stolfi C (2015) Th17-type cytokines, IL-6 and TNF-alpha synergistically activate STAT3 and NF-kB to promote colorectal cancer cell growth. Oncogene 34:3493–3503. https://doi.org/10.1038/onc.2014.286
Takano Y, Haruki K, Tsukihara S, Ito D, Kanno H, Son K, Eto K, Hanyu N, Ikegami T (2021) Preoperative serum cholinesterase levels as a risk factor of postoperative complications for the elderly undergoing emergency surgery. Surg Today 51:1828–1834. https://doi.org/10.1007/s00595-021-02288-4
Hayama T, Hashiguchi Y, Okada Y, Ono K, Nemoto K, Shimada R, Ozawa T, Toyoda T, Tsuchiya T, Iinuma H, Nozawa K, Matsuda K (2020) Significance of the 7th postoperative day neutrophil-to-lymphocyte ratio in colorectal cancer. Int J Colorectal Dis 35:119–124. https://doi.org/10.1007/s00384-019-03463-3
Sato R, Oikawa M, Kakita T, Okada T, Abe T, Yazawa T, Tsuchiya H, Akazawa N, Sato M, Ohira T, Harada Y, Okano H, Ito K, Tsuchiya T (2020) The prognostic value of the prognostic nutritional index and inflammation-based markers in obstructive colorectal cancer. Surg Today 50:1272–1281. https://doi.org/10.1007/s00595-020-02007-5
Matsuoka H, Ando K, Hu Q, Zaitsu Y, Tsuda Y, Hisamatsu Y, Nakashima Y, Kimura Y, Oki E, Mori M (2020) Postoperative C-reactive protein/albumin ratio is a biomarker of risk of recurrence and need for adjuvant chemotherapy for stage III colorectal cancer. Int J Clin Oncol 25:1318–1326. https://doi.org/10.1007/s10147-020-01672-3
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Benson AB 3rd, Choti MA, Cohen AM, Doroshow JH, Fuchs C, Kiel K, Martin EW Jr, McGinn C, Petrelli NJ, Posey JA, Skibber JM, Venook A, Yeatman TJ, Network NCC (2000) NCCN practice guidelines for colorectal cancer. Oncology (Williston Park) 14:203–212
Bi Y, Zhang J, Zeng D, Chen L, Ye W, Yang Q, Ling Y (2021) Cholinesterase is associated with prognosis and response to chemotherapy in advanced gastric cancer. Pathol Oncol Res 27:580800. https://doi.org/10.3389/pore.2021.580800
Mitsunaga S, Kinoshita T, Hasebe T, Nakagohri T, Konishi M, Takahashi S, Gotohda N, Ochiai A (2008) Low serum level of cholinesterase at recurrence of pancreatic cancer is a poor prognostic factor and relates to systemic disorder and nerve plexus invasion. Pancreas 36:241–248. https://doi.org/10.1097/MPA.0b013e31815b6b2b
Robinson MK, Trujillo EB, Mogensen KM, Rounds J, McManus K, Jacobs DO (2003) Improving nutritional screening of hospitalized patients: the role of prealbumin. JPEN J Parenter Enteral Nutr 27:389–395; quiz 439. https://doi.org/10.1177/0148607103027006389
Ostergaard D, Viby-Mogensen J, Hanel HK, Skovgaard LT (1988) Half-life of plasma cholinesterase. Acta Anaesthesiol Scand 32:266–269. https://doi.org/10.1111/j.1399-6576.1988.tb02727.x
Spiess A, Mikalunas V, Carlson S, Zimmer M, Craig RM (1996) Albumin kinetics in hypoalbuminemic patients receiving total parenteral nutrition. JPEN J Parenter Enteral Nutr 20:424–428. https://doi.org/10.1177/0148607196020006424
Santarpia L, Marra M, Montagnese C, Alfonsi L, Pasanisi F, Contaldo F (2009) Prognostic significance of bioelectrical impedance phase angle in advanced cancer: preliminary observations. Nutrition 25:930–931. https://doi.org/10.1016/j.nut.2009.01.015
Rokavec M, Öner MG, Li H, Jackstadt R, Jiang L, Lodygin D, Kaller M, Horst D, Ziegler PK, Schwitalla S, Slotta-Huspenina J, Bader FG, Greten FR, Hermeking H (2014) IL-6R/STAT3/miR-34a feedback loop promotes EMT-mediated colorectal cancer invasion and metastasis. J Clin Invest 124:1853–1867. https://doi.org/10.1172/JCI73531
Ye X, Wu H, Sheng L, Liu YX, Ye F, Wang M, Zhou H, Su Y, Zhang XK (2019) Oncogenic potential of truncated RXRalpha during colitis-associated colorectal tumorigenesis by promoting IL-6-STAT3 signaling. Nat Commun 10:1463–1468. https://doi.org/10.1038/s41467-019-09375-8
Author information
Authors and Affiliations
Contributions
Y. T. and K. H. developed the main concept and designed the study. Y. T., K. H., S. T., D. I., H. K., K. S., N. H., and K. E. were responsible for acquisition of clinicopathological data. Y. T. and K. H. performed data analysis and interpretation. Y. T., K. H., and K. E. drafted the manuscript. K. E. contributed to editing and critical revision for important intellectual contents.
Corresponding author
Ethics declarations
Ethics approval
The protocol for the present study was approved by the Ethics Committee of Tokyo General Hospital (No. 21–3) and it conforms to the provisions of the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Takano, Y., Haruki, K., Tsukihara, S. et al. The impact of low serum cholinesterase levels on survival in patients with colorectal cancer. Int J Colorectal Dis 37, 869–877 (2022). https://doi.org/10.1007/s00384-022-04119-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04119-5