Abstract
Purpose
The placement of self-expandable metallic stents as a bridge to surgery in malignant colon obstruction is concerning due to the long-term oncological results reported in recent published studies. The aim of this study was to evaluate the oncological consequences of stent-related perforations in patients with malignant colon obstruction and potentially curable disease.
Methods
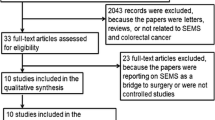
MEDLINE, Cochrane Library, Ovid and ISRCTN Registry were searched, with no restrictions. We performed five meta-analyses to estimate the pooled effect sizes by using a random-effect model. The outcomes were global, locoregional and systemic recurrence rate and 3 and 5 year-survival rate depending on the presence or absence of stent-related perforation.
Results
Thirteen studies (950 patients) were included. The overall rate of stent-related perforation was 8.9%. The global recurrence rate was significantly higher in stent-related perforation group (41.2 vs. 30.8%; OR 1.70; 95%CI: 1.02–2.84; p = 0.04). Locoregional recurrence rate was higher in the perforated group than in the non-perforated group (26.6 vs. 12.5%), with statistically significant differences (OR 2.41; 95% CI:1.33–4.34; p = 0.004). No significant differences were found in systemic recurrence rate (13.6 vs. 20.5%; OR 0.77; 95%CI: 0.35–1.7; p = 0.51); 3-year overall survival rate (65.4 vs. 74.8%; OR 0.63; 95% CI:0.29–1.39; p = 0.25) and 5-year overall survival rate (48.3 vs. 58.6%; OR 0.67; 95%CI: 0.27–1.65; p = 0.38).
Conclusion
Stent-related perforation is associated with an increased risk of global and locoregional recurrence. The successful placement of the stent as a bridge to surgery in the curative purpose of patients with obstructed colon cancer does not exclude the presence of underlying perforation, with the consequent danger of disease spread.
PROSPERO registration number: CRD42020152817







Similar content being viewed by others
Data Availability
Yes
References
National Institute for Health and Clinical Excellence (NICE). Colorectal cancer: the diagnosis and management of colorectal cancer. NICE Clinical Guideline 131; 2011. (last updated 2014)
Pisano M, Zorcolo L, Merli C, Cimbanassi S, Poiasina E, Ceresoli M, Agresta F, Allievi N, Bellanova G, Coccolini F, Coy C, Fugazzola P, Martinez CA, Montori G, Paolillo C, Penachim TJ, Pereira B, Reis T, Restivo A, Rezende-Neto J, Sartelli M, Valentino M, Abu-Zidan FM, Ashkenazi I, Bala M, Chiara O, de’ Angelis N, Deidda S, de Simone B, di Saverio S, Finotti E, Kenji I, Moore E, Wexner S, Biffl W, Coimbra R, Guttadauro A, Leppäniemi A, Maier R, Magnone S, Mefire AC, Peitzmann A, Sakakushev B, Sugrue M, Viale P, Weber D, Kashuk J, Fraga GP, Kluger I, Catena F, Ansaloni L (2018) 2017 WSES guidelines on colon and rectal cancer emergencies: obstruction and perforation. World J Emerg Surg 13:36
van Hooft JE, Van Halsema EE, Vanbiervliet G et al (2014) Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Gastrointest Endosc 80:747–761
Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M (2004) Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol 99:2051–2057
Ansaloni L, Andersson RE, Bazzoli F, Catena F, Cennamo V, di Saverio S, Fuccio L, Jeekel H, Leppäniemi A, Moore E, Pinna AD, Pisano M, Repici A, Sugarbaker PH, Tuech JJ (2010) Guidelenines in the management of obstructing cancer of the left colon: consensus conference of the world society of emergency surgery (WSES) and peritoneum and surgery (PnS) society. World J Emerg Surg 5:29
Angenete E, Asplund D, Bergström M, Park PO (2012) Stenting for colorectal cancer obstruction compared to surgery: a study of consecutive patients in a single institution. Int J Color Dis 27:665–670
Dastur JK, Forshaw MJ, Modarai B, Solkar MM, Raymond T, Parker MC (2008) Comparison of short and long-term outcomes following either insertion of self-expanding metallic stents or emergency surgery in malignant large bowel obstruction. Tech Coloproctol 12:51–55
Xu YS, Fu YF, Du HT, Li DC (2015) Palliative stent insertion for acute malignant colorectal obstruction: long-term patency and survival. Surg Laparosc Endosc Percutan Tech 25(6):500–504
Knight AL, Trompetas V, Saunders MP, Anderson HJ (2012) Does stenting of left-sided colorectal cancer as a “bridge to surgery” adversely affect oncological outcomes? A comparison with non-obstructing elective left-sided colonic resections. Int J Color Dis 27(11):1509–1514
Pessione S, Petruzzelli L, Gentilli S, Mioli P (2007) Treatment of neoplastic stenosis of the left colon: presurgical expandable metal stent vs. emergency surgery. Comparison of results and survival rates. Chir Ital 59:661–669
Pirlet IA, Slim K, Kwiatkowski F, Michot F, Millat BL (2011) Emergency preoperative stenting versus surgery for acute left-sided malignant colonic obstruction: a multicenter randomized controlled trial. Surg Endosc 25:1814–1821
van Hooft JE, Fockens MAW et al (2008) Early closure of a multicenter randomized clinical trial of endoscopic stenting versus surgery for stage IV left-sided colorectal cáncer. Endoscopy 40:184–191
van Hooft JE, Bemelman WA, Oldenburg B, Marinelli AW, Lutke Holzik MF, Grubben MJ, Sprangers MA, Dijkgraaf MG, Fockens P, collaborative Dutch Stent-In study group (2011) Colonic stenting versus emergency surgery for acute left- sided malignant colonic obstruction: a multicentre randomised trial. Lancet Oncol 12:344–352
Alcantara M, Serra-Aracil X, Falco J et al (2011) Prospective, controlled, randomized study of intraoperative colonic lavage versus stent placement. World J Surg 35(8):1904–1910
Watt AM, Faragher IG, Griffin TT, Rieger NA, Maddern GJ (2007) Self-expanding metallic stents for relieving malignant colorectal obstruction: a systematic review. Ann Surg 246:24–30
Frago R, Ramirez E, Millan M, Kreisler E, del Valle E, Biondo S (2014) Current management of acute malignant large bowel obstruction: a systematic review. Am J Surg 207:127–138
Atukorale YN, Church JL, Hoggan BL, Lambert RS, Gurgacz SL, Goodall S, Maddern GJ (2016) Self- expanding metallic stents for the management of emergency malignant large bowel obstruction: a systematic review. J Gastrointest Surg 20:455–462
Dionigi G, Villa F, Rovera F et al (2007) Colonic stenting for malignant disease: review of literature. Surg Oncol 16(suppl):S153–S155
Sagar J (2011) Colorectal stents for the management of malignant colonic obstructions. Cochrane Database Syst Rev 2011(11):CD007378
Tan CJ, Dasari BV, Gardiner K (2012) Systematic review and meta-analysis of randomized clinical trials of self-expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. Br J Surg 99:469–476
Khot UP, Lang AW, Murali K, Parker MC (2002) Systematic review of the efficacy and safety of colorectal stents. Br J Surg 89:1096–1102
Tilney HS, Lovegrove RE, Purkayastha S, Sains PS, Weston-Petrides GK, Darzi AW, Tekkis PP, Heriot AG (2007) Comparison of colonic stenting and open surgery for malignant large bowel obstruction. Surg Endosc 21:225–233
Arezzo A, Passera R, Lo Secco G, Verra M, Bonino MA, Targarona E, Morino M (2017) Stent as bridge to surgery for left-sided malignant colonic obstruction reduces adverse events and stoma rate compared with emergency surgery: results of a systematic review and meta-analysis of randomized controlled trials. Gastrointest Endosc 86:416–426
Zhang Y, Shi J, Shi B, Song CY, Xie WF, Chen YX (2012) Self-expanding metallic stent as a bridge to surgery versus emergency surgery for obstructive colorectal cancer: a meta-analysis. Surg Endosc 26(1):110–119
Ye GY, Cui Z, Chen L, Zhong M (2012) Colonic stenting vs. emergent surgery for acute left-sided malignant colonic obstruction: a systematic review and meta-analysis. World J Gastroenterol 18(39):5608–5615
Zhao RS, Wang H, Wang L et al (2012) Meta-analysis of safety and efficacy of self-expending metallic stents as bridge to surgery versus emergency surgery for left-sided malignant colorectal obstruction. Zhonghua Wei Chang Wai Ke Za Zhi 15(7):697–701
Cirocchi R, Farinella E, Trastulli S, Desiderio J, Listorti C, Boselli C, Parisi A, Noya G, Sagar J (2013) Safety and efficacy of endoscopic colonic stenting as a bridge to surgery in the management of intestinal obstruction due to left colon and rectal cancer: a systematic review and meta-analysis. Surg Oncol 22:14–21
De Ceglie A, Filiberti R, Baron TH et al (2012) A meta-analysis of endoscopic stenting as bridge to surgery versus emergency surgery for left-sided colorectal cancer obstruction. Crit Rev Oncol Hematol 88:387–403
Cennamo V, Luigiano C, Coccolini F, Fabbri C, Bassi M, de Caro G, Ceroni L, Maimone A, Ravelli P, Ansaloni L (2013) Meta-analysis of randomized trials comparing endoscopic stenting and surgical decompression for colorectal cancer obstruction. Int J Color Dis 28:855–863
Liu Z, Kang L, Li C, Huang M, Zhang X, Wang J (2014) Meta-analysis of complications of colonic stenting versus emergency surgery for acute left-sided malignant colonic obstruction. Surg Laparosc Endosc Percutan Tech 24(1):73–79
Wang X, He J, Chen X, Yang Q (2017) Stenting as a bridge to resection versus emergency surgery for left-sided colorectal cancer with malignant obstruction: a systematic review and meta-analysis. Int J Surg 48:64–68
Huang X, Lv B, Zhang S, Meng L (2014) Preoperative colonic stents versus emergency surgery for acute left-sided malignant colonic obstruction: a meta-analysis. J Gastrointest Surg 18:584–591
Allievi N, Ceresoli M, Fugazzola P et al (2017) Endoscopic stenting as bridge to surgery versus emergency resection for left-sided malignant colorectal obstruction: an updated meta-analysis. Int J Surg Oncol 2017:2863272
Amelung FJ, Burghgraef TA, Tanis PJ, van Hooft JE, ter Borg F, Siersema PD, Bemelman WA, Consten ECJ (2018) Critical appraisal of oncological safety of stent as bridge to surgery in left-sided obstructing colon cancer; a systematic review and meta-analysis. Crit Rev Oncol Hematol 131:66–75
Foo CC, Poon SHT, Chiu RHY, Lam WY, Cheung LC, Law WL (2019) Is bridge to surgery stenting a safe alternative to emergency surgery in malignant colonic obstruction: a meta-analysis of randomized control trials. Surg Endosc 33(1):293–302
Kim JS, Hur H, Min BS, Sohn SK, Cho CH, Kim NK (2009) Oncologic outcomes of self-expanding metallic stent insertion as a bridge to surgery in the management of left-sided colon cancer obstruction: comparison with nonobstructing elective surgery. World J Surg 33:1281–1286
Kim HJ, Choi GS, Park JS, Park SY, Jun SH (2013) Higher rate of perineurial invasion in stent-laparoscopic approach in comparison to emergent open resection for obstructing left-sided colon cancer. Int J Color Dis 28:407–414
Sabbagh C, Browet F, Diouf M (2013) Is stenting as “a bridge to surgery” an ontologically dafe strategy for the management of acute, left-sided, malignant, colonic obstruction? A comparative study with a propensity score analysis. Ann Surg 258:107–115
Gorissen KJ, Tuynman JB, Fryer F (2013) Local recurrence after stenting for obstructing left-sided colonic cancer. Br J Surg 100(13):1805–1809
Saida Y, Sumiyama Y, Nagao J, Uramatsu M (2003) Long-term prognosis of preoperative ‘bridge to surgery’ expandable metallic stent insertion for obstructive colorectal cancer: comparison with emergency operation. Dis Colon Rectum 46(Suppl):S44–S49
Park SJ, Lee KY, Kwon SH, Lee SH (2016) Stenting as a bridge to surgery for obstructive colon cancer: does it have surgical merit or oncologic demerit? Ann Surg Oncol 23(3):842–848
Amelung FJ, Draaisma WA, Consten ECJ, Siersema PD, ter Borg F (2017) Self-expandable metal stent placement versus emergency resection for malignant proximal colon obstructions. Surg Endosc 31(11):4532–4541
Choi JM, Lee C, Han YM, Lee M, Choi YH, Jang DK, Im JP, Kim SG, Kim JS, Jung HC (2014) Long-term oncologic outcomes of endoscopic stenting as a bridge to surgery for malignant colonic obstruction: comparison with emergency surgery. Surg Endosc 28(9):2649–2655
Erichsen R, Horváth-Puhó E, Jacobsen JB, Nilsson T, Baron JA, Sørensen HT (2015) Long-term mortality and recurrence after colorectal cancer surgery with preoperative stenting: a Danish nationwide cohort study. Endoscopy. 47(6):517–524
Flor-Lorente B, Báguena G, Frasson M et al (2017) Self-expanding metallic stent as a bridge to surgery in the treatment of left colon cancer obstruction: cost-benefit analysis and oncologic results. Cir Esp 95(3):143–151
Gibor U, Perry Z, Tirosh D, Netz U, Rosental A, Fich A, Man S, Ariad S, Kirshtein B (2017) Comparison of the long-term oncological outcomes of stent as a bridge to surgery and surgery alone in malignant colonic obstruction. Isr Med Assoc J 19(12):736–740
Ribeiro I, Pinho R, Leite M, Proença L, Silva J, Ponte A, Rodrigues J, Maciel-Barbosa J, Carvalho J (2016) Reevaluation of self-expanding metal stents as a bridge to surgery for acute left-sided malignant colonic obstruction: six years experience. GE Port J Gastroenterol 23(2):76–83
Rodrigues-Pinto E, Pereira P, Lopes S, Ribeiro A, Moutinho-Ribeiro P, Peixoto A, Macedo G (2015) Outcome of endoscopic self-expandable metal stents in acute malignant colorectal obstruction at a tertiary center. Rev Esp Enferm Dig 107(9):534–538
Kavanagh DO, Nolan B, Judge C, Hyland JMP, Mulcahy HE, O’Connell PR, Winter DC, Doherty GA (2013) A comparative study of short and medium-term outcomes comparing emergent surgery and stenting as a bridge to surgery in patients with acute malignant colonic obstruction. Dis Colon Rectum 56(4):433–440
Kwak MS, Kim WS, Lee JM, Yang DH, Yoon YS, Yu CS, Kim JC, Byeon JS (2016) Does stenting as a bridge to surgery in left-sided colorectal cancer obstruction really worsen oncological outcomes? Dis Colon Rectum 59(8):725–732
Quereshy FA, Poon JTC, Law JW (2014) Long-term outcomes of stenting as a bridge to surgery for acute left-sided malignant colonic obstruction. Color Dis 16(10):788–793
Crespí-Mir A, Romero-Marcos JM, de la Llave-Serralvo A, Dolz-Abadía C, Cifuentes-Ródenas JA (2018) Impact on surgical and oncological results of the use of colonic stents as a bridge to surgery for potentially curable occlusive colorectal neoplasms. Cir Esp 96(7):419–428
Van den Berg MW, Sloothaak DAM, Dijkgraaf MGW et al (2014) Bridge to surgery stent placement versus emergency resection for acute malignant colonic obstruction. Br J Surg 101(7):867–873
Yang SY, Park YY, Han YD, Cho MS, Hur H, Min BS, Lee KY, Kim NK (2019) Oncologic outcomes of self-expandable metallic stent as a bridge to surgery and safety and feasibility of minimally invasive surgery for acute malignant colonic obstruction. Ann Surg Oncol 26(9):2787–2796
Amelung FJ, Borstlap WAA, Consten ECJ, Veld JV, van Halsema EE, Bemelman WA, Siersema PD, ter Borg F, van Hooft JE, Tanis PJ, on behalf of the Dutch Snapshot Research Group, Algera H, Algie GD, Andeweg CS, Argillander T, Arron MNNJ, Arts K, Aufenacker THJ, Bakker IS, Basten Batenburg M, Bastiaansen AJNM, Beets GL, Berg A, Beukel B, Blom RLGM, Blomberg B, Boerma EG, Boer FC, Bouvy ND, Bouwman JE, Boye NDA, Brandt ARM, Brandsma HT, Breijer A, Broek W, Bröker MEE, Burbach JPM, Bruns ERJ, Burghgraef TA, Crolla RMPH, Dam M, Daniels L, Dekker JWT, Demirkiran A, Dongen K, Durmaz SF, Esch A, Essen JA, Foppen JW, Furnee EJB, Geloven AAW, Gerhards MF, Gorter EA, Grevenstein WMU, Groningen J, Groot I, Haak H, Haas JWA, Hagen P, Hamminga JTH, Havenga K, Hengel B, Harst E, Heemskerk J, Heeren J, Heijnen BHM, Heijnen L, Heikens JT, Heinsbergen M, Hess DA, Heuchemer N, Hoff C, Hogendoorn W, Houdijk APJ, Hugen N, Inberg B, Janssen T, Pierre DJ, Jong WJ, Jongen ACHM, Kamman AV, Klaase JM, Kelder W, Kelling EF, Klicks R, de Klein GW, Kloppenberg FWH, Konsten JLM, Koolen LJER, Kornmann V, Kortekaas RTJ, Kreiter A, Lamme B, Lange JF, Lettinga T, Lips D, Lo G, Logeman F, Loon YT, Holzik MFL, Marres CCM, Masselink I, Mearadji A, Meisen G, Menon AG, Merkus J, Mey D, Mijle HCJ, Moes DE, Molenaar C, Nieboer MJ, Nielsen K, Nieuwenhuijzen GAP, Neijenhuis PA, Oomen P, Oorschot N, Parry K, Peeters KCMJ, Paulides T, Paulusma I, Poelmann FB, Polle SW, Poortman P, Raber M, Renger RJ, Reiber BMM, Roukema R, Ruijter WMJ, Russchen MJAM, Rutten HJT, Scheerhoorn J, Scheurs S, Schippers H, Schuermans VNE, Schuijt HJ, Sierink JC, Sietses C, Silvis R, Slegt J, Slooter G, Sluis M, Sluis P, Smakman N, Smit D, Sprundel TC, Sonneveld DJA, Steur C, Straatman J, Struijs MC, Swank HA, Talsma AK, Tenhagen M, Tol JAMG, Tolenaar JL, Tseng L, Tuynman JB, Veen MJF, Veltkamp S, Ven AWH, Verkoele L, Vermaas M, Versteegh HP, Versluijs L, Visser T, Uden D, Vles WJ, Vos tot Nederveen Cappel R, Vries HS, Vugt ST, Vugts G, Wegdam JA, Weijs T, Wely BJ, Werker C, Westerterp M, Westreenen HL, Wiering B, Wijffels NAT, Wijkman AA, Wijngaarden LH, Wilt JHW, Wilt M, Wisselink DD, Wit F, Zaag ES, Zimmerman D, Zwols T (2019) Propensity score-matched analysis of oncological outcome between stent as bridge to surgery and emergency resection in patients with malignant left-sided colonic obstruction. Br J Surg 106(8):1075–1086
Sloothaak DAM, van den Berg MW, Dijkgraaf MGW, Fockens P, Tanis PJ, van Hooft JE, Bemelman WA, the collaborative Dutch Stent-In study group (2014) Oncological outcome of malignant colonic obstruction in the Dutch stent-in 2 trial. Br J Surg 101(13):1751–1757
Arezzo A, Balague C, Targarona E, Borghi F, Giraudo G, Ghezzo L, Arroyo A, Sola-Vera J, de Paolis P, Bossotti M, Bannone E, Forcignanò E, Bonino MA, Passera R, Morino M (2017) Colonic stenting as a bridge to surgery versus emergency surgery for malignant colonic obstruction: results of a multicentre randomised controlled trial (ESCO trial). Surg Endosc 31(8):3297–3305
Ghazal AH, El-Shazly WG, Bessa SS et al (2013) Colonic endolumenal stenting devices and elective surgery versus emergency subtotal/total colectomy in the management of malignant obstructed left colon carcinoma. J Gastrointest Surg 17(6):1123–1129
Tung KL, Cheung HY, Ng LW et al (2013) Endo-laparoscopic approach versus conventional open surgery in the treatment of obstructing left-sided colon cancer: long-term follow-up of a randomized trial. Asian J Endosc Surg 6(2):78–81
van Halsema EE, van Hooft JE, Small AJ et al (2014) Perforation in colorectal stenting: a meta-analysis and a search for risk factors. Gastrointest Endosc 79(6):970–983.e5
Fryer E, Gorissen KJ, Wang LM, Guy R, Chetty R (2015) Spectrum of histopathological changes encountered in stented colorectal carcinomas. Histopathology. 66(4):480–484
Honore C, Goere D, Souadka A et al (2013) Definition of patients presenting a high risk of developing peritoneal carcinomatosis after curative surgery for colorectal cancer: a systematic review. Ann Surg Oncol 20:183–192
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):e1–e34
Bowne WB, Lee B, Wong WD et al (2005) Operative salvage for locoregional recurrent colon cancer after curative resection: an analysis of 100 cases. Dis Colon Rectum 48(5):897–909
Sterne JAC, Hernan MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919
Avlund TH, Erichsen R, Ravn S, Ciplys Z, Andersen JC, Laurberg S, Iversen LH (2018) The prognostic impact of bowel perforation following self-expanding metal stent as a bridge to surgery in colorectal cancer obstruction. Surg Endosc 32(1):328–336
Kim SJ, Kim HW, Park SB, Kang DH, Choi CW, Song BJ, Hong JB, Kim DJ, Park BS, Son GM (2015) Colonic perforation either during or after stent insertion as a bridge to surgery for malignant colorectal obstruction increases the risk of peritoneal seeding. Surg Endosc 29(12):3499–3506
Verstockt B, Van Driessche A, De Man M et al (2018) Ten-year survival after endoscopic stent placement as a bridge to surgery in obstructing colon cancer. Gastrointest Endosc 87(3):705–713.e2
Zanghi A, Piccolo G, Cavallaro A et al (2016) A pilot study about the oncologic safety of colonic self-expandable metal stents (SEMS) in obstructive colon cancer: is occlusion always better than “silent” perforation? Eur Rev Med Pharmacol Sci 20(24):5242–5248
Higgins JPT, Green S (editors) (2019) Cochrane Handbook for Systematic Reviews of Interventions version 6 [updated July 2019]. The Cochrane Collaboration. Available from https://training.cochrane.org/handbooks. Accessed 15 Sept 2019
Egger M, Davey SG, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Maruthachalam K, Lash GE, Bk S et al (2007) Tumour cell disemination following endoscopic stent insertion. Br J Surg 94:1151–1154
Suarez J, Jimenez-Perez J (2016) Long-term outcomes after stenting as a “bridge to surgery” for the management of acute obstruction secondary to colorectal cáncer. World J Gastrointest Oncol 8:105–112
Yamashita S, Tanemura M, Sawada G, Moon J, Shimizu Y, Yamaguchi T, Kuwai T, Urata Y, Kuraoka K, Hatanaka N, Yamashita Y, Taniyama K (2018) Impact of endoscopic stent insertion on detection of viable circulating tumor cells from obstructive colorectal cancer. Oncol Lett 15(1):400–406
Takahashi G, Yamada T, Iwai T, Takeda K, Koizumi M, Shinji S, Uchida E (2018) Oncological assessment of stent placement for obstructive colorectal cancer from circulating cell-free DNA and circulating tumor DNA dynamics. Ann Surg Oncol 25(3):737–744
Steinert EM, Schwartz RH, Singh NJ (2012) At low precursor frequencies, the T-cell response to chronic self-antigen results in anergy without deletion. Eur J Immunol 42(11):2875–2880
Lemoine L, Sugarbaker P, Van der Speeten K (2016) Pathophysiology of colorectal peritoneal carcinomatosis. Role of peritoneum. World J Gastroenterol 22:7692–7707
Hayashi K, Jiang P, Yamauchi K, Yamamoto N, Tsuchiya H, Tomita K, Moossa AR, Bouvet M, Hoffman RM (2007) Real-time imaging of tumour-cell shedding and trafficking in lymphatic channels. Cancer Res 67:8223–8228
Manes G, de Bellis M, Fucsia L et al (2011) Endoscopic palliation in patients with incurable malignant colorectal obstruction by means of self-expanding metal stent: analysis of results and predictors of outcomes in a large multi center series. Arch Surg 146(10):1157–1162
Malgras B, Brulle L, Lo Dico R et al (2015) Insertion of a stent in obstructive colon cancer can induce a metastatic process in an experimental murine model. Ann Surg Oncol 22(Suppl 3):S1475–S1480
Baron TH, Dean PA, Yates MR 3rd et al (1998) Expandable metal stents for the treatment of colonic obstruction: techniques and outcomes. Gastrointest Endosc 47(3):277–286
Small AJ, Coelho-Prabhu N, Baron TH (2010) Endoscopic placement of self-expandable metal stents for malignant colonic obstruction: long-term outcomes and complication factors. Gastrointest Endosc 71(3):560–572
Pacheco-Barcia V, Mondéjar R, Martínez-Sáez O, Longo F, Moreno JA, Rogado J, Donnay O, Santander C, Carrato A, Colomer R (2019) Safety and oncological outcomes of bevacizumab therapy in patients with advanced colorectal cancer and self-expandable metal stents. Clin Colorectal Cancer 18(3):e287–e293
Binkert CA, Ledermann H, Jost R et al (1996) Acute colonic obstruction: clinical aspects and cost-effectiveness of preoperative and palliative treatment with self-expanding metallic stents – a preliminary report. Radiology 206(1):199–204
Camunez F, Echenagusia A, Simo G et al (2000) Colorectal obstruction treated by means of self-expanding metallic stents: effectiveness before surgery and in palliation. Radiology 216(2):492–497
Sabbagh C, Chatelain D, Trouillet N, Mauvais F, Bendjaballah S, Browet F, Regimbeau JM (2013) Does use of a metallic colon stent as a bridge to surgery modify the pathology data in patients with colonic obstruction? A case-matched study. Surg Endosc 27(10):3622–3631
Author information
Authors and Affiliations
Contributions
Study conception design, data acquisition and data analysis and interpretation: Izaskun Balciscueta, Zutoia Balciscueta and Natalia Uribe.
Drafting the article and critical revision: Izaskun Balciscueta, Zutoia Balciscueta and Natalia Uribe.
Final approval of the manuscript: Izaskun Balciscueta, Zutoia Balciscueta, Natalia Uribe and Eduardo García-Granero.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Balciscueta, I., Balciscueta, Z., Uribe, N. et al. Long-term outcomes of stent-related perforation in malignant colon obstruction: a systematic review and meta-analysis. Int J Colorectal Dis 35, 1439–1451 (2020). https://doi.org/10.1007/s00384-020-03664-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03664-1