Abstract
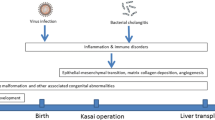
Biliary atresia (BA) is a severe cholangiopathy in infants. It is characterized by inflammatory fibro-obliteration of the intra- and extrahepatic bile ducts. Although the restoration of bile flow can be successful after Kasai operation, the rapid progression of liver fibrosis can continue, leading to cirrhosis. It is believed that the progression of liver fibrosis in BA is exacerbated by complicated mechanisms other than the consequence of bile duct obstruction. The fibrogenic cascade in BA liver can be divided into three stages, including liver inflammatory injury, myofibroblast activation, and fibrous scar formation. Recent studies have revealed that the activation of an immune response following bile duct injury plays an important role in promoting the inflammatory process, the releasing of inflammatory cytokines, and the development of fibrogenesis in BA liver. In this article, we summarized the evidence regarding liver inflammatory injury and the possible mechanisms that explain the rapid progression of liver fibrosis in BA.


Similar content being viewed by others
Data availability
The data used to support the findings of this study are included within the article.
References
Bezerra JA, Wells RG, Mack CL et al (2018) Biliary atresia: clinical and research challenges for the twenty-first century. Hepatology 68:1163–1173. https://doi.org/10.1002/hep.29905
Chung PHY, Zheng S, Tam PKH (2020) Biliary atresia: East versus west. Semin Pediatr Surg 29:150950. https://doi.org/10.1016/j.sempedsurg.2020.150950
Jimenez-Rivera C, Jolin-Dahel KS, Fortinsky KJ et al (2013) International incidence and outcomes of biliary atresia. J Pediatr Gastroenterol Nutr 56:344–354. https://doi.org/10.1097/MPG.0b013e318282a913
Nio M, Ohi R, Miyano T et al (2003) Five- and 10-year survival rates after surgery for biliary atresia: a report from the Japanese biliary atresia registry. J Pediatr Surg 38:997–1000. https://doi.org/10.1016/S0022-3468(03)00178-7
Wada H, Muraji T, Yokoi A et al (2007) Insignificant seasonal and geographical variation in incidence of biliary atresia in Japan: a regional survey of over 20 years. J Pediatr Surg 42:2090–2092. https://doi.org/10.1016/j.jpedsurg.2007.08.035
Lin Y-C, Chang M-H, Liao S-F et al (2011) Decreasing rate of biliary atresia in Taiwan: a survey, 2004–2009. Pediatrics 128:e530-536. https://doi.org/10.1542/peds.2011-0742
Lee KJ, Kim JW, Moon JS, Ko JS (2017) Epidemiology of biliary atresia in Korea. J Korean Med Sci 32:656–660. https://doi.org/10.3346/jkms.2017.32.4.656
Livesey E, Borja MC, Sharif K et al (2009) Epidemiology of biliary atresia in England and Wales (1999–2006). Arch Dis Child - Fetal Neonatal Ed 94:F451–F455. https://doi.org/10.1136/adc.2009.159780
Chardot C, Buet C, Serinet M-O et al (2013) Improving outcomes of biliary atresia: French national series 1986–2009. J Hepatol 58:1209–1217. https://doi.org/10.1016/j.jhep.2013.01.040
Hopkins PC, Yazigi N, Nylund CM (2017) Incidence of biliary atresia and timing of hepatoportoenterostomy in the United States. J Pediatr 187:253–257. https://doi.org/10.1016/j.jpeds.2017.05.006
Schreiber RA, Barker CC, Roberts EA et al (2007) Biliary atresia: the Canadian experience. J Pediatr 151(659–665):665.e1. https://doi.org/10.1016/j.jpeds.2007.05.051
Asai A, Miethke A, Bezerra JA (2015) Pathogenesis of biliary atresia: defining biology to understand clinical phenotypes. Nat Rev Gastroenterol Hepatol 12:342–352. https://doi.org/10.1038/nrgastro.2015.74
Davenport M, Muntean A, Hadzic N (2021) Biliary atresia: clinical phenotypes and aetiological heterogeneity. J Clin Med 10:5675. https://doi.org/10.3390/jcm10235675
Lendahl U, Lui VCH, Chung PHY, Tam PKH (2021) Biliary atresia – emerging diagnostic and therapy opportunities. EBioMedicine 74:103689. https://doi.org/10.1016/j.ebiom.2021.103689
Bijl EJ, Bharwani KD, Houwen RHJ, de Man RA (2013) The long-term outcome of the Kasai operation in patients with biliary atresia: a systematic review. Neth J Med 71:170–173
Kasahara M, Umeshita K, Sakamoto S et al (2017) Liver transplantation for biliary atresia: a systematic review. Pediatr Surg Int 33:1289–1295. https://doi.org/10.1007/s00383-017-4173-5
Hukkinen M, Ruuska S, Pihlajoki M et al (2021) Long-term outcomes of biliary atresia patients surviving with their native livers. Best Pract Res Clin Gastroenterol. https://doi.org/10.1016/j.bpg.2021.101764
Parola M, Pinzani M (2019) Liver fibrosis: pathophysiology, pathogenetic targets and clinical issues. Mol Aspects Med 65:37–55. https://doi.org/10.1016/j.mam.2018.09.002
Hukkinen M, Pihlajoki M, Pakarinen MP (2020) Predicting native liver injury and survival in biliary atresia. Semin Pediatr Surg 29:150943. https://doi.org/10.1016/j.sempedsurg.2020.150943
Shen W-J, Chen G, Wang M, Zheng S (2019) Liver fibrosis in biliary atresia. World J Pediatr 15:117–123. https://doi.org/10.1007/s12519-018-0203-1
Mack CL (2007) The pathogenesis of biliary atresia: evidence for a virus-induced autoimmune disease. Semin Liver Dis 27:233–242. https://doi.org/10.1055/s-2007-985068
Ortiz-Perez A, Donnelly B, Temple H et al (2020) Innate immunity and pathogenesis of biliary atresia. Front Immunol 11:329. https://doi.org/10.3389/fimmu.2020.00329
Antala S, Taylor SA (2022) Biliary atresia in children: update on disease mechanism, therapies, and patient outcomes. Clin Liver Dis 26:341–354. https://doi.org/10.1016/j.cld.2022.03.001
Udomsinprasert W, Ungsudechachai T, Vejchapipat P et al (2022) Systemic cytokine profiles in biliary atresia. PLoS ONE 17:e0267363. https://doi.org/10.1371/journal.pone.0267363
Kerola A, Lampela H, Lohi J et al (2017) Molecular signature of active fibrogenesis prevails in biliary atresia after successful portoenterostomy. Surgery 162:548–556. https://doi.org/10.1016/j.surg.2017.04.013
Marvie P, Lisbonne M, L’helgoualc’h A et al (2010) Interleukin-33 overexpression is associated with liver fibrosis in mice and humans. J Cell Mol Med 14:1726–1739. https://doi.org/10.1111/j.1582-4934.2009.00801.x
Shteyer E, Ramm GA, Xu C et al (2006) Outcome after portoenterostomy in biliary atresia: pivotal role of degree of liver fibrosis and intensity of stellate cell activation. J Pediatr Gastroenterol Nutr 42:93–99. https://doi.org/10.1097/01.mpg.0000189324.80323.a6
Suominen JS, Heikkil HL, Auml I, Jouko Lohi HJ (2014) Myofibroblastic cell activation and neovascularization predict native liver survival and development of esophageal varices in biliary atresia. World J Gastroenterol 20:3312–3319. https://doi.org/10.3748/wjg.v20.i12.3312
Díaz R, Kim JW, Hui J-J et al (2008) Evidence for the epithelial to mesenchymal transition in biliary atresia fibrosis. Hum Pathol 39:102–115. https://doi.org/10.1016/j.humpath.2007.05.021
Deng Y-H, Pu C-L, Li Y-C et al (2011) Analysis of biliary epithelial-mesenchymal transition in portal tract fibrogenesis in biliary atresia. Dig Dis Sci 56:731–740. https://doi.org/10.1007/s10620-010-1347-6
Omenetti A, Bass LM, Anders RA et al (2011) Hedgehog activity, epithelial-mesenchymal transitions, and biliary dysmorphogenesis in biliary atresia. Hepatol Baltim Md 53:1246–1258. https://doi.org/10.1002/hep.24156
Xiao Y, Zhou Y, Chen Y et al (2015) The expression of epithelial-mesenchymal transition-related proteins in biliary epithelial cells is associated with liver fibrosis in biliary atresia. Pediatr Res 77:310–315. https://doi.org/10.1038/pr.2014.181
Low Y, Vijayan V, Tan CE (2001) The prognostic value of ductal plate malformation and other histologic parameters in biliary atresia: an immunohistochemical study. J Pediatr 139:320–322. https://doi.org/10.1067/mpd.2001.117003
Shimadera S, Iwai N, Deguchi E et al (2008) Significance of ductal plate malformation in the postoperative clinical course of biliary atresia. J Pediatr Surg 43:304–307. https://doi.org/10.1016/j.jpedsurg.2007.10.023
Arii R, Koga H, Arakawa A et al (2011) How valuable is ductal plate malformation as a predictor of clinical course in postoperative biliary atresia patients? Pediatr Surg Int 27:275–277. https://doi.org/10.1007/s00383-010-2793-0
Vuković J, Grizelj R, Bojanić K et al (2012) Ductal plate malformation in patients with biliary atresia. Eur J Pediatr 171:1799–1804. https://doi.org/10.1007/s00431-012-1820-7
Mukhopadhyay SG, Roy P, Chatterjee U et al (2014) A histopathological study of liver and biliary remnants in the long-term survivors (>10 years) of cases of biliary atresia. Indian J Pathol Microbiol 57:380–385. https://doi.org/10.4103/0377-4929.138722
Safwan M, Ramachandran P, Vij M et al (2015) Impact of ductal plate malformation on survival with native liver in children with biliary atresia. Pediatr Surg Int 31:837–843. https://doi.org/10.1007/s00383-015-3728-6
Russo P, Magee JC, Anders RA et al (2016) Key histopathologic features of liver biopsies that distinguish biliary atresia from other causes of infantile cholestasis and their correlation with outcome: a multicenter study. Am J Surg Pathol 40:1601–1615. https://doi.org/10.1097/PAS.0000000000000755
Nguyen A-HP, Pham YHT, Vu GH et al (2021) Biliary atresia liver histopathological determinants of early post-Kasai outcome. J Pediatr Surg 56:1169–1173. https://doi.org/10.1016/j.jpedsurg.2021.03.039
Santos JL, Kieling CO, Meurer L et al (2009) The extent of biliary proliferation in liver biopsies from patients with biliary atresia at portoenterostomy is associated with the postoperative prognosis. J Pediatr Surg 44:695–701. https://doi.org/10.1016/j.jpedsurg.2008.09.013
Lampela H, Kosola S, Heikkilä P et al (2014) Native liver histology after successful portoenterostomy in biliary atresia. J Clin Gastroenterol 48:721–728. https://doi.org/10.1097/MCG.0000000000000013
Null G, Sirait DN, Budiarti LR et al (2020) Histopathological findings for prediction of liver cirrhosis and survival in biliary atresia patients after Kasai procedure. Diagn Pathol 15:79. https://doi.org/10.1186/s13000-020-00996-y
El-Araby HA, Saber MA, Radwan NM et al (2021) Temporal histopathological changes in biliary atresia: a perspective for rapid fibrosis progression. Ann Hepatol 21:100263. https://doi.org/10.1016/j.aohep.2020.09.007
Moyer K, Kaimal V, Pacheco C et al (2010) Staging of biliary atresia at diagnosis by molecular profiling of the liver. Genome Med 2:33. https://doi.org/10.1186/gm154
Webb NL, Jiwane A, Ooi CY et al (2017) Clinical significance of liver histology on outcomes in biliary atresia. J Paediatr Child Health 53:252–256. https://doi.org/10.1111/jpc.13371
Desmet VJ (1992) Congenital diseases of intrahepatic bile ducts: variations on the theme “ductal plate malformation.” Hepatol Baltim Md 16:1069–1083. https://doi.org/10.1002/hep.1840160434
Sato K, Marzioni M, Meng F et al (2019) Ductular reaction in liver diseases: pathological mechanisms and translational significances. Hepatol Baltim Md 69:420–430. https://doi.org/10.1002/hep.30150
Banales JM, Huebert RC, Karlsen T et al (2019) Cholangiocyte pathobiology. Nat Rev Gastroenterol Hepatol 16:269–281. https://doi.org/10.1038/s41575-019-0125-y
Fabris L, Spirli C, Cadamuro M et al (2017) Emerging concepts in biliary repair and fibrosis. Am J Physiol - Gastrointest Liver Physiol 313:G102–G116. https://doi.org/10.1152/ajpgi.00452.2016
Zagory JA, Nguyen MV, Wang KS (2015) Recent advances in the pathogenesis and management of biliary atresia. Curr Opin Pediatr 27:389–394. https://doi.org/10.1097/MOP.0000000000000214
Mavila N, James D, Shivakumar P et al (2014) Expansion of PROMININ-1-expressing cells in association with fibrosis of biliary atresia. Hepatol Baltim Md 60:941–953. https://doi.org/10.1002/hep.27203
Mack CL, Tucker RM, Sokol RJ et al (2004) Biliary atresia is associated with CD4+ Th1 cell-mediated portal tract inflammation. Pediatr Res 56:79–87. https://doi.org/10.1203/01.PDR.0000130480.51066.FB
Ohya T, Fujimoto T, Shimomura H, Miyano T (1995) Degeneration of intrahepatic bile duct with lymphocyte infiltration into biliary epithelial cells in biliary atresia. J Pediatr Surg 30:515–518. https://doi.org/10.1016/0022-3468(95)90120-5
Kobayashi H, Puri P, O’Briain DS et al (1997) Hepatic overexpression of MHC class II antigens and macrophage-associated antigens (CD68) in patients with biliary atresia of poor prognosis. J Pediatr Surg 32:590–593. https://doi.org/10.1016/s0022-3468(97)90714-4
Urushihara N, Iwagaki H, Yagi T et al (2000) Elevation of serum interleukin-18 levels and activation of Kupffer cells in biliary atresia. J Pediatr Surg 35:446–449. https://doi.org/10.1016/s0022-3468(00)90211-2
Davenport M, Gonde C, Redkar R et al (2001) Immunohistochemistry of the liver and biliary tree in extrahepatic biliary atresia. J Pediatr Surg 36:1017–1025. https://doi.org/10.1053/jpsu.2001.24730
Asselah T, Marcellin P, Bedossa P (2014) Improving performance of liver biopsy in fibrosis assessment. J Hepatol 61:193–195. https://doi.org/10.1016/j.jhep.2014.03.006
Wang Y, Hou J-L (2015) Current strategies for quantitating fibrosis in liver biopsy. Chin Med J (Engl) 128:252–258. https://doi.org/10.4103/0366-6999.149223
Huang Y, de Boer WB, Adams LA et al (2013) Image analysis of liver collagen using sirius red is more accurate and correlates better with serum fibrosis markers than trichrome. Liver Int Off J Int Assoc Study Liver 33:1249–1256. https://doi.org/10.1111/liv.12184
Longo-Santos LR, Teodoro WR, de Mello ES et al (2016) Early type I collagen deposition is associated with prognosis in biliary atresia. J Pediatr Surg 51:379–385. https://doi.org/10.1016/j.jpedsurg.2015.08.061
Ramachandran P, Unny AK, Vij M et al (2019) α-Smooth muscle actin expression predicts the outcome of Kasai portoenterostomy in biliary atresia. Saudi J Gastroenterol Off J Saudi Gastroenterol Assoc 25:101–105. https://doi.org/10.4103/sjg.SJG_242_18
Babu RO, Lui VCH, Chen Y et al (2020) Beta-amyloid deposition around hepatic bile ducts is a novel pathobiological and diagnostic feature of biliary atresia. J Hepatol 73:1391–1403. https://doi.org/10.1016/j.jhep.2020.06.012
Amarachintha SP, Mourya R, Ayabe H et al (2022) Biliary organoids uncover delayed epithelial development and barrier function in biliary atresia. Hepatology 75:89–103. https://doi.org/10.1002/hep.32107
Chen S, Li P, Wang Y et al (2020) Rotavirus infection and cytopathogenesis in human biliary organoids potentially recapitulate biliary atresia development. MBio 11:e01968-e2020. https://doi.org/10.1128/mBio.01968-20
Chu AS, Russo PA, Wells RG (2012) Cholangiocyte cilia are abnormal in syndromic and non-syndromic biliary atresia. Mod Pathol Off J US Can Acad Pathol Inc 25:751–757. https://doi.org/10.1038/modpathol.2011.212
Frassetto R, Parolini F, Marceddu S et al (2018) Intrahepatic bile duct primary cilia in biliary atresia. Hepatol Res Off J Jpn Soc Hepatol 48:664–674. https://doi.org/10.1111/hepr.13060
Lam W-Y, Tang CS-M, So M-T et al (2021) Identification of a wide spectrum of ciliary gene mutations in nonsyndromic biliary atresia patients implicates ciliary dysfunction as a novel disease mechanism. EBioMedicine 71:103530. https://doi.org/10.1016/j.ebiom.2021.103530
Hartley JL, Davenport M, Kelly DA (2009) Biliary atresia. Lancet 374:1704–1713. https://doi.org/10.1016/S0140-6736(09)60946-6
Feldman AG, Mack CL (2012) Biliary atresia: cellular dynamics and immune dysregulation. Semin Pediatr Surg 21:192–200. https://doi.org/10.1053/j.sempedsurg.2012.05.003
Mack CL, Feldman AG, Sokol RJ (2012) Clues to the etiology of bile duct injury in biliary atresia. Semin Liver Dis 32:307–316. https://doi.org/10.1055/s-0032-1329899
Nomden M, Beljaars L, Verkade HJ et al (2020) Current concepts of biliary atresia and matrix metalloproteinase-7: a review of literature. Front Med 7:617261. https://doi.org/10.3389/fmed.2020.617261
Trussoni CE, O’Hara SP, LaRusso NF (2022) Cellular senescence in the cholangiopathies: a driver of immunopathology and a novel therapeutic target. Semin Immunopathol 44:527–544. https://doi.org/10.1007/s00281-022-00909-9
Riepenhoff-Talty M, Gouvea V, Evans MJ et al (1996) Detection of group C rotavirus in infants with extrahepatic biliary atresia. J Infect Dis 174:8–15. https://doi.org/10.1093/infdis/174.1.8
Tyler KL, Sokol RJ, Oberhaus SM et al (1998) Detection of reovirus RNA in hepatobiliary tissues from patients with extrahepatic biliary atresia and choledochal cysts. Hepatol Baltim Md 27:1475–1482. https://doi.org/10.1002/hep.510270603
Rauschenfels S, Krassmann M, Al-Masri AN et al (2009) Incidence of hepatotropic viruses in biliary atresia. Eur J Pediatr 168:469–476. https://doi.org/10.1007/s00431-008-0774-2
Schukfeh N, Al-Gamrah A, Petersen C, Kuebler JF (2012) Detection of hepatotropic viruses has no impact on the prognosis after Kasai procedure. J Pediatr Surg 47:1828–1832. https://doi.org/10.1016/j.jpedsurg.2012.04.024
Xu Y, Yu J, Zhang R et al (2012) The perinatal infection of cytomegalovirus is an important etiology for biliary atresia in China. Clin Pediatr (Phila) 51:109–113. https://doi.org/10.1177/0009922811406264
Drut R, Drut RM, Gómez MA et al (1998) Presence of human papillomavirus in extrahepatic biliary atresia. J Pediatr Gastroenterol Nutr 27:530–535. https://doi.org/10.1097/00005176-199811000-00007
Mahjoub F, Shahsiah R, Ardalan FA et al (2008) Detection of Epstein Barr virus by chromogenic in situ hybridization in cases of extra-hepatic biliary atresia. Diagn Pathol 3:19. https://doi.org/10.1186/1746-1596-3-19
Mohanty SK, Donnelly B, Temple H, Tiao GM (2019) A rotavirus-induced mouse model to study biliary atresia and neonatal cholestasis. In: Vinken M (ed) Experimental cholestasis research. Springer, New York, NY, pp 259–271
Petersen C, Madadi-Sanjani O (2018) Role of viruses in biliary atresia: news from mice and men. Innov Surg Sci 3:101–106. https://doi.org/10.1515/iss-2018-0009
Fu M, Lin Z, Lin H, et al (2018) A Silver Nanoparticle Method for Ameliorating Biliary Atresia Syndrome in Mice. J Vis Exp JoVE 58158. https://doi.org/10.3791/58158
Alvarez F (2013) Is biliary atresia an immune mediated disease? J Hepatol 59:648–650. https://doi.org/10.1016/j.jhep.2013.06.006
Mohanty SK, Lobeck I, Donnelly B et al (2020) Rotavirus reassortant-induced murine model of liver fibrosis parallels human biliary atresia. Hepatol Baltim Md 71:1316–1330. https://doi.org/10.1002/hep.30907
Squires JE, Shivakumar P, Mourya R et al (2015) Natural killer cells promote long-term hepatobiliary inflammation in a low-dose rotavirus model of experimental biliary atresia. PLoS ONE 10:e0127191. https://doi.org/10.1371/journal.pone.0127191
Shivakumar P, Campbell KM, Sabla GE et al (2004) Obstruction of extrahepatic bile ducts by lymphocytes is regulated by IFN-gamma in experimental biliary atresia. J Clin Invest 114:322–329. https://doi.org/10.1172/JCI21153
Allen SR, Jafri M, Donnelly B et al (2007) Effect of rotavirus strain on the murine model of biliary atresia. J Virol 81:1671–1679. https://doi.org/10.1128/JVI.02094-06
Mohanty SK, Donnelly B, Bondoc A et al (2013) Rotavirus replication in the cholangiocyte mediates the temporal dependence of murine biliary atresia. PLoS ONE 8:e69069. https://doi.org/10.1371/journal.pone.0069069
Mack CL, Tucker RM, Sokol RJ, Kotzin BL (2005) Armed CD4+ Th1 effector cells and activated macrophages participate in bile duct injury in murine biliary atresia. Clin Immunol Orlando Fla 115:200–209. https://doi.org/10.1016/j.clim.2005.01.012
Mack CL, Tucker RM, Lu BR et al (2006) Cellular and humoral autoimmunity directed at bile duct epithelia in murine biliary atresia. Hepatology 44:1231–1239. https://doi.org/10.1002/hep.21366
Shivakumar P, Sabla GE, Whitington P et al (2009) Neonatal NK cells target the mouse duct epithelium via Nkg2d and drive tissue-specific injury in experimental biliary atresia. J Clin Invest 119:2281–2290. https://doi.org/10.1172/jci38879
Feldman AG, Tucker RM, Fenner EK et al (2013) B cell deficient mice are protected from biliary obstruction in the rotavirus-induced mouse model of biliary atresia. PLoS ONE 8:e73644. https://doi.org/10.1371/journal.pone.0073644
Si X, Chen J, Huang L (2021) RRV-induced biliary atresia in neonatal mice involves CD8 + T lymphocyte killer cells and the Notch signaling pathway. Genes Genomics 43:1289–1299. https://doi.org/10.1007/s13258-021-01153-5
Klemann C, Schröder A, Dreier A et al (2016) Interleukin 17, produced by γδ T cells, contributes to hepatic inflammation in a mouse model of biliary atresia and is increased in livers of patients. Gastroenterology 150:229-241.e5. https://doi.org/10.1053/j.gastro.2015.09.008
Mohanty SK, Donnelly B, Temple H et al (2021) T-bet deficiency attenuates bile duct injury in experimental biliary atresia. Cells 10:3461. https://doi.org/10.3390/cells10123461
Shivakumar P, Sabla G, Mohanty S et al (2007) Effector role of neonatal hepatic CD8+ lymphocytes in epithelial injury and autoimmunity in experimental biliary atresia. Gastroenterology 133:268–277. https://doi.org/10.1053/j.gastro.2007.04.031
Wang J, Xu Y, Chen Z et al (2020) Liver immune profiling reveals pathogenesis and therapeutics for biliary atresia. Cell 183:1867-1883.e26. https://doi.org/10.1016/j.cell.2020.10.048
Guo X, Xu Y, Luo W et al (2021) Programmed cell death protein-1 (PD-1) protects liver damage by suppressing IFN-γ expression in T cells in infants and neonatal mice. BMC Pediatr 21:317. https://doi.org/10.1186/s12887-021-02794-x
Erickson N, Mohanty SK, Shivakumar P et al (2008) Temporal-spatial activation of apoptosis and epithelial injury in murine experimental biliary atresia. Hepatol Baltim Md 47:1567–1577. https://doi.org/10.1002/hep.22229
Funaki N, Sasano H, Shizawa S et al (1998) Apoptosis and cell proliferation in biliary atresia. J Pathol 186:429–433. https://doi.org/10.1002/(SICI)1096-9896(199812)186:4%3c429::AID-PATH195%3e3.0.CO;2-6
Madadi-Sanjani O, Bohlen G, Wehrmann F et al (2021) Increased serum levels of activated caspases in murine and human biliary atresia. J Clin Med 10:2718. https://doi.org/10.3390/jcm10122718
Chusilp S, Lee C, Li B et al (2020) A novel model of injured liver ductal organoids to investigate cholangiocyte apoptosis with relevance to biliary atresia. Pediatr Surg Int 36:1471–1479. https://doi.org/10.1007/s00383-020-04765-2
Chusilp S, Lee C, Li B et al (2021) Human amniotic fluid stem cells attenuate cholangiocyte apoptosis in a bile duct injury model of liver ductal organoids. J Pediatr Surg 56:11–16. https://doi.org/10.1016/j.jpedsurg.2020.09.043
Zhang S, Goswami S, Ma J et al (2019) CD4+T cell subset profiling in biliary atresia reveals ICOS- regulatory T cells as a favorable prognostic factor. Front Pediatr 7:279. https://doi.org/10.3389/fped.2019.00279
Zhang J, Luo Y, Feng M, Xia Q (2021) Identification of liver immune microenvironment-related hub genes in liver of biliary atresia. Front Pediatr 9:786422. https://doi.org/10.3389/fped.2021.786422
Pang X, Cao J, Chen S et al (2021) Unsupervised clustering reveals distinct subtypes of biliary atresia based on immune cell types and gene expression. Front Immunol 12:720841. https://doi.org/10.3389/fimmu.2021.720841
Yang C, Xing H, Tan B, Zhang M (2022) Immune characteristics in biliary atresia based on immune genes and immune cell infiltration. Front Pediatr 10:902571. https://doi.org/10.3389/fped.2022.902571
Mack CL, Falta MT, Sullivan AK et al (2007) Oligoclonal expansions of CD4+ and CD8+ T-cells in the target organ of patients with biliary atresia. Gastroenterology 133:278–287. https://doi.org/10.1053/j.gastro.2007.04.032
Kotb MA, El Henawy A, Talaat S et al (2005) Immune-mediated liver injury: prognostic value of CD4+, CD8+, and CD68+ in infants with extrahepatic biliary atresia. J Pediatr Surg 40:1252–1257. https://doi.org/10.1016/j.jpedsurg.2005.05.007
Funding
This work was supported by the Canadian Institutes of Health Research (CIHR) Foundation under Grant No. 353857.
Author information
Authors and Affiliations
Contributions
SC: conception and design, drafting and revising the manuscript, final approval of the manuscript. FB: drafting and revising the manuscript, final approval of the manuscript. BL, PV: conception and design, final approval of the manuscript. AP: conception and design, drafting and revising the manuscript, final approval of the manuscript.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chusilp, S., Balsamo, F., Li, B. et al. Development of liver inflammatory injury in biliary atresia: from basic to clinical research. Pediatr Surg Int 39, 207 (2023). https://doi.org/10.1007/s00383-023-05489-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05489-9