Abstract
Background
Primary spontaneous pneumothorax (PSP) commonly occurs in lean, tall, male children and adolescents. To reduce recurrence rates of PSP, chemical pleurodesis could be helpful for patients undergoing video-assisted thoracoscopic surgery (VATS) wedge bullectomy. The efficacy and safety of intraoperative OK-432 (Picibanil) pleurodesis on preventing the recurrence of PSP in pediatric patients remain unclear.
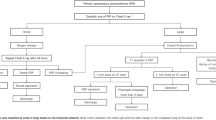
Methods
It is a retrospective observational study in a single center, between 2014 and 2020, enrolled 48 (8 females) pediatric PSP patients with persistent air leakage at the mean age of 16.3 ± 1.1 years to receive VATS wedge bullectomy and pleural abrasion. Twenty patients received additional intraoperative OK-432 pleurodesis. The clinical characteristics of patients, surgical outcomes, and recurrence rates were analyzed.
Results
The OK-432 group had longer operation time (118.6 ± 35.6 vs. 96.5 ± 23.3 min; p < 0.05) and higher proportion of postoperative fever (75.0% vs. 28.5%; p = 0.015) than the standard group. No serious adverse events were noted and other surgical outcomes in the two groups were comparable. After a mean follow-up period of 18.1 ± 19.1 months, the OK-432 group had a lower recurrence rate compared with the standard group (5% vs. 28.6%; p < 0.05, odds ratio 0.13, 95% confidence interval: 0.01–1.15), but it had no significant difference in statistics on the Kaplan–Meier curves (log-rank p = 0.105).
Conclusion
It was the first study that focused on the addition of intraoperative OK-432 pleurodesis for PSP with persistent air leakage in children and adolescents receiving VATS. It demonstrated the efficacy with a low recurrence rate and short-term safety as a single-center experience.
Level of evidence
Retrospective review, therapeutic study, Level III.


Similar content being viewed by others
Data availability
All data pertaining to this study are available upon justified request through the author in correspondence.
Abbreviations
- PSP:
-
Primary spontaneous pneumothorax
- VATS:
-
Video-assisted thoracoscopic surgery
- KE:
-
Klinische Einheit
- NRS:
-
Numeric Rating Scale
References
Sahn SA, Heffner JE (2000) Spontaneous pneumothorax. New Engl J Med 342:868–874
MacDuff A, Arnold A, Harvey J (2010) Management of spontaneous pneumothorax: British thoracic society pleural disease guideline 2010. Thorax 65:ii18-31
Sedrakyan A, van der Meulen J, Lewsey J, Treasure T (2004) Video assisted thoracic surgery for treatment of pneumothorax and lung resections: systematic review of randomised clinical trials. BMJ 329:1008
Sawada S, Watanabe Y, Moriyama S (2005) Video-assisted thoracoscopic surgery for primary spontaneous pneumothorax: evaluation of indications and long-term outcome compared with conservative treatment and open thoracotomy. Chest 127:2226–2230
Muramatsu T, Nishii T, Takeshita S, Ishimoto S, Morooka H, Shiono M (2010) Preventing recurrence of spontaneous pneumothorax after thoracoscopic surgery: a review of recent results. Surg Today 40:696–699
Ling ZG, Wu YB, Ming MY, Cai SQ, Chen YQ (2015) The effect of pleural abrasion on the treatment of primary spontaneous pneumothorax: a systematic review of randomized controlled trials. PLoS ONE 10:e0127857
Mithiran H, Leow L, Ong K et al (2019) Video-assisted thoracic surgery (VATS) talc pleurodesis versus pleurectomy for primary spontaneous pneumothorax: a large single-centre study with no conversion. World J Surg 43:2099–2105
How CH, Hsu HH, Chen JS (2013) Chemical pleurodesis for spontaneous pneumothorax. J Formos Med Assoc 112:749–755
Kishi K, Homma S, Sakamoto S et al (2004) Efficacious pleurodesis with OK-432 and doxorubicin against malignant pleural effusions. Eur Respir J 24:263–266
Ogawa K, Takahashi Y, Murase K et al (2018) OK-432 pleurodesis for the treatment of pneumothorax in patients with interstitial pneumonia. Respir Investig 56:410–417
Choi SY, Kim YH, Jo KH et al (2013) Video-assisted thoracoscopic surgery for primary spontaneous pneumothorax in children. Pediatr Surg Int 29:505–509
Wilson PM, Rymeski B, Xu X, Hardie W (2021) An evidence-based review of primary spontaneous pneumothorax in the adolescent population. J Am Coll Emerg Physicians Open 2:e12449
Huang H, Ji H, Tian H (2015) Risk factors for recurrence of primary spontaneous pneumothorax after thoracoscopic surgery. Biosci Trends 9:193–197
Feller-Kopman D, Light R (2018) Pleural disease. N Engl J Med 378:1754
Sudduth CL, Shinnick JK, Geng Z, McCracken CE, Clifton MS, Raval MV (2017) Optimal surgical technique in spontaneous pneumothorax: a systematic review and meta-analysis. J Surg Res 210:32–46
How CH, Hsu HH, Chen JS (2019) Effects of picibanil as sclerosing agent in primary spontaneous pneumothorax patient after thoracoscopic procedures. Video-assist Thorac Surg 4:16
Shinno Y, Kage H, Chino H et al (2018) Old age and underlying interstitial abnormalities are risk factors for development of ARDS after pleurodesis using limited amount of large particle size talc. Respirology 23:55–59
Kishi K, Homma S, Sakamoto S et al (2003) High efficacy of pleurodesis using OK-432 for controlling intractable pneumothorax associated with pulmonary lymphangioleiomyomatosis. Nihon Kokyuki Gakkai Zasshi 41:704–707
Taniguchi Y, Haruki T, Fujioka S, Adachi Y, Miwa K, Nakamura H (2008) Pulmonary lymphangioleiomyomatosis with concomitant tuberous sclerosis complex diagnosed by video-assisted thoracoscopic surgery. Gen Thorac Cardiovasc Surg 56:81–84
How CH, Tsai TM, Kuo SW et al (2014) Chemical pleurodesis for prolonged postoperative air leak in primary spontaneous pneumothorax. J Formos Med Assoc 113:284–290
Ukale V, Agrenius V, Widström O, Hassan A, Hillerdal G (2004) Inflammatory parameters after pleurodesis in recurrent malignant pleural effusions and their predictive value. Respir Med 98:1166–1172
Ogasawara T, Umezawa H, Kato S, Yano T, Kasamatsu N, Hashizume I (2012) Intrathoracic administration of OK-432 elevates the serum procalcitonin levels. Intern Med 51:2727–2731
Morimoto Y, Takei H, Tachibana K et al (2018) Risk factors for chest pain and fever in patients undergoing pleurodesis with OK-432. Intern Med 57:1697–1702
Acknowledgements
The authors would like to express their deepest gratitude to all the people who participated in this study. Our heartfelt thanks goes to the hospital officials for their guidance and support for this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Data curation: HH. Investigation: HH and Y-HL. Resources: HH, PC-YC, N-LW, and J-CS. Writing—original draft: HH and Y-HL. Writing—review and editing: HH, Y-HL, and PC-YC. Critical revision: HH.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflict of interest.
Studies with human participants
This study was conducted under the Declaration of Helsinki and was approved by the Institutional Review Board of MacKay Memorial Hospital, Taipei, Taiwan (approval number: 21MMHIS404e).
Informed consent
Informed consent was obtained from the patient included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, H., Lin, YH., Chang, P.CY. et al. Intraoperative OK-432 pleurodesis for preventing recurrence of primary spontaneous pneumothorax in children and adolescents: a single-center experience. Pediatr Surg Int 39, 66 (2023). https://doi.org/10.1007/s00383-022-05347-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-022-05347-0