Abstract
Purpose
To maintain safe intrarenal pelvic pressure (IPP), the combination of flexible ureteroscope (fURS) and traditional ureteral access sheath (T-UAS) should maintain a basic rule that is the ratio of endoscope-sheath diameter (RESD) ≤ 0.75. However, the negative-pressure ureteral access sheath (NP-UAS) may break the rule of negative pressure suction. This study aimed to examine the effect of NP-UAS on IPP and flow rate (FR) with varying RESD.
Methods
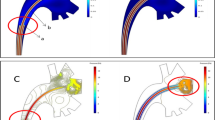
In a 3D-printed renal model, flexible ureteroscopy lithotripsy (fURL) was replicated. Six sizes of fURS paired with 12Fr T-UAS and NP-UAS resulted in six distinct RESDs of 0.63, 0.78, 0.87, 0.89, 0.90, and 0.91. While the irrigation pressure (IRP) was set between 100 and 800 cmH2O and the sucking pressure (SP) was set between 0 and 800 cmH2O, the IPP and FR were measured in each RESD.
Results
NP-UASs can reduce the IPP and increase the FR at the same RESD compared to T-UASs. The IPP decreased with increasing SP with NP-UAS. When RESD ≤ 0.78, T-UAS and NP-UAS can maintain IPP < 40 cmH2O in most circumstances. When RESD = 0.87, it is challenging for T-UAS to sustain IPP < 40 cmH2O; however, NP-UAS can do so. When RESD ≥ 0.89, it is difficult to maintain an IPP < 40 cmH2O even with NP-UAS.
Conclusion
NP-UAS can decrease IPP and increase FR compared with T-UAS. To maintain a safe IPP, it is recommended that RESD < 0.85 when utilizing NP-UAS.


Similar content being viewed by others
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Skolarikos A, Neisius A, Petřík A et al (2022) EAU guidelines on urolithiasis. https://uroweb.org/guidelines/urolithiasis
De Coninck V, Keller EX, Somani B et al (2020) Complications of ureteroscopy: a complete overview. World J Urol 38(9):2147–2166. https://doi.org/10.1007/s00345-019-03012-1
Tokas T, Herrmann TRW, Skolarikos A, Nagele U (2019) Pressure matters: intrarenal pressures during normal and pathological conditions, and impact of increased values to renal physiology. World J Urol 37(1):125–131. https://doi.org/10.1007/s00345-018-2378-4
Tracy CR, Ghareeb GM, Paul CJ, Brooks NA (2018) Increasing the size of ureteral access sheath during retrograde intrarenal surgery improves surgical efficiency without increasing complications. World J Urol 36(6):971–978. https://doi.org/10.1007/s00345-018-2204-z
Azhar RA, Alghamdi MM, Khawaji AA et al (2022) Effective ureteral access sheath insertion during flexible ureteroscopy: influence of the ureteral orifice configuration. Can Urol Assoc J 16(7):E375–E380. https://doi.org/10.5489/cuaj.7656
Kaplan AG, Lipkin ME, Scales CD, Preminger GM (2016) Use of ureteral access sheaths in ureteroscopy. Nat Rev Urol 13(3):135–140. https://doi.org/10.1038/nrurol.2015.271
Li W, Mao Y, Gu Y et al (2021) Is 10/12 Fr ureteral access sheath more suitable for flexible ureteroscopic lithotripsy? Urol J, 19(2):89–94. https://doi.org/10.22037/uj.v18i.6620
Fang L, Xie G, Zheng Z et al (2019) The effect of ratio of endoscope-sheath diameter on intrapelvic pressure during flexible ureteroscopic lasertripsy. J Endourol 33(2):132–139. https://doi.org/10.1089/end.2018.0774
Wang D, Han Z, Bi Y et al (2022) Comparison of intrarenal pressure between convention and vacuum-assisted ureteral access sheath using an ex vivo porcine kidney model. World J Urol 40(12):3055–3060. https://doi.org/10.1007/s00345-022-04149-2
Chen Y, Li C, Gao L et al (2022) Novel flexible vacuum-assisted ureteral access sheath can actively control intrarenal pressure and obtain a complete stone-free status. J Endourol 36(9):1143–1148. https://doi.org/10.1089/end.2022.0004
Zhu Z, Cui Y, Zeng F et al (2019) Comparison of suctioning and traditional ureteral access sheath during flexible ureteroscopy in the treatment of renal stones. World J Urol 37(5):921–929. https://doi.org/10.1007/s00345-018-2455-8
Yue G, Dou S, Cai C et al (2023) A novel distal active flexible vacuum-assisted ureteric access sheath in retrograde intrarenal surgery. Urology 179:204–205. https://doi.org/10.1016/j.urology.2023.06.009
Lih E, Park K, Chun SY et al (2016) Biomimetic porous PLGA scaffolds incorporating decellularized extracellular matrix for kidney tissue regeneration. ACS Appl Mater Interfaces 8(33):21145–21154. https://doi.org/10.1021/acsami.6b03771
Sierra A, Corrales M, Kolvatzis M, Doizi S, Traxer O (2022) Real time intrarenal pressure control during flexible ureterorrenscopy using a vascular pressurewire: pilot study. J Clin Med. https://doi.org/10.3390/jcm12010147
Sierra A, Corrales M, Kolvatzis M et al (2022) Real time intrarenal pressure control during flexible ureterorrenscopy using a vascular pressurewire: pilot study. J Clin Med 12:147. https://doi.org/10.3390/jcm12010147
Malhotra SK, Khaitan A, Goswami AK et al (2001) Monitoring of irrigation fluid absorption during percutaneous nephrolithotripsy: the use of 1% ethanol as a marker. Anaesthesia 56(11):1103–1106. https://doi.org/10.1046/j.1365-2044.2001.01962-3.x
Croghan SM, Skolarikos A, Jack GS et al (2023) Upper urinary tract pressures in endourology: a systematic review of range, variables and implications. BJU Int 131(3):267–279. https://doi.org/10.1111/bju.15764
Rehman J, Monga M, Landman J et al (2003) Characterization of intrapelvic pressure during ureteropyeloscopy with ureteral access sheaths. Urology 61(4):713–718. https://doi.org/10.1016/s0090-4295(02)02440-8
Wright A, Williams K, Somani B, Rukin N (2015) Intrarenal pressure and irrigation flow with commonly used ureteric access sheaths and instruments. Cent Eur J Urol 68(4):434–438. https://doi.org/10.5173/ceju.2015.604
Hendlin K, Weiland D, Monga M (2008) Impact of irrigation systems on stone migration. J Endourol 22(3):453–458. https://doi.org/10.1089/end.2007.0260
Wu ZH, Liu TZ, Wang XH et al (2020) Negative-pressure ureteroscopic holmium-YAG laser lithotripsy for ureteral stones. Urol Int 104:752–757. https://doi.org/10.1159/000507266
Funding
Ningbo Top Medical and Health Research Program (No.2022020203). The funding is not supported by any company. All author is not belonged to the company.
Author information
Authors and Affiliations
Contributions
JS: Project development, Data Collection, Data analysis, Manuscript writing. TH: Model design, Data Collection. BS: Data analysis. WL: Data Collection. YC: Data analysis. LF: Project development, Manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shi, J., Huang, T., Song, B. et al. The optimal ratio of endoscope-sheath diameter with negative-pressure ureteral access sheath: an in vitro research. World J Urol 42, 122 (2024). https://doi.org/10.1007/s00345-024-04815-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00345-024-04815-7