Abstract
Objective
This study aimed to prove the vacuum-assisted ureteral access sheath (vaUAS) is more effective in maintaining a lower IRP than conventional ureteral access sheath (cUAS).
Materials
The model consisted of 12 freshly harvested adult porcine kidneys.
Methods
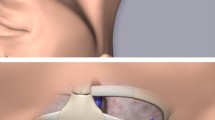
Either a 12/14F cUAS or vaUAS was alternately inserted into the ureter to one cm below the renal pelvis. Upper, middle, and lower calyces were punctured, and 6F pressure monitor catheters were introduced. IRP with cUAS was monitored using various irrigation rates. IRP with vaUAS was monitored with the same irrigation rates; various aspiration pressures; and vent fully closed, 50% closed, and fully open.
Results
cUAS with irrigation rate of 50 cc/min resulted in IRP < 30 mmHg. 50 to 100 cc/min should be used with caution. When irrigation rate exceeded 100 cc/min, IRP rose to ≥ 30 mmHg in most instances. With vent closed, vaUAS with vacuum pressure ≥ 150 mmHg and irrigation rate of 50 cc, 100 cc, and 150 cc/min generally resulted in IRPs < 5 mmHg. With vent half closed, vaUAS with vacuum pressure ≥ 300 mmHg and irrigation rate of ≤ 100 cc/min avoided IRP > 30 mmHg. vaUAS with vent open showed limited advantages over cUAS.
Conclusion
vaUAS maintains lower IRP than cUAS under same parameters. Both vaUAS and cUAS can be used when irrigation is ≤ 50 cc/min vaUAS showed clear advantages over cUAS in maintaining lower pressure when irrigation rate is ≥ 100 cc/min.


Similar content being viewed by others
References
Türk C, Petřík A, Sarica K et al (2016) EAU guidelines on interventional treatment for urolithiasis. Eur Urol 69(3):475–482
Assimos D, Krambeck A, Miller NL et al (2016) Surgical management of stones: American Urological Association/Endourological Society Guideline. PART II J Urol 196(4):1161–1169
Aboumarzouk O, Monga M, Kata SG et al (2012) Flexible ureteroscopy and laser lithotripsy for stones >2 cm: a systematic review and meta-analysis. J Endourol 26(10):1257–1263
Hinman F, Redewill FH (1926) Pyelovenous back flow. J Am Med Assoc 87(16):1287–1293
Boccafoschi C, Lugnani F (1985) Intra-renal reflux. Urol Res 13(5):253–258
Jung HU, Frimodt-Moller PC, Osther PJ et al (2006) Pharmacological effect on pyeloureteric dynamics with a clinical perspective: a review of the literature. Urol Res 34(6):341–350
Kukreja RA, Desai MR, Sabnis RB et al (2002) Fluid absorption during percutaneous nephrolithotomy: does it matter? J Endourol 16(4):221–224
Stenberg A, Bohman SO, Morsing P et al (1988) Back-leak of pelvic urine to the blood stream. Acta Physiol Scand 134(2):223–234
Cao Z, Yu W, Li W et al (2015) Oxidative damage and mitochondrial injuries are induced by various irrigation pressures in rabbit models of mild and severe hydronephrosis. PLoS One 10(6):e0127143
Boddy SA, Nimmon CC, Jones S et al (1989) Irrigation and acute ureteric dilation—as for ureteroscopy. Br J Urol 63(1):11–13
Cao Z, Yu W, Li W et al (2013) Acute kidney injuries induced by various irrigation pressure in rat models of mild and severe hydronephrosis. Urology 82(6):1453–1459
Shao Y, Shen ZJ, Zhu YY et al (2012) Fluid electrolytes and renal pelvic pressure changes during ureteroscopic lithotripsy. Min Invas Ther Allied Techol MITAT 21(4):302–306
Fang L, Xie GH, Zheng Z et al (2019) The effect of ratio of endoscope-sheath diameter on intrapelvic pressure during flexible ureteroscopic lasertripsy. J Endourol 33(2):132–139
Monga M, Best S, Venkatesh R et al (2004) Prospective randomized comparison of 2 ureteral access sheaths during flexible retrograde ureteroscopy. J Urol 172(2):572–573
Monga M, Bodie J, Ercole B (2004) Is there a role for small-diameter ureteral access sheaths? Impact on irrigant flow and intrapelvic pressures. Urology 64(3):439–441 (discussion 441-442)
Wright A, Williams K, Somani B, Rukin N (2015) Intrarenal pressure and irrigation flow with commonly used ureteric access sheaths and instruments. Central Eur J Urol 68(4):434–438
Auge BK, Pietrow PK, Lallas CD et al (2004) Ureteral access sheath provides protection against elevated renal pressures during routine flexible ureteroscopic stone manipulation. J Endourol 18(1):33–36
Wilson WT, Preminger GM (1990) Intrarenal pressures generated during flexible deflectable ureterorenoscopy. J Endourol 4:135–141
Jung H, Osther PJS (2015) Intraluminal pressure profiles during flexible ureterorenoscopy. Springerplus 4:373–380
Thomsen HS, Larsen S, Talner LB (1982) Pyelorenal backflow during retrograde pyelography in normal and ischemic porcine kidneys. A radiologic and pathoanatomic study. Eur Urol 8(5):291–297
Thomsen HS, Dorph S, Larsen S et al (1983) Intrarenal backflow and renal perfusion during increased intrapelvic pressure in excised porcine kidneys. Acta Radio Diagn 24(4):327–336
Schwalb DM, Eshghi M, Davidian M et al (1993) Morphological and physiological changes in the urinary tract associated with ureteral dilation and ureteropyeloscopy: an experimental study. J Urol 149(6):1576–1585
Noureldin YA, Kallidonis P, Ntasiotis P et al (2019) The effect of irrigation power and ureteral access sheath diameter on the maximal intra-pelvic pressure during ureteroscopy: in vivo experimental study in a live anesthetized pig. J Endourol 33(9):725–729
Fung LC, Atala A (1998) Constant elevation in renal pelvic pressure induces an increase in urinary N-acetyl-β-d-glucosaminidase in a nonobstructive porcine model. J Urol 159(1):212–216
Rehman J, Monga M, Landman J et al (2003) Characterization of intrapelvic pressure during ureteropyeloscopy with ureteral access sheaths. Urology 61(4):713–718
Yoshida T, Inoue T, Abe T et al (2018) Evaluation of intrapelvic pressure when using small-sized ureteral access sheaths of ≤10/12Fr in an ex vivo porcine kidney model. J Endourol 32(12):1142–1147
Acknowledgements
The authors want to thank Professor Shaw P. Wan, MD. for his input and editing the English for this manuscript.
Author information
Authors and Affiliations
Contributions
HX designed the experiment and wrote the manuscript. DW and ZH performed the experiments and wrote the manuscript. YB and GM contributed to data collection. GX and QH did data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors of this study disclose no conflicts of interest. There was no funded for this study.
Informed consent
This research used commercially acquired animal parts (porcine kidneys). There was no live animal involved. This research was reviewed and approved by the Institutional Ethics Committees of all the institutions involved in this study. None of the participating institutions has Animals Care and Use Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, D., Han, Z., Bi, Y. et al. Comparison of intrarenal pressure between convention and vacuum-assisted ureteral access sheath using an ex vivo porcine kidney model. World J Urol 40, 3055–3060 (2022). https://doi.org/10.1007/s00345-022-04149-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-022-04149-2