Abstract
Objectives
The experience of thermal ablation of lung lesions is limited, especially performing the procedure under localisation by cone-beam CT in the hybrid operation room (HOR). Here, we present the experience of microwave ablation (MWA) of lung nodules in the HOR.
Methods
We reviewed patients who underwent image-guide percutaneous MWA for lung nodules in the HOR under general anaesthesia between July 2020 and July 2022. The workflow in the HOR including the pre-procedure preparation, anaesthesia consideration, operation methods, and postoperative care was clearly described.
Results
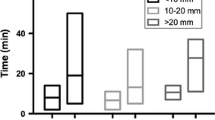
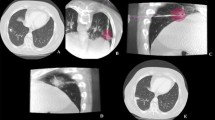
Forty lesions in 33 patients who underwent MWA under general anaesthesia (GA) in the HOR were analysed. Twenty-seven patients had a single pulmonary nodule, and the remaining six patients had multiple nodules. The median procedure time was 41.0 min, and the median ablation time per lesion was 6.75 min. The median global operation room time was 115.0 min. The median total dose area product was 14881 μGym2. The median ablation volume was 111.6 cm3. All patients were discharged from the hospital with a median postoperative stay of 1 day. Four patients had pneumothorax, two patients had pleural effusion during the first month of outpatient follow-up, and one patient reported intercostal neuralgia during the 3-month follow-up.
Conclusions
Thermal ablation of pulmonary nodules under GA in the HOR can be performed safely and efficiently if we follow the workflow provided. The procedure provides an alternative to managing pulmonary nodules in patients.
Clinical relevance statement
Thermal ablation of pulmonary nodules under GA in the HOR can be performed safely and efficiently if the provided workflow is followed.
Key Points
• We tested the feasibility of microwave ablation of lung lesions performed in a hybrid operating room.
• To this end, we provide a description of microwave ablation of the lung under cone-beam CT localisation.
• We describe a workflow by which ablation of the pulmonary nodule can be performed safely under general anaesthesia.



Similar content being viewed by others
Abbreviations
- CBCT:
-
Cone-beam computed tomography
- DAP:
-
Dose area product
- GA:
-
General anaesthesia
- GGN:
-
Ground-glass nodules
- HOR:
-
Hybrid operating room
- MWA:
-
Microwave ablation
- RFA:
-
Radiofrequency ablation
References
National Lung Screening Trial Research Team (2011) Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 365:395–409
de Koning HJ, van der Aalst CM, de Jong PA et al (2020) Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med 382:503–513
Ettinger DS, Wood DE, Aisner DL et al (2021) NCCN guidelines insights: non-small cell lung cancer, Version 2.2021. J Natl Compr Canc Netw 19:254–266
Gould MK, Donington J, Lynch WR et al (2013) Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 143:e93S-e120S
Moyer VA, U.S. Preventive Services Task Force (2014) Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 160:330–338
MacMahon H, Naidich DP, Goo JM et al (2017) Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology 284:228–243
Postmus PE, Kerr KM, Oudkerk M et al (2017) Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 28:iv1–iv21
Donahoe LL, Nguyen ET, Chung TB et al (2016) CT-guided microcoil VATS resection of lung nodules: a single-centre experience and review of the literature. J Thorac Dis 8:1986–1994
Huang YH, Chen KC, Chen JS (2019) Ultrasound for intraoperative localization of lung nodules during thoracoscopic surgery. Ann Transl Med 7:37
Ko WC, Lee YF, Chen YC et al (2016) CT-guided percutaneous microwave ablation of pulmonary malignant tumors. J Thorac Dis 8:S659–S665
Bhatia S, Pereira K, Mohan P, Narayanan G, Wangpaichitr M, Savaraj N (2016) Radiofrequency ablation in primary non-small cell lung cancer: what a radiologist needs to know. Indian J Radiol Imaging 26:81–91
Chockalingam A, Konstantinidis M, Koo B et al (2022) Surgical resection, radiotherapy and percutaneous thermal ablation for treatment of stage 1 non-small cell lung cancer: protocol for a systematic review and network meta-analysis. BMJ Open 12:e057638
Palussiere J, Catena V, Buy X (2017) Percutaneous thermal ablation of lung tumors - radiofrequency, microwave and cryotherapy: where are we going? Diagn Interv Imaging 98:619–625
Li G, Xue M, Chen W, Yi S (2018) Efficacy and safety of radiofrequency ablation for lung cancers: a systematic review and meta-analysis. Eur J Radiol 100:92–98
Healey TT, March BT, Baird G, Dupuy DE (2017) Microwave ablation for lung neoplasms: a retrospective analysis of long-term results. J Vasc Interv Radiol 28:206–211
Knavel EM, Brace CL (2013) Tumor ablation: common modalities and general practices. Tech Vasc Interv Radiol 16:192–200
Bailey CW, Sydnor MK Jr (2019) Current state of tumor ablation therapies. Dig Dis Sci 64:951–958
Alexander ES, Dupuy DE (2013) Lung cancer ablation: technologies and techniques. Semin Intervent Radiol 30:141–150
Abtin FG, Eradat J, Gutierrez AJ, Lee C, Fishbein MC, Suh RD (2012) Radiofrequency ablation of lung tumors: imaging features of the postablation zone. Radiographics 32:947–969
Mouli SK, Kurilova I, Sofocleous CT, Lewandowski RJ (2017) The role of percutaneous image-guided thermal ablation for the treatment of pulmonary malignancies. AJR Am J Roentgenol 209:740–751
Lencioni R, de Baere T, Martin RC, Nutting CW, Narayanan G (2015) Image-guided ablation of malignant liver tumors: recommendations for clinical validation of novel thermal and non-thermal technologies - a western perspective. Liver Cancer 4:208–214
Ng CSH, Krimsky WS, Yasufuku K (2021) Editorial: The hybrid operating room in modern thoracic surgery. Front Surg 8:725897
Yang SM, Chung WY, Ko HJ et al (2022) Single-stage augmented fluoroscopic bronchoscopy localization and thoracoscopic resection of small pulmonary nodules in a hybrid operating room. Eur J Cardiothorac Surg 63:ezac541
Spenkelink IM, Heidkamp J, Futterer JJ, Rovers MM (2022) Image-guided procedures in the hybrid operating room: a systematic scoping review. PLoS One 17:e0266341
Harrison OJ, Sarvananthan S, Tamburrini A, Peebles C, Alzetani A (2021) Image-guided combined ablation and resection in thoracic surgery for the treatment of multiple pulmonary metastases: a preliminary case series. JTCVS Tech 9:156–162
Ye X, Fan W, Wang Z et al (2022) Clinical practice guidelines on image-guided thermal ablation of primary and metastatic lung tumors (2022 edition). J Cancer Res Ther 18:1213–1230
Tomiyama N, Yasuhara Y, Nakajima Y et al (2006) CT-guided needle biopsy of lung lesions: a survey of severe complication based on 9783 biopsies in Japan. Eur J Radiol 59:60–64
Lee SM, Park CM, Lee KH, Bahn YE, Kim JI, Goo JM (2014) C-arm cone-beam CT-guided percutaneous transthoracic needle biopsy of lung nodules: clinical experience in 1108 patients. Radiology 271:291–300
Liu Y, Wu K, Xu K, Tian C, Jiao D, Han X (2022) Cone beam computed tomography-guided microwave ablation for hepatocellular carcinoma under the hepatic dome: a retrospective case-control study. Quant Imaging Med Surg 12:4837–4851
Cicenia J, Bhadra K, Sethi S, Nader DA, Whitten P, Hogarth DK (2021) Augmented fluoroscopy: a new and novel navigation platform for peripheral bronchoscopy. J Bronchology Interv Pulmonol 28:116–123
Wolf FJ, Grand DJ, Machan JT, Dipetrillo TA, Mayo-Smith WW, Dupuy DE (2008) Microwave ablation of lung malignancies: effectiveness, CT findings, and safety in 50 patients. Radiology 247:871–879
Ni Y, Peng J, Yang X et al (2021) Multicentre study of microwave ablation for pulmonary oligorecurrence after radical resection of non-small-cell lung cancer. Br J Cancer 125:672–678
Aufranc V, Farouil G, Abdel-Rehim M et al (2019) Percutaneous thermal ablation of primary and secondary lung tumors: comparison between microwave and radiofrequency ablation. Diagn Interv Imaging 100:781–791
Emara EHA, Aboelezz MSMO, Rahman HEDMA, Biomy SS, Vogl TJ (2020) Role of microwave ablation in treatment of lung tumors. Med J Cairo Univ 88:1117–1129
Li L, Wu K, Lai H, Zhang B (2017) Clinical application of CT-guided percutaneous microwave ablation for the treatment of lung metastasis from colorectal cancer. Gastroenterol Res Pract 2017:9621585
Palussiere J, Catena V, Gaubert JY, Buy X, de Baere T (2017) Percutaneous lung thermo-ablation. Bull Cancer 104:417–422
Chang HC, Yang MC (2018) Systemic air embolism after percutaneous computed tomography-guided lung biopsy due to a kink in the coaxial biopsy system: a case report. BMC Med Imaging 18:1
Fiore L, Frenk NE, Martins GLP, Viana PCC, de Menezes MR (2017) Systemic air embolism after percutaneous lung biopsy: a manageable complication. J Radiol Case Rep 11:6–14
Ramaswamy R, Narsinh KH, Tuan A, Kinney TB (2014) Systemic air embolism following percutaneous lung biopsy. Semin Intervent Radiol 31:375–377
Kramer M, Parekh M, Modi RY, Donuru A (2020) Review of thoracic causes of systemic arterial air embolism on computed tomography. J Thorac Imaging 35:W68–W74
Franke M, Reinhardt HC, von Bergwelt-Baildon M, Bangard C (2014) Massive air embolism after lung biopsy. Circulation 129:1046–1047
Magnusson L, Spahn DR (2003) New concepts of atelectasis during general anaesthesia. Br J Anaesth 91:61–72
Hedenstierna G, Rothen HU (2000) Atelectasis formation during anesthesia: causes and measures to prevent it. J Clin Monit Comput 16:329–335
Hu B, Ren W, Feng Z et al (2022) Correlation between CT imaging characteristics and pathological diagnosis for subcentimeter pulmonary nodules. Thorac Cancer 13:1067–1075
de Morais AQ, da Silva TPF, Braga JCD et al (2020) Factors associated with subcentimeter pulmonary nodule outcomes followed with computed tomography imaging in oncology patients. Eur J Radiol Open 7:100266
Takenaka T (2017) How to manage patients with subcentimeter non-small cell lung cancer? J Thorac Dis 9:4860–4862
Sanchez M, Benegas M, Vollmer I (2018) Management of incidental lung nodules <8 mm in diameter. J Thorac Dis 10:S2611–S2627
Ahmed M, Solbiati L, Brace CL et al (2014) Image-guided tumor ablation: standardization of terminology and reporting criteria–a 10-year update. Radiology 273:241–260
Pillai K, Akhter J, Chua TC et al (2015) Heat sink effect on tumor ablation characteristics as observed in monopolar radiofrequency, bipolar radiofrequency, and microwave, using ex vivo calf liver model. Medicine (Baltimore) 94:e580
Brace CL (2009) Radiofrequency and microwave ablation of the liver, lung, kidney, and bone: what are the differences? Curr Probl Diagn Radiol 38:135–143
Brace CL (2010) Microwave tissue ablation: biophysics, technology, and applications. Crit Rev Biomed Eng 38:65–78
Radosevic A, Quesada R, Serlavos C et al (2022) Microwave versus radiofrequency ablation for the treatment of liver malignancies: a randomized controlled phase 2 trial. Sci Rep 12:316
Primavesi F, Swierczynski S, Klieser E et al (2018) Thermographic real-time-monitoring of surgical radiofrequency and microwave ablation in a perfused porcine liver model. Oncol Lett 15:2913–2920
Dodd GD 3rd, Dodd NA, Lanctot AC, Glueck DA (2013) Effect of variation of portal venous blood flow on radiofrequency and microwave ablations in a blood-perfused bovine liver model. Radiology 267:129–136
Abbas G, Pennathur A, Landreneau RJ, Luketich JD (2009) Radiofrequency and microwave ablation of lung tumors. J Surg Oncol 100:645–650
Fan W, Li X, Zhang L, Jiang H, Zhang J (2012) Comparison of microwave ablation and multipolar radiofrequency ablation in vivo using two internally cooled probes. AJR Am J Roentgenol 198:W46–W50
Andreano A, Huang Y, Meloni MF, Lee FT Jr, Brace C (2010) Microwaves create larger ablations than radiofrequency when controlled for power in ex vivo tissue. Med Phys 37:2967–2973
Crocetti L, Bozzi E, Faviana P et al (2010) Thermal ablation of lung tissue: in vivo experimental comparison of microwave and radiofrequency. Cardiovasc Intervent Radiol 33:818–827
Li HW, Long YJ, Yan GW et al (2022) Microwave ablation vs. cryoablation for treatment of primary and metastatic pulmonary malignant tumors. Mol Clin Oncol 16:62
Bourgouin PP, Wrobel MM, Mercaldo ND et al (2022) Comparison of percutaneous image-guided microwave ablation and cryoablation for sarcoma lung metastases: a 10-year experience. AJR Am J Roentgenol 218:494–504
Pistorius GA, Alexander C, Krisch CM, Feifel G, Schilling MK, Menger MD (2005) Local platelet trapping as the cause of thrombocytopenia after hepatic cryotherapy. World J Surg 29:657–660 (discussion 661)
Acknowledgements
The authors thank the Siemens Healthcare marketing manager, Frank Chun-Hsien Wu, PhD, and the application specialist, Maxwell Jiun-Yan Lin, for their technical assistance with the ARTIS Pheno operation and image post processing. They also thank the Siemens Healthcare research scientist Shwetambara Malwade for her helpful advice regarding revision of the manuscript.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Shun-Mao Yang.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have not been previously reported.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chang, LK., Yang, SM., Chung, WY. et al. Cone-beam computed tomography image-guided percutaneous microwave ablation for lung nodules in a hybrid operating room: an initial experience. Eur Radiol (2023). https://doi.org/10.1007/s00330-023-10360-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00330-023-10360-5