Abstract
Objectives
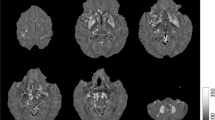
Iron deposition and mitochondrial dysfunction are closely associated with the genesis and progression of Parkinson’s disease (PD). This study aims to extract susceptibility and oxygen extraction fraction (OEF) values of deep grey matter (DGM) to explore spatiotemporal progression patterns of brain iron-oxygen metabolism in PD.
Methods
Ninety-five PD patients and forty healthy controls (HCs) were included. Quantitative susceptibility mapping (QSM) and OEF maps were computed from MRI multi-echo gradient echo data. Analysis of covariance (ANCOVA) was used to compare mean susceptibility and OEF values in DGM between early-stage PD (ESP), advanced-stage PD (ASP) patients and HCs. Then Granger causality analysis on the pseudo-time-series of MRI data was applied to assess the causal effect of early altered nuclei on iron content and oxygen extraction in other DGM nuclei.
Results
The susceptibility values in substantia nigra (SN), red nucleus, and globus pallidus (GP) significantly increased in PD patients compared with HCs, while the iron content in GP did not elevate obviously until the late stage. The mean OEF values for the caudate nucleus, putamen, and dentate nucleus were higher in ESP patients than in ASP patients or/and HCs. We also found that iron accumulation progressively expands from the midbrain to the striatum. These alterations were correlated with clinical features and improved AUC for early PD diagnosis to 0.824.
Conclusions
Abnormal cerebral iron deposition and tissue oxygen utilization in PD measured by QSM and OEF maps could reflect pathological alterations in neurodegenerative processes and provide valuable indicators for disease identification and management.
Clinical relevance statement
Noninvasive assessment of cerebral iron-oxygen metabolism may serve as clinical evidence of pathological changes in PD and improve the validity of diagnosis and disease monitoring.
Key Points
• Quantitative susceptibility mapping and oxygen extraction fraction maps indicated the cerebral pathology of abnormal iron accumulation and oxygen metabolism in Parkinson’s disease.
• Iron deposition is mainly in the midbrain, while altered oxygen metabolism is concentrated in the striatum and cerebellum.
• The susceptibility and oxygen extraction fraction values in subcortical nuclei were associated with clinical severity.






Similar content being viewed by others
Abbreviations
- ASP:
-
Advanced-stage Parkinson’s disease
- CaSCNs:
-
Causal structural covariance network
- CAU:
-
Caudate nucleus
- CMRO2:
-
Cerebral oxygen consumption
- DGM:
-
Deep grey matter
- DN:
-
Dentate nucleus
- ESP:
-
Early-stage Parkinson’s disease
- FDG-PET:
-
Fluorodeoxyglucose positron emission tomography
- GCA:
-
Granger causality analysis
- GP:
-
Globus pallidus
- HCs:
-
Healthy controls
- H-Y stage:
-
Hoehn & Yahr stage
- LEDD:
-
Levodopa equivalent daily dose
- mGRE:
-
Multi-echo gradient echo
- MMSE:
-
Mini-Mental State Examination
- OEF:
-
Oxygen extraction fraction
- PD:
-
Parkinson’s disease
- PUT:
-
Putamen
- QSM:
-
Quantitative susceptibility mapping
- RN:
-
Red nucleus
- ROI:
-
Region of interest
- SN:
-
Substantia nigra
- UPDRS-III:
-
The third part of the Unified Parkinson’s Disease Rating Scale
References
Maiti P, Manna J, Dunbar GL (2017) Current understanding of the molecular mechanisms in Parkinson’s disease: targets for potential treatments. Transl Neurodegener 6:28
Dauer W, Przedborski S (2003) Parkinson’s disease: mechanisms and models. Neuron 39:889–909
Albrecht F, Ballarini T, Neumann J, Schroeter ML (2019) FDG-PET hypometabolism is more sensitive than MRI atrophy in Parkinson’s disease: a whole-brain multimodal imaging meta-analysis. Neuroimage Clin 21:101594
Meles SK, Renken RJ, Pagani M et al (2020) Abnormal pattern of brain glucose metabolism in Parkinson’s disease: replication in three European cohorts. Eur J Nucl Med Mol Imag 47:437–450
Wang JY, Zhuang QQ, Zhu LB et al (2016) Meta-analysis of brain iron levels of Parkinson’s disease patients determined by postmortem and MRI measurements. Sci Rep 6:36669
Guan X, Xu X, Zhang M (2017) Region-specific iron measured by MRI as a biomarker for Parkinson’s disease. Neurosci Bull 33:561–567
Haacke EM, Cheng NY, House MJ et al (2005) Imaging iron stores in the brain using magnetic resonance imaging. Magn Reson Imaging 23:1–25
Sofic E, Paulus W, Jellinger K, Riederer P, Youdim MB (1991) Selective increase of iron in substantia nigra zona compacta of parkinsonian brains. J Neurochem 56:978–982
Götz ME, Double K, Gerlach M, Youdim MB, Riederer P (2004) The relevance of iron in the pathogenesis of Parkinson’s disease. Ann N Y Acad Sci 1012:193–208
Ward RJ, Zucca FA, Duyn JH, Crichton RR, Zecca L (2014) The role of iron in brain ageing and neurodegenerative disorders. Lancet Neurol 13:1045–1060
Langkammer C, Schweser F, Krebs N et al (2012) Quantitative susceptibility mapping (QSM) as a means to measure brain iron? A post mortem validation study. Neuroimage 62:1593–1599
Wu B, Li W, Guidon A, Liu C (2012) Whole brain susceptibility mapping using compressed sensing. Magn Reson Med 67:137–147
Acosta-Cabronero J, Cardenas-Blanco A, Betts MJ et al (2017) The whole-brain pattern of magnetic susceptibility perturbations in Parkinson’s disease. Brain 140:118–131
He N, Ling H, Ding B et al (2015) Region-specific disturbed iron distribution in early idiopathic Parkinson’s disease measured by quantitative susceptibility mapping. Hum Brain Mapp 36:4407–4420
Guan X, Xuan M, Gu Q et al (2017) Regionally progressive accumulation of iron in Parkinson’s disease as measured by quantitative susceptibility mapping. NMR Biomed 30:4
Wu P, Wang J, Peng S et al (2013) Metabolic brain network in the Chinese patients with Parkinson’s disease based on 18F-FDG PET imaging. Parkinsonism Relat Disord 19:622–627
Borghammer P, Cumming P, Østergaard K et al (2012) Cerebral oxygen metabolism in patients with early Parkinson’s disease. J Neurol Sci 313:123–128
Cho J, Zhang S, Kee Y et al (2020) Cluster analysis of time evolution (CAT) for quantitative susceptibility mapping (QSM) and quantitative blood oxygen level-dependent magnitude (qBOLD)-based oxygen extraction fraction (OEF) and cerebral metabolic rate of oxygen (CMRO2) mapping. Magn Reson Med 83:844–857
Cho J, Lee J, An H, Goyal MS, Su Y, Wang Y (2021) Cerebral oxygen extraction fraction (OEF): comparison of challenge-free gradient echo QSM+qBOLD (QQ) with (15)O PET in healthy adults. J Cereb Blood Flow Metab 41:1658–1668
Postuma RB, Berg D, Stern M et al (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30:1591–1601
Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25:2649–2653
Liu Z, Spincemaille P, Yao Y, Zhang Y, Wang Y (2018) MEDI+0: Morphology enabled dipole inversion with automatic uniform cerebrospinal fluid zero reference for quantitative susceptibility mapping. Magn Reson Med 79:2795–2803
Liu T, Wisnieff C, Lou M, Chen W, Spincemaille P, Wang Y (2013) Nonlinear formulation of the magnetic field to source relationship for robust quantitative susceptibility mapping. Magn Reson Med 69:467–476
Liu T, Khalidov I, de Rochefort L et al (2011) A novel background field removal method for MRI using projection onto dipole fields (PDF). NMR Biomed 24:1129–1136
Cho J, Kee Y, Spincemaille P et al (2018) Cerebral metabolic rate of oxygen (CMRO2) mapping by combining quantitative susceptibility mapping (QSM) and quantitative blood oxygenation level-dependent imaging (qBOLD). Magn Reson Med 80:1595–1604
Cho J, Spincemaille P, Nguyen TD, Gupta A, Wang Y (2021) Temporal clustering, tissue composition, and total variation for mapping oxygen extraction fraction using QSM and quantitative BOLD. Magn Reson Med 86:2635–2646
Zhang Y, Wei H, Cronin MJ, He N, Yan F, Liu C (2018) Longitudinal atlas for normative human brain development and aging over the lifespan using quantitative susceptibility mapping. Neuroimage 171:176–189
Zhang Z, Liao W, Xu Q et al (2017) Hippocampus-associated causal network of structural covariance measuring structural damage progression in temporal lobe epilepsy. Hum Brain Mapp 38:753–766
Berding G, Odin P, Brooks DJ et al (2001) Resting regional cerebral glucose metabolism in advanced Parkinson’s disease studied in the off and on conditions with [(18)F]FDG-PET. Mov Disord 16:1014–1022
Kordower JH, Olanow CW, Dodiya HB et al (2013) Disease duration and the integrity of the nigrostriatal system in Parkinson’s disease. Brain 136:2419–2431
Herman S, Djaldetti R, Mollenhauer B, Offen D (2022) CSF-derived extracellular vesicles from patients with Parkinson’s disease induce symptoms and pathology. Brain 146:209–224
Zhang Y, Larcher KM, Misic B, Dagher A (2017) Anatomical and functional organization of the human substantia nigra and its connections. eLife 6:e26653
Lin TP, Carbon M, Tang C et al (2008) Metabolic correlates of subthalamic nucleus activity in Parkinson’s disease. Brain 131(Pt 5):1373–1380
Tang BL (2020) Glucose, glycolysis, and neurodegenerative diseases. J Cell Physiol 235:7653–7662
Ko JH, Lerner RP, Eidelberg D (2015) Effects of levodopa on regional cerebral metabolism and blood flow. Mov Disord 30:54–63
Zang Z, Song T, Li J et al (2022) Modulation effect of substantia nigra iron deposition and functional connectivity on putamen glucose metabolism in Parkinson’s disease. Hum Brain Mapp 43:3735–3744
Cheng HC, Ulane CM, Burke RE (2010) Clinical progression in Parkinson disease and the neurobiology of axons. Ann Neurol 67:715–725
Lewis MM, Du G, Kidacki M et al (2013) Higher iron in the red nucleus marks Parkinson’s dyskinesia. Neurobiol Aging 34:1497–1503
He N, Huang P, Ling H et al (2017) Dentate nucleus iron deposition is a potential biomarker for tremor-dominant Parkinson’s disease. NMR Biomed 30:4
Peralta M, Baxter JSH, Khan AR, Haegelen C, Jannin P (2020) Striatal shape alteration as a staging biomarker for Parkinson’s disease. Neuroimage Clin 27:102272
Hou Y, Zhang L, Ou R et al (2022) Motor progression marker for newly diagnosed drug-naïve patients with Parkinson’s disease: a resting-state functional MRI study. Hum Brain Mapp 44:901–913
Kosyakovsky J, Fine JM, Frey WH, 2nd, Hanson LR (2021) Mechanisms of intranasal deferoxamine in neurodegenerative and neurovascular disease. Pharmaceuticals (Basel) 14:95
Novak P, Pimentel Maldonado DA, Novak V (2019) Safety and preliminary efficacy of intranasal insulin for cognitive impairment in Parkinson disease and multiple system atrophy: a double-blinded placebo-controlled pilot study. PLoS One 14:e0214364
Acknowledgements
The authors thank all the PD patients and healthy control subjects who participated in this study.
Funding
This study was supported by the Regional Innovation and Development Joint Fund of the National Natural Science Foundation of China (U22A20354).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Professor Wenzhen Zhu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• cross-sectional study
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yan, S., Lu, J., Li, Y. et al. Spatiotemporal patterns of brain iron-oxygen metabolism in patients with Parkinson’s disease. Eur Radiol 34, 3074–3083 (2024). https://doi.org/10.1007/s00330-023-10283-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10283-1