Abstract
Objective
This study aimed to evaluate the diagnostic performance of machine learning (ML)–based ultrasound (US) radiomics models for risk stratification of gallbladder (GB) masses.
Methods
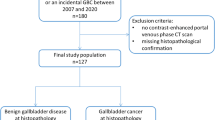
We prospectively examined 640 pathologically confirmed GB masses obtained from 640 patients between August 2019 and October 2022 at four institutions. Radiomics features were extracted from grayscale US images and germane features were selected. Subsequently, 11 ML algorithms were separately used with the selected features to construct optimum US radiomics models for risk stratification of the GB masses. Furthermore, we compared the diagnostic performance of these models with the conventional US and contrast-enhanced US (CEUS) models.
Results
The optimal XGBoost-based US radiomics model for discriminating neoplastic from non-neoplastic GB lesions showed higher diagnostic performance in terms of areas under the curves (AUCs) than the conventional US model (0.822–0.853 vs. 0.642–0.706, p < 0.05) and potentially decreased unnecessary cholecystectomy rate in a speculative comparison with performing cholecystectomy for lesions sized over 10 mm (2.7–13.8% vs. 53.6–64.9%, p < 0.05) in the validation and test sets. The AUCs of the XGBoost-based US radiomics model for discriminating carcinomas from benign GB lesions were higher than the conventional US model (0.904–0.979 vs. 0.706–0.766, p < 0.05). The XGBoost-US radiomics model performed better than the CEUS model in discriminating GB carcinomas (AUC: 0.995 vs. 0.902, p = 0.011).
Conclusions
The proposed ML-based US radiomics models possess the potential capacity for risk stratification of GB masses and may reduce the unnecessary cholecystectomy rate and use of CEUS.
Clinical relevance statement
The machine learning-based ultrasound radiomics models have potential for risk stratification of gallbladder masses and may potentially reduce unnecessary cholecystectomies.
Key Points
• The XGBoost-based US radiomics models are useful for the risk stratification of GB masses.
• The XGBoost-based US radiomics model is superior to the conventional US model for discriminating neoplastic from non-neoplastic GB lesions and may potentially decrease unnecessary cholecystectomy rate for lesions sized over 10 mm in comparison with the current consensus guideline.
• The XGBoost-based US radiomics model could overmatch CEUS model in discriminating GB carcinomas from benign GB lesions.





Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- CEA:
-
Carcinoembryonic antigen
- CEUS:
-
Contrast-enhanced ultrasound
- GB:
-
Gallbladder
- ICC:
-
Intraclass correlation coefficient
- ML:
-
Machine learning
- ROI:
-
Region of interest
- US:
-
Ultrasound
- XGBoost:
-
Extreme gradient boosting
References
McCain RS, Diamond A, Jones C, Coleman HG (2018) Current practices and future prospects for the management of gallbladder polyps: a topical review. World J Gastroenterol 24:2844–2852
Ganeshan D, Kambadakone A, Nikolaidis P et al (2021) Current update on gallbladder carcinoma. Abdom Radiol (NY) 46:2474–2489
Mellnick VM, Menias CO, Sandrasegaran K et al (2015) Polypoid lesions of the gallbladder: disease spectrum with pathologic correlation. Radiographics 35:387–399
Ramachandran A, Srivastava DN, Madhusudhan KS (2021) Gallbladder cancer revisited: the evolving role of a radiologist. Br J Radiol 94:20200726
Randi G, Franceschi S, La Vecchia C (2006) Gallbladder cancer worldwide: geographical distribution and risk factors. Int J Cancer 118:1591–1602
Jang JY, Kim SW, Lee SE et al (2009) Differential diagnostic and staging accuracies of high resolution ultrasonography, endoscopic ultrasonography, and multidetector computed tomography for gallbladder polypoid lesions and gallbladder cancer. Ann Surg 250:943–949
Kai K, Aishima S, Miyazaki K (2014) Gallbladder cancer: clinical and pathological approach. World J Clin Cases 2:515–521
Babu BI, Dennison AR, Garcea G (2015) Management and diagnosis of gallbladder polyps: a systematic review. Langenbecks Arch Surg 400:455–462
Bhatt NR, Gillis A, Smoothey CO, Awan FN, Ridgway PF (2016) Evidence based management of polyps of the gall bladder: a systematic review of the risk factors of malignancy. Surgeon 14:278–286
Park HY, Oh SH, Lee KH, Lee JK, Lee KT (2015) Is cholecystectomy a reasonable treatment option for simple gallbladder polyps larger than 10 mm? World J Gastroenterol 21:4248–4254
Coburn NG, Cleary SP, Tan JC, Law CH (2008) Surgery for gallbladder cancer: a population-based analysis. J Am Coll Surg 207:371–382
Yu MH, Kim YJ, Park HS, Jung SI (2020) Benign gallbladder diseases: imaging techniques and tips for differentiating with malignant gallbladder diseases. World J Gastroenterol 26:2967–2986
Elmasry M, Lindop D, Dunne DF et al (2016) The risk of malignancy in ultrasound detected gallbladder polyps: a systematic review. Int J Surg 33:28–35
Kim JH, Lee JY, Baek JH et al (2015) High-resolution sonography for distinguishing neoplastic gallbladder polyps and staging gallbladder cancer. AJR Am J Roentgenol 204:W150-159
Kim JS, Lee JK, Kim Y, Lee SM (2016) US characteristics for the prediction of neoplasm in gallbladder polyps 10 mm or larger. Eur Radiol 26:1134–1140
Lee JS, Kim JH, Kim YJ et al (2017) Diagnostic accuracy of transabdominal high-resolution US for staging gallbladder cancer and differential diagnosis of neoplastic polyps compared with EUS. Eur Radiol 27:3097–3103
Choi TW, Kim JH, Park SJ et al (2018) Risk stratification of gallbladder polyps larger than 10 mm using high-resolution ultrasonography and texture analysis. Eur Radiol 28:196–205
Cheng Y, Wang M, Ma B, Ma X (2018) Potential role of contrast-enhanced ultrasound for the differentiation of malignant and benign gallbladder lesions in east Asia: a meta-analysis and systematic review. Medicine (Baltimore) 97:e11808
Negrão de Figueiredo G, Mueller-Peltzer K, Armbruster M, Rübenthaler J, Clevert DA (2019) Contrast-enhanced ultrasound (CEUS) for the evaluation of gallbladder diseases in comparison to cross-sectional imaging modalities and histopathological results. Clin Hemorheol Microcirc 71:141–149
Liang X, Jing X (2020) Meta-analysis of contrast-enhanced ultrasound and contrast-enhanced harmonic endoscopic ultrasound for the diagnosis of gallbladder malignancy. BMC Med Inform Decis Mak 20:235
Xie XH, Xu HX, Xie XY et al (2010) Differential diagnosis between benign and malignant gallbladder diseases with real-time contrast-enhanced ultrasound. Eur Radiol 20:239–248
Liu LN, Xu HX, Lu MD et al (2012) Contrast-enhanced ultrasound in the diagnosis of gallbladder diseases: a multi-center experience. PLoS One 7:e48371
Yuan Z, Liu X, Li Q et al (2021) Is contrast-enhanced ultrasound superior to computed tomography for differential diagnosis of gallbladder polyps? a cross-sectional study. Front Oncol 11:657223
Liu Z, Zhang XY, Shi YJ et al (2017) Radiomics analysis for evaluation of pathological complete response to neoadjuvant chemoradiotherapy in locally advanced rectal cancer. Clin Cancer Res 23:7253–7262
Huang YQ, Liang CH, He L (2016) Development and validation of a radiomics nomogram for preoperative prediction of lymph node metastasis in colorectal cancer. J Clin Oncol 34:2157–2164
Lambin P, Leijenaar RTH, Deist TM et al (2017) Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol 14:749–762
Lambin P, Rios-Velazquez E, Leijenaar R et al (2012) Radiomics: extracting more information from medical images using advanced feature analysis. Eur J Cancer 48:441–446
Gillies RJ, Kinahan PE, Hricak H (2016) Radiomics: images are more than pictures, they are data. Radiology 278:563–577
Jeong Y, Kim JH, Chae HD et al (2020) Deep learning-based decision support system for the diagnosis of neoplastic gallbladder polyps on ultrasonography: preliminary results. Sci Rep 10:7700
Yuan HX, Yu QH, Zhang YQ et al (2020) Ultrasound radiomics effective for preoperative identification of true and pseudo gallbladder polyps based on spatial and morphological features. Front Oncol 10:1719
Zhao CK, Ren TT, Yin YF et al (2021) A comparative analysis of two machine learning-based diagnostic patterns with thyroid imaging reporting and data system for thyroid nodules: diagnostic performance and unnecessary biopsy rate. Thyroid 31:470–481
Yushkevich PA, Piven J, Hazlett HC et al (2006) User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage 31:1116–1128
Varma S, Simon R (2006) Bias in error estimation when using cross-validation for model selection. BMC Bioinformatics 7:91
Foley KG, Lahaye MJ, Thoeni RF (2022) Management and follow-up of gallbladder polyps: updated joint guidelines between the ESGAR, EAES, EFISDS and ESGE. Eur Radiol 32:3358–3368
Wiles R, Thoeni R, Barbu S et al (2017) Management and follow-up of gallbladder polyps: joint guidelines between the European Society of Gastrointestinal and Abdominal Radiology (ESGAR), European Association for Endoscopic Surgery and other Inter-ventional Techniques (EAES), International Society of Digestive Surgery - European Federation (EFISDS) and European Society of Gastrointestinal Endoscopy (ESGE). Eur Radiol 27:3856–3866
Isherwood J, Oakland K, Khanna A (2019) A systematic review of the ae- tiology and management of post cholecystectomy syndrome. Surgeon 17:33–42
Womack NA, Crider RL (1947) The persistence of symptoms following cholecystectomy. Ann Surg 126:31–55
Tarnasky PR (2016) Post-cholecystectomy syndrome and sphincter of Oddi dysfunction: past, present and future. Expert Rev Gastroenterol Hepatol 10:1359–1372
Misra S, Chaturvedi A, Misra NC, Sharma ID (2003) Carcinoma of the gallbladder. Lancet Oncol 4:167–176
Tian YH, Ji X, Liu B et al (2015) Surgical treatment of incidental gallbladder cancer discovered during or following laparoscopic cholecystectomy. World J Surg 39:746–752
Zhou W, Yang Y, Yu C et al (2021) Ensembled deep learning model outperforms human experts in diagnosing biliary atresia from sonographic gallbladder images. Nat Commun 12:1259
Ji GW, Zhang YD, Zhang H et al (2019) Biliary tract cancer at CT: a radiomics-based model to predict lymph node metastasis and survival outcomes. Radiology 290:90–98
Xiang F, Liang X, Yang L, Liu X, Yan S (2022) Contrast-enhanced CT radiomics for prediction of recurrence-free survival in gallbladder carcinoma after surgical resection. Eur Radiol 32:7087–7097
Chen T, Guestrin C (2016) XGBoost: a scalable tree boosting system. In: Proceedings of the 22nd ACM SIGKDD international conference on knowledge discovery and data mining-KDD 2016, San Francisco, CA, USA, pp 785–794
Cha BH, Hwang JH, Lee SH et al (2011) Pre-operative factors that can predict neoplastic polypoid lesions of the gallbladder. World J Gastroenterol 17:2216–2222
French DG, Allen PD, Ellsmere JC (2013) The diagnostic accuracy of transabdominal ultrasonography needs to be considered when managing gallbladder polyps. Surg Endosc 27:4021–4025
Zhang HP, Bai M, Gu JY, He YQ, Qiao XH, Du LF (2018) Value of contrast-enhanced ultrasound in the differential diagnosis of gallbladder lesion. World J Gastroenterol 24:744–751
Chen LD, Huang Y, Xie XH et al (2017) Diagnostic nomogram for gallbladder wall thickening mimicking malignancy: using contrast-enhanced ultrasonography or multi-detector computed tomography? Abdom Radiol (NY) 42:2436–2446
Sun LP, Guo LH, Xu HX et al (2015) Value of contrast-enhanced ultrasound in the differential diagnosis between gallbladder adenoma and gallbladder adenoma canceration. Int J Clin Exp Med 8:1115–1121
Ganeshan D, Kambadakone A, Nikolaidis P, Subbiah V, Subbiah IM, Devine C (2021) Current update on gallbladder carcinoma. Abdom Radiol (NY) 46:2474–2489
Wang YF, Feng FL, Zhao XH et al (2014) Combined detection tumor markers for diagnosis and prognosis of gallbladder cancer. World J Gastroenterol 20:4085–4092
Shukla VK, Gurubachan, Sharma D, Dixit VK, Usha (2006) Diagnostic value of serum CA242, CA 19-9, CA 15-3 and CA 125 in patients with carcinoma of the gallbladder. Trop Gastroenterol 27:160-165
Funding
This work was supported in part by the National Natural Science Foundation of China (Grant 82202174), the Science and Technology Commission of Shanghai Municipality (Grants 18441905500, and 19DZ2251100), Shanghai Municipal Health Commission (Grants 2019LJ21 and SHSLCZDZK03502), Shanghai Science and Technology Innovation Action Plan (21Y11911200), and Fundamental Research Funds for the Central Universities (ZD-11-202151), Scientific Research and Development Fund of Zhongshan Hospital of Fudan University (Grant 2022ZSQD07).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Hui-Xiong Xu.
Conflict of interest
These authors declare that they have no conflict of interest.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from patients in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• diagnostic or prognostic study
• performed at four institutions
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, LF., Wang, Q., Mao, F. et al. Risk stratification of gallbladder masses by machine learning-based ultrasound radiomics models: a prospective and multi-institutional study. Eur Radiol 33, 8899–8911 (2023). https://doi.org/10.1007/s00330-023-09891-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09891-8