Abstract
Objectives
To develop and validate a radiomics nomogram based on a fully automated pancreas segmentation to assess pancreatic exocrine function. Furthermore, we aimed to compare the performance of the radiomics nomogram with the pancreatic flow output rate (PFR) and conclude on the replacement of secretin-enhanced magnetic resonance cholangiopancreatography (S-MRCP) by the radiomics nomogram for pancreatic exocrine function assessment.
Methods
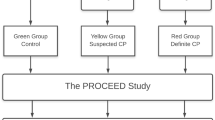
All participants underwent S-MRCP between April 2011 and December 2014 in this retrospective study. PFR was quantified using S-MRCP. Participants were divided into normal and pancreatic exocrine insufficiency (PEI) groups using the cut-off of 200 µg/L of fecal elastase-1. Two prediction models were developed including the clinical and non-enhanced T1-weighted imaging radiomics model. A multivariate logistic regression analysis was conducted to develop the prediction models. The models’ performances were determined based on their discrimination, calibration, and clinical utility.
Results
A total of 159 participants (mean age \(\pm\) standard deviation, 45 years \(\pm\) 14;119 men) included 85 normal and 74 PEI. All the participants were divided into a training set comprising 119 consecutive patients and an independent validation set comprising 40 consecutive patients. The radiomics score was an independent risk factor for PEI (odds ratio = 11.69; p < 0.001). In the validation set, the radiomics nomogram exhibited the highest performance (AUC, 0.92) in PEI prediction, whereas the clinical nomogram and PFR had AUCs of 0.79 and 0.78, respectively.
Conclusion
The radiomics nomogram accurately predicted pancreatic exocrine function and outperformed pancreatic flow output rate on S-MRCP in patients with chronic pancreatitis.
Key Points
• The clinical nomogram exhibited moderate performance in diagnosing pancreatic exocrine insufficiency.
• The radiomics score was an independent risk factor for pancreatic exocrine insufficiency, and every point rise in the rad-score was associated with an 11.69-fold increase in pancreatic exocrine insufficiency risk.
• The radiomics nomogram accurately predicted pancreatic exocrine function and outperformed the clinical model and pancreatic flow output rate quantified by secretin-enhanced magnetic resonance cholangiopancreatography on MRI in patients with chronic pancreatitis.






Similar content being viewed by others
Abbreviations
- CP:
-
Chronic pancreatitis
- PEI:
-
Pancreatic exocrine insufficiency
- PFT:
-
Pancreatic exocrine function test
- FE-1:
-
Fecal elastase-1
- ELISA:
-
Enzyme-linked immunosorbent assay
- S-MRCP:
-
Secretin-enhanced magnetic resonance cholangiopancreatography
- PFR:
-
Pancreatic flow output rate
- MPD:
-
Main pancreatic duct
- BPD:
-
Branch pancreatic duct
- SIR:
-
Signal intensity ratio
- Rad-score:
-
Radiomics score
References
Hart PA, Conwell DL (2020) Chronic pancreatitis: managing a difficult disease. Am J Gastroenterol 115:49–55
Trout AT, Wallihan DB, Serai S, Abu-El-Haija M (2017) Secretin-enhanced magnetic resonance cholangiopancreatography for assessing pancreatic secretory function in children. J Pediatr 188:186–191
Schiller LR, Rivera LM, Santangelo WC, Little KH, Fordtran JS (1994) Diagnostic value of fasting plasma peptide concentrations in patients with chronic diarrhea. Dig Dis Sci 39:2216–2222
Manfredi R, Pozzi Mucelli R (2016) Secretin-enhanced MR imaging of the pancreas. Radiology 279:29–43
Lindkvist B (2013) Diagnosis and treatment of pancreatic exocrine insufficiency. World J Gastroenterol 19:7258–7266
Lankisch PG (1982) Exocrine pancreatic function tests. Gut 23:777–798
Law R, Lopez R, Costanzo A, Parsi MA, Stevens T (2012) Endoscopic pancreatic function test using combined secretin and cholecystokinin stimulation for the evaluation of chronic pancreatitis. Gastrointest Endosc 75:764–768
Vanga RR, Tansel A, Sidiq S, El-Serag HB, Othman MO (2018) Diagnostic performance of measurement of fecal elastase-1 in detection of exocrine pancreatic insufficiency: systematic review and meta-analysis. Clin Gastroenterol Hepatol 16(1220–1228):e1224
Mensel B, Messner P, Mayerle J et al (2014) Secretin-stimulated MRCP in volunteers: assessment of safety, duct visualization, and pancreatic exocrine function. AJR Am J Roentgenol 202:102–108
Punwani S, Gillams AR, Lees WR (2003) Non-invasive quantification of pancreatic exocrine function using secretin-stimulated MRCP. Eur Radiol 13:273–276
Manfredi R, Ventriglia A, Mantovani W et al (2015) Mucinous cystic neoplasms and serous cystadenomas arising in the body-tail of the pancreas: MR imaging characterization. Eur Radiol 25:940–949
Bian Y, Wang L, Chen C et al (2013) Quantification of pancreatic exocrine function of chronic pancreatitis with secretin-enhanced MRCP. World J Gastroenterol 19:7177–7182
Wathle GK, Tjora E, Ersland L et al (2014) Assessment of exocrine pancreatic function by secretin-stimulated magnetic resonance cholangiopancreaticography and diffusion-weighted imaging in healthy controls. J Magn Reson Imaging 39:448–454
Bali MA, Sontou R, Arvanitakis M, Metens T, Deviere J, Matos C (2007) Evaluation of the stimulating effect of a low dose of secretin compared to the standard dose on the exocrine pancreas with MRCP: preliminary results in normal subjects (MRCP quantification of secretin stimulation). Abdom Imaging 32:743–748
de la Pinta C (2022) Radiomics in pancreatic cancer for oncologist: present and future. Hepatobiliary Pancreat Dis Int 21:356–361
Preuss K, Thach N, Liang X et al (2022) Using quantitative imaging for personalized medicine in pancreatic cancer: a review of radiomics and deep learning applications. Cancers (Basel) 14:1654
Virarkar M, Wong VK, Morani AC, Tamm EP, Bhosale P (2022) Update on quantitative radiomics of pancreatic tumors. Abdom Radiol (NY) 47:3118–3160
Moons KG, Altman DG, Reitsma JB et al (2015) Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med 162:W1-73
Ito T, Ishiguro H, Ohara H et al (2016) Evidence-based clinical practice guidelines for chronic pancreatitis 2015. J Gastroenterol 51:85–92
Zhang Q, Sun B, Cheng Y, Li X (2021) Residual self-calibration and self-attention aggregation network for crop disease recognition. Int J Environ Res Public Health 18:8404
Portet S (2020) A primer on model selection using the Akaike information criterion. Infect Dis Model 5:111–128
Gillams A, Pereira S, Webster G, Lees W (2008) Correlation of MRCP quantification (MRCPQ) with conventional non-invasive pancreatic exocrine function tests. Abdom Imaging 33:469–473
Gillams AR, Lees WR (2007) Quantitative secretin MRCP (MRCPQ): results in 215 patients with known or suspected pancreatic pathology. Eur Radiol 17:2984–2990
Sandrasegaran K, Lin Y, Asare-Sawiri M, Taiyini T, Tann M (2019) CT texture analysis of pancreatic cancer. Eur Radiol 29:1067–1073
Bian Y, Guo S, Jiang H et al (2019) Relationship between radiomics and risk of lymph node metastasis in pancreatic ductal adenocarcinoma. Pancreas 48:1195–1203
Park S, Chu LC, Hruban RH et al (2020) Differentiating autoimmune pancreatitis from pancreatic ductal adenocarcinoma with CT radiomics features. Diagn Interv Imaging 101:555–564
Ren S, Zhao R, Cui W et al (2020) Computed tomography-based radiomics signature for the preoperative differentiation of pancreatic adenosquamous carcinoma from pancreatic ductal adenocarcinoma. Front Oncol 10:1618
Liu KL, Wu T, Chen PT et al (2020) Deep learning to distinguish pancreatic cancer tissue from non-cancerous pancreatic tissue: a retrospective study with cross-racial external validation. Lancet Digit Health 2:e303–e313
Funding
This work was supported in part by the National Science Foundation for Scientists of China (81871352, 82171915, and 82171930, 82202126, 82271972), The Natural Science Foundation of Shanghai Science and Technology Innovation Action Plan (21ZR1478500, 21Y11910300), Clinical Research Plan of SHDC (SHDC2020CR4073, SHDC2022CRD028), and 234 Platform Discipline Consolidation Foundation Project (2019YPT001, 2020YPT001).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Yun Bian.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
A professor of Biostatistics (Prof.Cheng Wu, PhD) was consulted for specialist advice.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained by the Changhai Hospital.
Methodology
• Retrospective
• Diagnostic or prognostic study
• Performed at one center institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bian, Y., Zhou, J., Zhu, M. et al. Replacing secretin-enhanced MRCP with MRI radiomics model based on a fully automated pancreas segmentation for assessing pancreatic exocrine function in chronic pancreatitis. Eur Radiol 33, 3580–3591 (2023). https://doi.org/10.1007/s00330-023-09448-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09448-9