Abstract
Objective
This study aimed to develop and validate post- and preoperative models for predicting recurrence after curative-intent surgery using an FDG PET-CT metabolic parameter to improve the prognosis of patients with synchronous colorectal cancer liver metastasis (SCLM).
Methods
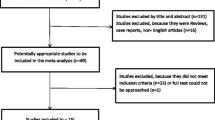
In this retrospective multicenter study, consecutive patients with resectable SCLM underwent upfront surgery between 2006 and 2015 (development cohort) and between 2006 and 2017 (validation cohort). In the development cohort, we developed and internally validated the post- and preoperative models using multivariable Cox regression with an FDG metabolic parameter (metastasis-to-primary-tumor uptake ratio [M/P ratio]) and clinicopathological variables as predictors. In the validation cohort, the models were externally validated for discrimination, calibration, and clinical usefulness. Model performance was compared with that of Fong’s clinical risk score (FCRS).
Results
A total of 374 patients (59.1 ± 10.5 years, 254 men) belonged in the development cohort and 151 (60.3 ± 12.0 years, 94 men) in the validation cohort. The M/P ratio and nine clinicopathological predictors were included in the models. Both postoperative and preoperative models showed significantly higher discrimination than FCRS (p < .05) in the external validation (time-dependent AUC = 0.76 [95% CI 0.68–0.84] and 0.76 [0.68–0.84] vs. 0.65 [0.57–0.74], respectively). Calibration plots and decision curve analysis demonstrated that both models were well calibrated and clinically useful. The developed models are presented as a web-based calculator (https://cpmodel.shinyapps.io/SCLM/) and nomograms.
Conclusions
FDG metabolic parameter-based prognostic models are well-calibrated recurrence prediction models with good discriminative power. They can be used for accurate risk stratification in patients with SCLM.
Key Points
• In this multicenter study, we developed and validated prediction models for recurrence in patients with resectable synchronous colorectal cancer liver metastasis using a metabolic parameter from FDG PET-CT.
• The developed models showed good predictive performance on external validation, significantly exceeding that of a pre-existing model.
• The models may be utilized for accurate patient risk stratification, thereby aiding in therapeutic decision-making.




Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the receiver-operating characteristic curve
- CI95% :
-
95% confidence interval
- CLM:
-
Colorectal cancer liver metastasis
- FCRS:
-
Fong’s clinical risk score
- FDG:
-
2-[18F]fluoro-2-deoxy-D-glucose
- M/P ratio:
-
Metastasis-to-primary-tumor uptake ratio
- nSUVpeak :
-
Normalized peak standardized uptake value
- RFS:
-
Recurrence-free survival
- SCLM:
-
Synchronous colorectal cancer liver metastasis
- SUV:
-
Standardized uptake value
- SUVpeak :
-
Peak standardized uptake value
References
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
van der Pool AEM, Damhuis RA, Ijzermans JNM et al (2012) Trends in incidence, treatment and survival of patients with stage IV colorectal cancer: a population-based series. Colorectal Dis 14:56–61
Chow FCL, Chok KSH (2019) Colorectal liver metastases: an update on multidisciplinary approach. World J Hepatol 11:150–172
Zarour LR, Anand S, Billingsley KG et al (2017) Colorectal cancer liver metastasis: evolving paradigms and future directions. Cell Mol Gastroenterol Hepatol 3:163–173
House MG, Ito H, Gönen M et al (2010) Survival after hepatic resection for metastatic colorectal cancer: trends in outcomes for 1,600 patients during two decades at a single institution. J Am Coll Surg 210:744–752
Andres A, Majno PE, Morel P et al (2008) Improved long-term outcome of surgery for advanced colorectal liver metastases: reasons and implications for management on the basis of a severity score. Ann Surg Oncol 15:134–143
Adam R, de Gramont A, Figueras J et al (2015) Managing synchronous liver metastases from colorectal cancer: a multidisciplinary international consensus. Cancer Treat Rev 41:729–741
Hashiguchi Y, Muro K, Saito Y et al (2020) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol 25:1–42
Moris D, Tsilimigras DI, Machairas N et al (2019) Laparoscopic synchronous resection of colorectal cancer and liver metastases: a systematic review. J Surg Oncol 119:30–39
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144:646–674
Xia Q, Liu J, Wu C et al (2015) Prognostic significance of 18FDG PET/CT in colorectal cancer patients with liver metastases: a meta-analysis. Cancer Imaging 15:19
Lee HS, Kim HO, Hong YS et al (2014) Prognostic value of metabolic parameters in patients with synchronous colorectal cancer liver metastasis following curative-intent colorectal and hepatic surgery. J Nucl Med 55:582–589
Van Cutsem E, Cervantes A, Adam R et al (2016) ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol 27:1386–1422
Boellaard R, Delgado-Bolton R, Oyen WJG, et al (2014) FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging 42:328–354
Mahar AL, Compton C, Halabi S et al (2017) Personalizing prognosis in colorectal cancer: a systematic review of the quality and nature of clinical prognostic tools for survival outcomes. J Surg Oncol 116:969–982
Pavlou M, Ambler G, Seaman SR et al (2015) How to develop a more accurate risk prediction model when there are few events. BMJ 351:7–11
Collins GS, Ogundimu EO, Altman DG (2016) Sample size considerations for the external validation of a multivariable prognostic model: A resampling study. Stat Med 35:214–226
Pencina MJ, D’Agostino RB, Steyerberg EW (2011) Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med 30:11–21
Chang W, Cheng J, Allaire JJ, et al (2021) shiny: Web Application Framework for R. R package version 1.5.0. https://CRAN.R-project.org/package=shiny
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: Analysis of 1001 consecutive cases. Ann Surg 230:309–321
Rahman MS, Ambler G, Choodari-Oskooei B, Omar RZ (2017) Review and evaluation of performance measures for survival prediction models in external validation settings. BMC Med Res Methodol 17:60
Royston P, Altman DG (2013) External validation of a Cox prognostic model: Principles and methods. BMC Med Res Methodol 13:33
Vickers AJ, Elkin EB (2006) Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making 26:565–574
Collins GS, Reitsma JB, Altman DG, Moons KGM (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. Ann Intern Med 162:55–63
Gregoire E, Hoti E, Gorden DL et al (2010) Utility or futility of prognostic scoring systems for colorectal liver metastases in an era of advanced multimodal therapy. Eur J Surg Oncol 36:568–574
Margonis GA, Sasaki K, Gholami S et al (2018) Genetic And Morphological Evaluation (GAME) score for patients with colorectal liver metastases. Br J Surg 105:1210–1220
Brudvik KW, Jones RP, Giuliante F et al (2019) RAS mutation clinical risk score to predict survival after resection of colorectal liver metastases. Ann Surg 269:120–126
Paredes AZ, Hyer JM, Tsilimigras DI et al (2020) A novel machine-learning approach to predict recurrence after resection of colorectal liver metastases. Ann Surg Oncol 27:5139–5147
André T, Shiu KK, Kim TW et al (2020) Pembrolizumab in microsatellite-instability–high advanced colorectal cancer. N Engl J Med 383:2207–2218
Funding
This study was supported by a grant of the Medical Data-Driven Hospital Support Project through the Korea Health Information Service (KHIS), funded by the Ministry of Health & Welfare, Republic of Korea; the Medical Research Promotion Program, through the GangNeung Asan Hospital, funded by the Asan Foundation (2021IB001); the National Research Foundation of Korea (NRF) grant, funded by the Korean government (MSIT) (2021R1G1A1009606); and the research grant from Korea University (K2023081).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantors of this publication are Hyo Sang Lee and Ji Sung Lee.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Ji Sung Lee (a PhD statistician) kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects (120 patients in the development cohort) have been previously reported in J Nucl Med. 2014; 55(4):582-9. The previous study was a prognostic marker study that analyzed the prognostic value of FDG metabolic parameters. The current study is about the prognostic modelling using the FDG metabolic parameter, which is the natural extension of the previous study.
Methodology
• retrospective
• prognostic study
• multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Hyo Sang Lee and Hyun Woo Kwon equally share first-authorship.
Supplementary information
ESM 1
(DOCX 4313 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, H.S., Kwon, H.W., Lim, SB. et al. FDG metabolic parameter-based models for predicting recurrence after upfront surgery in synchronous colorectal cancer liver metastasis. Eur Radiol 33, 1746–1756 (2023). https://doi.org/10.1007/s00330-022-09141-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-09141-3