Abstracts
Objective
To investigate and compare the clinical outcomes between radiofrequency ablation (RFA) and thyroid lobectomy (TL) for T1bN0M0 papillary thyroid carcinoma (PTC).
Methods
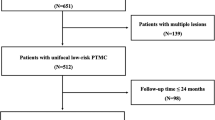
This retrospective study evaluated 283 patients with solitary T1bN0M0 PTC treated with RFA (RFA group, 91 patients) or TL (TL group, 192 patients) from May 2014 to November 2018. The patients were regularly followed up after treatment. Local tumor progression, lymph node metastasis (LNM), recurrent tumor, persistent tumor, recurrence-free survival (RFS), treatment variables (hospitalization, procedure time, estimated blood loss, and cost), complication, and delayed surgery were compared.
Results
During the follow-up (median [interquartile ranges], 50.4 [18.0] months), no significant differences were found in the local tumor progression (4.4% vs 3.6%, p = 1.000), LNM (1.1% vs 2.1%, p = 0.917), recurrent tumor (2.2% vs 1.6%, p = 1.000), persistent tumor (1.1% vs 0%, p = 0.146), and RFS rate (95.6% vs 96.4%, p = 0.816) in the RFA and TL groups. Distant metastasis was not detected. Patients in the RFA group had a shorter hospitalization (0 vs 7.0 [3.0] days, p < 0.001), shorter procedure time (5.6 [2.9] vs 90.0 [38.5] min, p < 0.001), lower estimated blood loss (0 vs 20 [20] mL, p < 0.001), lower cost ($1972.5 [0.1] vs $2362.4 [1009.3], p < 0.001), and lower complication rate (0 vs 12/192 [6.3%], p = 0.015) than those in the TL group. No patients in the RFA group underwent delayed surgery.
Conclusions
This study revealed comparable 4-year clinical outcomes between RFA and TL for T1bN0M0 PTC in terms of local tumor progression and RFS. As a minimally invasive modality, RFA may be a promising feasible alternative to surgery for the treatment of T1bN0M0 PTC in selected patients after strict evaluation.
Key Points
• No significant difference in local tumor progression and RFS was found between RFA and TL for T1bN0M0 PTC during a median follow-up period of 50.4 months.
• Compared with TL, RFA led to a shorter hospitalization, lower estimated blood loss, lower cost, and lower complication rate.
• RFA may be a promising feasible alternative to surgery for the treatment of T1bN0M0 PTC in selected patients after strict evaluation.




Similar content being viewed by others
Abbreviations
- AS:
-
Active surveillance
- CECT:
-
Contrast-enhanced computed tomography
- CEUS:
-
Contrast-enhanced ultrasound
- CNB:
-
Core-needle biopsy
- CND:
-
Central neck dissection
- ETE:
-
Extrathyroidal extension
- FNA:
-
Fine-needle aspiration
- LNM:
-
Lymph node metastasis
- PTC:
-
Papillary thyroid carcinoma
- RFA:
-
Radiofrequency ablation
- RFS:
-
Recurrence-free survival
- RLN:
-
Recurrent laryngeal nerve
- TL:
-
Thyroid lobectomy
- US:
-
Ultrasound
References
Sung H, Ferlay J, Siegel RL et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249
Haugen BR, Alexander EK, Bible KC et al (2015) 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid 26:1–133
Mauri G, Hegedüs L, Bandula S et al (2021) European Thyroid Association and Cardiovascular and Interventional Radiological Society of Europe 2021 clinical practice guideline for the use of minimally invasive treatments in malignant thyroid lesions. Eur Thyroid J 10:185–197
Tuttle RM, Haugen B, Perrier ND (2017) Updated American Joint Committee on Cancer/Tumor-Node-Metastasis staging system for differentiated and anaplastic thyroid cancer (eighth edition): what changed and why? Thyroid 27:751–756
Nickel B, Tan T, Cvejic E et al (2019) Health-related quality of life after diagnosis and treatment of differentiated thyroid cancer and association with type of surgical treatment. JAMA Otolaryngol Head Neck Surg 145:231–238
Tuttle RM, Zhang L, Shaha A (2018) A clinical framework to facilitate selection of patients with differentiated thyroid cancer for active surveillance or less aggressive initial surgical management. Expert Rev Endocrinol Metab 13:77–85
Sakai T, Sugitani I, Ebina A et al (2019) Active surveillance for T1bN0M0 papillary thyroid carcinoma. Thyroid 29:59–63
Tuttle RM, Fagin JA, Minkowitz G et al (2017) Natural history and tumor volume kinetics of papillary thyroid cancers during active surveillance. JAMA Otolaryngol Head Neck Surg 143:1015–1020
Cho SJ, Suh CH, Baek JH et al (2019) Active surveillance for small papillary thyroid cancer: a systematic review and meta-analysis. Thyroid 29:1399–1408
Kim JH, Baek JH, Lim HK et al (2018) 2017 thyroid radiofrequency ablation guideline: Korean Society of Thyroid Radiology. Korean J Radiol 19:632–655
Cao XJ, Liu J, Zhu YL et al (2021) Efficacy and safety of thermal ablation for solitary T1bN0M0 papillary thyroid carcinoma: a multicenter study. J Clin Endocrinol Metab 106:e573–e581
Xiao J, Zhang M, Zhang Y et al (2020) Efficacy and safety of ultrasonography-guided radiofrequency ablation for the treatment of T1bN0M0 papillary thyroid carcinoma: a retrospective study. Int J Hyperthermia 37:392–398
Cao X J, Wang S R, Che Y et al (2021) Efficacy and safety of thermal ablation for treatment of solitary T1N0M0 papillary thyroid carcinoma: a multicenter retrospective study. Radiology 202735
Xiao J, Zhang Y, Zhang M et al (2021) Ultrasonography-guided radiofrequency ablation vs. surgery for the treatment of solitary T1bN0M0 papillary thyroid carcinoma: a comparative study. Clin Endocrinol (Oxf) 94:684–691
He H, Wu R, Zhao J, Song Q, Zhang Y, Luo Y (2021) Ultrasound-guided radiofrequency ablation versus surgical resection for the treatment of T1bN0M0 papillary thyroid carcinoma in different age groups. Front Endocrinol (Lausanne) 12
Mauri G, Pacella CM, Papini E et al (2019) Image-guided thyroid ablation: proposal for standardization of terminology and reporting criteria. Thyroid 29:611–618
Zhang Y, Zhang X, Li J, Cai Q, Qiao Z, Luo YK (2021) Contrast-enhanced ultrasound: a valuable modality for extracapsular extension assessment in papillary thyroid cancer. Eur Radiol 31:4568–4575
Cho SJ, Baek SM, Lim HK, Lee KD, Son JM, Baek JH (2020) Long-term follow-up results of ultrasound-guided radiofrequency ablation for low-risk papillary thyroid microcarcinoma: more than 5-year follow-up for 84 tumors. Thyroid 30:1745–1751
Zhang M, Luo Y, Zhang Y, Tang J (2016) Efficacy and safety of ultrasound-guided radiofrequency ablation for treating low-risk papillary thyroid microcarcinoma: a prospective study. Thyroid 26:1581–1587
Chen J, Cao J, Qiu F, Huang P (2019) The efficacy and the safety of ultrasound-guided ablation therapy for treating papillary thyroid microcarcinoma. J Cancer 10:5272–5282
Ge MH, Xu D, Yang AK et al (2018) Expert consensus on thermal ablation for thyroid benign nodes, mocrocarcinoma and metastatic cervical lymph nodes (2018 edition). China Cancer 27(10):768–773 (In Chinese)
Zhang M, Tufano RP, Russell JO et al (2020) Ultrasound-guided radiofrequency ablation versus surgery for low-risk papillary thyroid microcarcinoma: results of over 5 years’ follow-up. Thyroid 30:408–417
Anuwong A, Ketwong K, Jitpratoom P, Sasanakietkul T, Duh QY (2018) Safety and outcomes of the transoral endoscopic thyroidectomy vestibular approach. JAMA Surg 153:21–27
Sugitani I, Ito Y, Takeuchi D et al (2021) Indications and strategy for active surveillance of adult low-risk papillary thyroid microcarcinoma: consensus statements from the Japan Association of Endocrine Surgery Task Force on Management for Papillary Thyroid Microcarcinoma. Thyroid 31:183–192
Sawka AM, Ghai S, Yoannidis T et al (2020) A prospective mixed-methods study of decision-making on surgery or active surveillance for low-risk papillary thyroid cancer. Thyroid 30:999–1007
Pham KN, Cullen J, Hurwitz LM et al (2016) Prospective quality of life in men choosing active surveillance compared to those biopsied but not diagnosed with prostate cancer. J Urol 196:392–398
Ito Y, Miyauchi A, Inoue H et al (2010) An observational trial for papillary thyroid microcarcinoma in Japanese patients. World J Surg 34:28–35
Ito Y, Uruno T, Nakano K et al (2003) An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid. Thyroid 13:381–387
Haser GC, Tuttle RM, Su HK et al (2016) Active surveillance for papillary thyroid microcarcinoma: new challenges and opportunities for the health care system. Endocr Pract 22:602–611
Sawka AM, Ghai S, Rotstein L et al (2022) A quantitative analysis examining patients’ choice of active surveillance or surgery for managing low-risk papillary thyroid cancer. Thyroid 32:255–262
McDow AD, Roman BR, Saucke MC et al (2021) Factors associated with physicians’ recommendations for managing low-risk papillary thyroid cancer. Am J Surg 222:111–118
Nickel B, Brito JP, Barratt A, Jordan S, Moynihan R, McCaffery K (2017) Clinicians’ views on management and terminology for papillary thyroid microcarcinoma: a qualitative study. Thyroid 27:661–671
Oh HS, Kwon H, Song E et al (2019) Tumor volume doubling time in active surveillance of papillary thyroid carcinoma. Thyroid 29:642–649
Morris LG, Wong RJ, Tuttle RM (2016) Ethical considerations when counseling patients with thyroid cancer about surgery vs observation. JAMA Otolaryngol Head Neck Surg 142:406–407
Oh HS, Ha J, Kim HI et al (2018) Active surveillance of low-risk papillary thyroid microcarcinoma: a multi-center cohort study in Korea. Thyroid 28:1587–1594
Mauri G, Orsi F, Carriero S et al (2020) Image-guided thermal ablation as an alternative to surgery for papillary thyroid microcarcinoma: preliminary results of an Italian experience. Front Endocrinol (Lausanne) 11:575152
Gärtner FR, Portielje JE, Langendam M et al (2019) Role of patient preferences in clinical practice guidelines: a multiple methods study using guidelines from oncology as a case. BMJ Open 9:e032483
Stiggelbout AM, Van der Weijden T, De Wit MP et al (2012) Shared decision making: really putting patients at the centre of healthcare. BMJ 344:e256
Russo S, Jongerius C, Faccio F et al (2019) Understanding patients’ preferences: a systematic review of psychological instruments used in patients’ preference and decision studies. Value Health 22:491–501
Zhou W, Jiang S, Zhan W, Zhou J, Xu S, Zhang L (2017) Ultrasound-guided percutaneous laser ablation of unifocal T1N0M0 papillary thyroid microcarcinoma: preliminary results. Eur Radiol 27:2934–2940
Teng DK, Li WH, Du JR, Wang H, Yang DY, Wu XL (2020) Effects of microwave ablation on papillary thyroid microcarcinoma: a five-year follow-up report. Thyroid 30:1752–1758
Yue WW, Qi L, Wang DD et al (2020) US-guided microwave ablation of low-risk papillary thyroid microcarcinoma: longer-term results of a prospective study. J Clin Endocrinol Metab 105
Li J, Liu Y, Liu J, Qian L (2018) Ultrasound-guided percutaneous microwave ablation versus surgery for papillary thyroid microcarcinoma. Int J Hyperthermia 34:653–659
Li J, Liu Y, Liu J, Yang P, Hu X, Qian L (2019) A comparative study of short-term efficacy and safety for thyroid micropapillary carcinoma patients after microwave ablation or surgery. Int J Hyperthermia 36:640–646
Zhou W, Ni XF, Xu SY, Zhang L, Chen YD, Zhan WW (2019) Ultrasound-guided laser ablation versus surgery for solitary papillary thyroid microcarcinoma: a retrospective study. Int J Hyperthermia 36:897–904
Yan L, Zhang M, Song Q, Luo Y (2021) Ultrasound-guided radiofrequency ablation versus thyroid lobectomy for low-risk papillary thyroid microcarcinoma: a propensity-matched cohort study of 884 patients. Thyroid 31:1662–1672
Yan L, Lan Y, Xiao J, Lin L, Jiang B, Luo Y (2021) Long-term outcomes of radiofrequency ablation for unifocal low-risk papillary thyroid microcarcinoma: a large cohort study of 414 patients. Eur Radiol 31:685–694
Cho SJ, Baek SM, Na DG, Lee KD, Shong YK, Baek JH (2021) Five-year follow-up results of thermal ablation for low-risk papillary thyroid microcarcinomas: systematic review and meta-analysis. Eur Radiol 31:6446–6456
Cho SJ, Baek JH, Chung SR, Choi YJ, Lee JH (2019) Thermal ablation for small papillary thyroid cancer: a systematic review. Thyroid 29:1774–1783
Baek JH, Cho SJ (2021) Thermal ablation for small papillary thyroid cancer: a potential game changer. Radiology:210424
Yeh MW, Bauer AJ, Bernet VA et al (2015) American Thyroid Association statement on preoperative imaging for thyroid cancer surgery. Thyroid 25:3–14
Suh CH, Baek JH, Choi YJ, Lee JH (2017) Performance of CT in the preoperative diagnosis of cervical lymph node metastasis in patients with papillary thyroid cancer: a systematic review and meta-analysis. AJNR Am J Neuroradiol 38:154–161
Baek JH, Lee JH, Sung JY et al (2012) Complications encountered in the treatment of benign thyroid nodules with US-guided radiofrequency ablation: a multicenter study. Radiology 262:335–342
Jung SL, Baek JH, Lee JH et al (2018) Efficacy and safety of radiofrequency ablation for benign thyroid nodules: a prospective multicenter study. Korean J Radiol 19:167–174
Ma B, Wei W, Xu W et al (2018) Surgical confirmation of incomplete treatment for primary papillary thyroid carcinoma by percutaneous thermal ablation: a retrospective case review and literature review. Thyroid 28:1134–1142
Yan L, Luo Y, Zhang Y et al (2020) The clinical application of core-needle biopsy after radiofrequency ablation for low-risk papillary thyroid microcarcinoma: a large cohort of 202 patients study. J Cancer 11:5257–5263
Kim JH, Yoo WS, Park YJ et al (2015) Efficacy and safety of radiofrequency ablation for treatment of locally recurrent thyroid cancers smaller than 2 cm. Radiology 276:909–918
Chu KF, Dupuy DE (2014) Thermal ablation of tumours: biological mechanisms and advances in therapy. Nat Rev Cancer 14:199
Ha SM, Shin JY, Baek JH et al (2019) Does radiofrequency ablation induce neoplastic changes in benign thyroid nodules: a preliminary study. Endocrinol Metab (Seoul) 34:169–178
Lee SJ, Jung SL, Kim BS et al (2014) Radiofrequency ablation to treat loco-regional recurrence of well-differentiated thyroid carcinoma. Korean J Radiol 15:817–826
Guang Y, Luo Y, Zhang Y et al (2017) Efficacy and safety of percutaneous ultrasound guided radiofrequency ablation for treating cervical metastatic lymph nodes from papillary thyroid carcinoma. J Cancer Res Clin Oncol 143:1555–1562
Funding
No funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Yukun Luo.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional review board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yan, L., Li, X., Li, Y. et al. Comparison of ultrasound-guided radiofrequency ablation versus thyroid lobectomy for T1bN0M0 papillary thyroid carcinoma. Eur Radiol 33, 730–740 (2023). https://doi.org/10.1007/s00330-022-08963-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08963-5