Abstract
Objective
To explore whether magnetic susceptibility value (MSV) and radiomics features of the nigrostriatal system could be used as imaging markers for diagnosing Parkinson’s disease (PD) and its related cognitive impairment (CI).
Methods
A total of 104 PD patients and 45 age-sex-matched healthy controls (HCs) underwent quantitative susceptibility mapping (QSM). The former completed Hoehn-Yahr Stage and Montreal Cognitive Assessment (MoCA). The patients were divided into several subgroups according to disease stages, courses, and MoCA scores. The ROI was subdivided into the substantia nigra (SN), head of caudate nucleus (HCN), and putamen. The MSVs and radiomics features were obtained from QSM. The multivariable logistic regression (MLR) and support vector machine (SVM) models were constructed to diagnose PD. The correlations between MSVs, radiomics features, and MoCA scores were evaluated.
Results
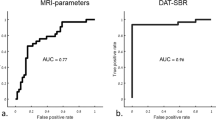
The MSVs in bilateral SN pars compacta (SNc) of PD patients were higher than those of the HCs (p < 0.001). There were differences in some radiomics features between the two groups (p < 0.05). The MSVs of the right SNc and the radiomics features of the right SN had the highest area under the curve (AUC), respectively. The comprehensive MLR model (0.90) and SVM model (0.95) revealed better classification performance than MSVs (p < 0.05) in diagnosing PD. The MSVs from the HCN were negatively correlated with MoCA scores in PD subgroups. There were correlations between radiomics features and MoCA scores in PD patients.
Conclusions
Radiomics features and MSVs of the nigrostriatal system from QSM could have crucial role in diagnosing PD and assessing CI.
Key Points
• The MLR and the SVM models have excellent diagnostic performance in the diagnosis of PD.
• A PD diagnostic nomogram, created based on MSV and the radiomics scores of SVM model, is very convenient for clinical use.
• The radiomics features of the nigrostriatal system based on QSM help to evaluate the cognitive impairment in PD patients.



Similar content being viewed by others
Abbreviations
- CI:
-
Cognitive impairment
- HC:
-
Healthy control
- HCN:
-
Head of caudate nucleus
- H-Y:
-
Hoehn-Yahr
- MLR:
-
Multivariate logistic regression
- MoCA:
-
Montreal Cognitive Assessment
- MSV:
-
Magnetic susceptibility value
- PD:
-
Parkinson’s disease
- PUT:
-
Putamen
- QSM:
-
Quantitative susceptibility mapping
- SN:
-
Substantia nigra
- SNc:
-
SN pars compacta
- SNr:
-
SN pars reticulata
- SVM:
-
Support vector machine
References
Tysnes OB, Storstein A (2017) Epidemiology of Parkinson’s disease. J Neural Transm (Vienna) 124:901–905
Acosta-Cabronero J, Cardenas-Blanco A, Betts MJ et al (2017) The whole-brain pattern of magnetic susceptibility perturbations in Parkinson’s disease. Brain 140:118–131
An H, Zeng X, Niu T et al (2018) Quantifying iron deposition within the substantia nigra of Parkinson’s disease by quantitative susceptibility mapping. J Neurol Sci 386:46–52
Ghassaban K, He N, Sethi SK et al (2019) Regional high iron in the substantia nigra differentiates Parkinson’s disease patients from healthy controls. Front Aging Neurosci. https://doi.org/10.3389/fnagi.2019.00106
Deistung A, Schweser F, Reichenbach JR et al (2017) Overview of quantitative susceptibility mapping. NMR Biomed. https://doi.org/10.1002/nbm.3569
Aggarwal M, Li X, Gröhn O, Sierra A (2018) Nuclei-specific deposits of iron and calcium in the rat thalamus after status epilepticus revealed with quantitative susceptibility mapping (QSM). J Magn Reson Imaging 47:554–564
Chen L, Cai C, Yang T et al (2017) Changes in brain iron concentration after exposure to high-altitude hypoxia measured by quantitative susceptibility mapping. Neuroimage 147:488–499
Li H, Gao L, Ma H et al (2021) Radiomics-based features for prediction of histological subtypes in central lung cancer. Front Oncol. https://doi.org/10.3389/fonc.2021.658887
Xiao B, He N, Wang Q et al (2019) Quantitative susceptibility mapping based hybrid feature extraction for diagnosis of Parkinson’s disease. Neuroimage Clin. https://doi.org/10.1016/j.nicl.2019.102070
Shu ZY, Cui SJ, Wu X et al (2021) Predicting the progression of Parkinson’s disease using conventional MRI and machine learning: an application of radiomic biomarkers in whole-brain white matter. Magn Reson Med 85:1611–1624
Salmanpour MR, Shamsaei M, Saberi A, Hajianfar G, Soltanian-Zadeh H, Rahmim A (2021) Robust identification of Parkinson’s disease subtypes using radiomics and hybrid machine learning. Comput Biol Med. https://doi.org/10.1016/j.compbiomed.2020.104142
Monastero R, Cicero CE, Baschi R et al (2018) Mild cognitive impairment in Parkinson’s disease: the Parkinson’s disease cognitive study (PACOS). J Neurol 265:1050–1058
Baschi R, Restivo V, Nicoletti A et al (2019) Mild behavioral impairment in Parkinson’s disease: data from the Parkinson’s Disease Cognitive Impairment Study (PACOS). J Alzheimers Dis 68:1603–1610
Uchida Y, Kan H, Sakurai K et al (2019) Voxel-based quantitative susceptibility mapping in Parkinson’s disease with mild cognitive impairment. Mov Disord 34:1164–1173
Thomas GEC, Leyland LA, Schrag AE, Lees AJ, Acosta-Cabronero J, Weil RS (2020) Brain iron deposition is linked with cognitive severity in Parkinson’s disease. J Neurol Neurosurg Psychiatry 91:418–425
Li DTH, Hui ES, Chan Q et al (2018) Quantitative susceptibility mapping as an indicator of subcortical and limbic iron abnormality in Parkinson’s disease with dementia. Neuroimage Clin 20:365–373
Betrouni N, Lopes R, Defebvre L, Leentjens AFG, Dujardin K (2020) Texture features of magnetic resonance images: a marker of slight cognitive deficits in Parkinson’s disease. Mov Disord 35:486–494
Postuma RB, Berg D, Stern M et al (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30:1591–1601
Smith GS, Mills KA, Pontone GM et al (2019) Effect of STN DBS on vesicular monoamine transporter 2 and glucose metabolism in Parkinson’s disease. Parkinsonism Relat Disord 64:235–241
Dowling P, Klinker F, Stadelmann C et al (2011) Dopamine D3 receptor specifically modulates motor and sensory symptoms in iron-deficient mice. J Neurosci 31:70–77
Verschuur CVM, Suwijn SR, Boel JA et al (2019) Randomized delayed-start trial of levodopa in Parkinson’s disease. N Engl J Med 380:315–324
Dalrymple-Alford JC, MacAskill MR, Nakas CT et al (2010) The MoCA: well-suited screen for cognitive impairment in Parkinson disease. Neurology 75:1717–1725
van Griethuysen JJM, Fedorov A, Parmar C et al (2017) Computational radiomics system to decode the radiographic phenotype. Cancer Res 77(21):e104–e107
Ma DN, Gao XY, Dan YB et al (2020) Evaluating solid lung adenocarcinoma anaplastic lymphoma kinase gene rearrangement using noninvasive radiomics biomarkers. Onco Targets Ther 13:6927–6935
Mazzucchi S, Frosini D, Costagli M et al (2019) Quantitative susceptibility mapping in atypical Parkinsonisms. Neuroimage Clin. https://doi.org/10.1016/j.nicl.2019.101999
Shahmaei V, Faeghi F, Mohammdbeigi A, Hashemi H, Ashrafi F (2019) Evaluation of iron deposition in brain basal ganglia of patients with Parkinson’s disease using quantitative susceptibility mapping. Eur J Radiol Open 6:169–174
Liu P, Wang H, Zheng S, Zhang F, Zhang X (2020) Parkinson’s disease diagnosis using neostriatum radiomic features based on T2-weighted magnetic resonance imaging. Front Neurol. https://doi.org/10.3389/fneur.2020.00248
Cao X, Wang X, Xue C, Zhang S, Huang Q, Liu W (2020) A radiomics approach to predicting Parkinson’s disease by incorporating whole-brain functional activity and gray matter structure. Front Neurosci. https://doi.org/10.3389/fnins.2020.00751
Uchida Y, Kan H, Sakurai K et al (2020) Magnetic susceptibility associates with dopaminergic deficits and cognition in Parkinson’s disease. Mov Disord 35:1396–1405
Wang N, Liu XL, Li L et al (2021) Screening for early-stage Parkinson’s disease: swallow tail sign on MRI susceptibility map-weighted images compared with PET. J Magn Reson Imaging 53(3):722–730
Piccardo A, Cappuccio R, Bottoni G et al (2021) The role of the deep convolutional neural network as an aid to interpreting brain [18F] DOPA PET/CT in the diagnosis of Parkinson's disease [J]. Eur Radiol 31(9):7003–7011
Cheng Z, Zhang J, He N et al (2019) Radiomic features of the nigrosome-1 region of the substantia nigra: using quantitative susceptibility mapping to assist the diagnosis of idiopathic Parkinson’s disease. Front Aging Neurosci. https://doi.org/10.3389/fnagi.2019.00167
Shu Z, Pang P, Wu X, Cui S, Xu Y, Zhang M (2020) An integrative nomogram for identifying early-stage Parkinson’s disease using non-motor symptoms and white matter-based radiomics biomarkers from whole-brain MRI. Front Aging Neurosci. https://doi.org/10.3389/fnagi.2020.548616
Kim JS, Oh YS, Lee KS, Kim YI, Yang DW, Goldstein DS (2012) Association of cognitive dysfunction with neurocirculatory abnormalities in early Parkinson disease. Neurology 79(13):1323–1331
Apostolova LG, Beyer M, Green AE et al (2010) Hippocampal, caudate, and ventricular changes in Parkinson’s disease with and without dementia. Mov Disord 25:687–695
Pasquini J, Durcan R, Wiblin L et al (2019) Clinical implications of early caudate dysfunction in Parkinson’s disease. J Neurol Neurosurg Psychiatry 90:1098–1104
Rahmim A, Salimpour Y, Jain S et al (2016) Application of texture analysis to DAT SPECT imaging: relationship to clinical assessments. Neuroimage Clin 12:e1–e9
Jin ZJ, Wang Y, Jokar M et al (2022) Automatic detection of neuromelanin and iron in the midbrain nuclei using a magnetic resonance imaging-based brain template. Hum Brain Mapp. https://doi.org/10.1002/hbm.25770
Lewis MM, Du GW, Kidacki M et al (2013) Higher iron in the red nucleus marks Parkinson’s dyskinesia. Neurobiol Aging 34:1497–1503
Acknowledgements
We would like to thank the radiographers in Affiliated Hospital of Nantong University for their professional assistance and MRI scans.
Funding
This study has received funding by the Jiangsu Provincial Health Commission (No. H2019089) and the Nantong Science and Technology Project (No. MS12020044).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jin Juan Kang.
Conflict of interest
The authors declare no conflicts of interest.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects in this study.
Ethical approval
This study was approved by the institutional review board (Ethics Committee of Affiliated Hospital of Nantong University).
Methodology
• retrospective
• diagnostic and prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOC 81 kb)
Rights and permissions
About this article
Cite this article
Kang, J.J., Chen, Y., Xu, G.D. et al. Combining quantitative susceptibility mapping to radiomics in diagnosing Parkinson’s disease and assessing cognitive impairment. Eur Radiol 32, 6992–7003 (2022). https://doi.org/10.1007/s00330-022-08790-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08790-8