Abstract
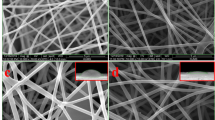
Advanced therapeutic dressings are the current research interest that achieves rapid and complete wound healing. The healing of skin wounds demonstrates a remarkable cellular function process that is distinct in nature and involves the interaction of various cells, growth factors, and cytokines. In this study, nanofibrous scaffolds were prepared using poly(ε-caprolactone) and polylactic acid as mat scaffolds. Also, copper nanoparticles (CuNPs) and curcumin were added to fabricate a hybrid nanocomposite scaffold using the electrospinning technique. The fabricated scaffolds were analyzed by scanning electron microscopy (SEM), transmission electron microscopy (TEM), tensile analysis, porosity, and water vapor transmission rate. SEM analysis proved the nanostructured fibers have suitable porosity without any beads. The presence of CuNPs in the PCL-Cu nanofibrous mat was confirmed by TEM analysis. The tensile test confirmed an increase and decrease in the elongation ratio by CuNPs and curcumin addition, respectively. The biocompatibility and cell attachment to the nanofibers were proved by MTT and DAPI staining which proved a significantly positive effect of curcumin in the cell growth. The scaffold can hinder both the gram-negative and gram-positive bacteria through direct contact with them. This research study showed that the addition of CuNPs and curcumin in the hybrid nanocomposite scaffold compensates for each other's shortcomings and has the potential to be used in wound healing applications.







Similar content being viewed by others
References
Boateng J, Catanzano O (2015) Advanced therapeutic dressings for effective wound healing—a review. J Pharm Sci 104:3653–3680. https://doi.org/10.1002/jps.24610
Shahriari-Khalaji M, Hu G, Chen L, Cao Z, Andreeva T, Xiong X, Krastev R, Hong FF (2021) Functionalization of aminoalkylsilane-grafted bacterial nanocellulose with ZnO-NPs-doped pullulan electrospun nanofibers for multifunctional wound dressing. ACS Biomater Sci Eng 7:3933–3946. https://doi.org/10.1021/acsbiomaterials.1c00444
Al-Alwany A (2021) Iatrogenic atrial septal defect post radiofrequency ablation in patients with left atrial SVT: predictors and outcomes. Revista Latinoamericana de Hipertension 15:185–191. https://doi.org/10.5281/zenodo.5651240
Velnar T, Bailey T, Smrkolj V (2009) The wound healing process: an overview of the cellular and molecular mechanisms. J Int Med Res 37:1528–1542. https://doi.org/10.1177/147323000903700531
Thu H-E, Zulfakar MH, Ng S-F (2012) Alginate based bilayer hydrocolloid films as potential slow-release modern wound dressing. Int J Pharm 434:375–383. https://doi.org/10.1016/j.ijpharm.2012.05.044
Al-Zuhairy SAS, Kadhum WR, Alhijjaj M, Kadhim MM, Al-Janabi AS, Salman AW, Al-Sharifi HKR, Khadom AA (2022) Development and evaluation of biocompatible topical petrolatum-liquid crystal formulations with enhanced skin permeation properties. J Oleo Sci 71:ess21344. https://doi.org/10.5650/jos.ess21344
Hjazi A (2023) The effects of Capsicum annuum supplementation on lipid profiles in adults with metabolic syndrome and related disorders: a systematic review and meta-analysis of randomized controlled trials. Phytother Res 37:3859–3866. https://doi.org/10.1002/ptr.7922
Percival NJ (2002) Classification of wounds and their management. Surg Infect 20:114–117. https://doi.org/10.1383/surg.20.5.114.14626
Tottoli EM, Dorati R, Genta I, Chiesa E, Pisani S (2020) Skin wound healing process and new emerging technologies for skin wound care and regeneration. Pharmaceutics 12(8):735
Kadhum WR, See GL, Alhijjaj M, Kadhim MM, Arce FJ, Al-Janabi AS, Al-Rashidi RR, Khadom AA (2022) Evaluation of the skin permeation-enhancing abilities of newly developed water-soluble self-assembled liquid crystal formulations based on hexosomes. Crystals 12:1238. https://doi.org/10.3390/cryst12091238
Enoch S, Leaper DJ (2005) Basic science of wound healing. Surg Infect 23:37–42. https://doi.org/10.1383/surg.23.2.37.60352
Boateng JS, Matthews KH, Stevens HNE, Eccleston GM (2008) Wound healing dressings and drug delivery systems: a review. J Pharm Sci 97:2892–2923. https://doi.org/10.1002/jps.21210
Chen D, Hou Q, Zhong L, Zhao Y, Li M, Fu X (2019) Review article bioactive molecules for skin repair and regeneration : progress and perspectives. Stem Cells Int 2019:6789823
Liu M, Duan X-P, Li Y-M, Yang D-P, Long Y-Z (2017) Electrospun nanofibers for wound healing. Mater Sci Eng, C 76:1413–1423. https://doi.org/10.1016/j.msec.2017.03.034
Naghavi Alhosseini S, Moztarzadeh F, Karkhaneh A, Dodel M, Khalili M, Eslami Arshaghi T, Elahirad E, Mozafari M (2019) Improved cellular response on functionalized Polypyrrole interfaces. J Cellular Physiol 234:15279–15287. https://doi.org/10.1002/jcp.28173
Endo T, Inoue Y, Kato S, Kaminaka H, Ifuku S (2023) Effects of chitin nanofiber application on plant growth and its differences by soil type. Asian J Agricult Rural Develop 13:163–172. https://doi.org/10.55493/5005.v13i3.4820
Amiri H, Babapour A, Fallahi M, Azimi N, Hadidi A (2023) Optimization of energy in oil pipelines covered with nanofibers of phase change materials using CFD. Iran J Chem Chem Eng. https://doi.org/10.30492/ijcce.2023.2001283.6000
Zahedi P, Rezaeian I, Ranaei-Siadat S, Jafari S, Supaphol P (2010) A review on wound dressings with an emphasis on electrospun nanofibrous polymeric bandages. Polym Adv Technol 21:77–95. https://doi.org/10.1002/pat.1625
Meinel AJ, Germershaus O, Luhmann T, Merkle HP, Meinel L (2012) European Journal of Pharmaceutics and Biopharmaceutics Electrospun matrices for localized drug delivery : current technologies and selected biomedical applications. Eur J Pharm Biopharm 81:1–13. https://doi.org/10.1016/j.ejpb.2012.01.016
Kadhum WR, Al-Zuhairy SAS, Mohamed MBM, Abdulrahman AY, Kadhim MM, Alsadoon Z, Teoh TC (2021) A nanotechnological approach for enhancing the topical drug delivery by newly developed liquid crystal formulations. Int J Drug Delivery Technol 11:716–720. https://doi.org/10.25258/ijddt.11.3.11
Esmaeili E, Eslami-Arshaghi T, Hosseinzadeh S, Elahirad E, Jamalpoor Z, Hatamie S, Soleimani M (2020) The biomedical potential of cellulose acetate/polyurethane nanofibrous mats containing reduced graphene oxide/silver nanocomposites and curcumin: antimicrobial performance and cutaneous wound healing. Int J Biol Macromol 152:418–427. https://doi.org/10.1016/j.ijbiomac.2020.02.295
Hosseinzadeh S, Hamedi S, Esmaeili E, Kabiri M, Babaie A, Soleimani M, Ardeshirylajimi A (2019) Mucoadhesive nanofibrous membrane with anti-inflammatory activity. Polym Bull 76:4827–4840. https://doi.org/10.1007/s00289-018-2618-1
Altaher Y, Kandeel M (2022) Structure-activity relationship of anionic and cationic polyamidoamine (PAMAM) dendrimers against Staphylococcus aureus. J Nanomater 2022:1–5. https://doi.org/10.1155/2022/4013016
Santoro M, Shah SR, Walker JL, Mikos AG (2016) Poly(lactic acid) nanofibrous scaffolds for tissue engineering. Adv Drug Deliv Rev 107:206–212. https://doi.org/10.1016/j.addr.2016.04.019
Donya H, Darwesh R, Ahmed MK (2021) Morphological features and mechanical properties of nanofibers scaffolds of polylactic acid modified with hydroxyapatite/CdSe for wound healing applications. Int J Biol Macromol 186:897–908. https://doi.org/10.1016/j.ijbiomac.2021.07.073
Sharifi M, Bahrami SH, Nejad NH, Milan PB (2020) Electrospun PCL and PLA hybrid nanofibrous scaffolds containing Nigella sativa herbal extract for effective wound healing. J Appl Polym Sci 137:9–11. https://doi.org/10.1002/app.49528
Esmaeili E, Didekhani R, Gohari Z, Khalili M (2023) Fabrication and characterization of PCL@PAN nanofibrous scaffold containing nature-derived oyster shell for bone tissue engineering applications. Appl Phys A 129:670. https://doi.org/10.1007/s00339-023-06943-0
Khalili M, Keshvari H, Imani R, Sohi AN, Esmaeili E, Tajabadi M (2021) Study of osteogenic potential of electrospun <scp>PCL</scp> incorporated by dendrimerized superparamagnetic nanoparticles as a bone tissue engineering scaffold. Polym Adv Technol. https://doi.org/10.1002/pat.5555
Khalili M, Khalili A, Bokov DO, Golmirzaei M, Oleneva MS, Naghiaei N, Radmehr M, Esmaeili E (2022) Preparation and characterization of bi-layered polycaprolactone/polyurethane nanofibrous scaffold loaded with titanium oxide and curcumin for wound dressing applications. Appl Phys A 128:497. https://doi.org/10.1007/s00339-022-05646-2
Vonbrunn E, Mueller M, Pichlsberger M, Sundl M, Helmer A, Wallner SA, Rinner B, Tuca A-C, Kamolz L-P, Brislinger D, Glasmacher B, Lang-Olip I (2020) Electrospun PCL/PLA scaffolds are more suitable carriers of placental mesenchymal stromal cells than collagen/elastin scaffolds and prevent wound contraction in a mouse model of wound healing. Front Bioeng Biotechnol 8:1–16. https://doi.org/10.3389/fbioe.2020.604123
Patrício T, Bártolo P (2013) Thermal stability of PCL/PLA blends produced by physical blending process. Proc Eng 59:292–297. https://doi.org/10.1016/j.proeng.2013.05.124
Luo Y, Lin Z, Guo G (2019) Biodegradation assessment of poly (Lactic Acid) filled with functionalized Titania nanoparticles (PLA/TiO2) under compost conditions. Nanoscale Res Lett 14:56. https://doi.org/10.1186/s11671-019-2891-4
Nevoralová M, Koutný M, Ujčić A, Starý Z, Šerá J, Vlková H, Šlouf M, Fortelný I, Kruliš Z (2020) Structure characterization and biodegradation rate of Poly(ε-caprolactone)/Starch blends. Front Mater 7:1–14. https://doi.org/10.3389/fmats.2020.00141
Abbasi R, Shineh G, Mobaraki M, Doughty S, Tayebi L (2023) Structural parameters of nanoparticles affecting their toxicity for biomedical applications: a review. Netherlands. https://doi.org/10.1007/s11051-023-05690-w
Hosseini MR, Ahangari M, Johar MH, Allahkaram SR (2021) Optimization of nano HA-SiC coating on AISI 316L medical grade stainless steel via electrophoretic deposition. Mater Lett 285:129097. https://doi.org/10.1016/j.matlet.2020.129097
Esmaeili E, Ghiass MA, Vossoughi M, Soleimani M (2017) Hybrid magnetic-DNA directed immobilisation approach for efficient protein capture and detection on microfluidic platforms. Sci Rep 7:194. https://doi.org/10.1038/s41598-017-00268-8
Sabet M, Salavati-Niasari M, Esmaeili E (2016) Synthesis of zinc sulfide nanostructures with different sulfur sources via mild hydrothermal route: investigation of crystal phase and morphology. J Inorg Organomet Polym Mater 26:738–743. https://doi.org/10.1007/s10904-016-0374-y
Esmaeili E, Sabet M, Salavati-Niasari M, Zarghami Z, Bagheri S (2016) Effect of sulfur source on cadmium sulfide nanostructures morphologies via simple hydrothermal route. J Cluster Sci 27:351–360. https://doi.org/10.1007/s10876-015-0934-2
Qiu J, Wei WD (2014) Surface plasmon-mediated photothermal chemistry. J Phys Chem C 118:20735–20749. https://doi.org/10.1021/jp5042553
Salvo J, Sandoval C (2022) Role of copper nanoparticles in wound healing for chronic wounds: literature review. Burns & Trauma. 10:tkab047. https://doi.org/10.1093/burnst/tkab047
Sidhu GS, Singh AK, Thaloor D, Banaudha KK, Patnaik GK, Srimal RC, Maheshwari RK (1998) Enhancement of wound healing by curcumin in animals. Wound Repair Regeneration 6:167–177. https://doi.org/10.1046/j.1524-475X.1998.60211.x
Shefa AA, Sultana T, Park MK, Lee SY, Gwon JG, Lee BT (2020) Curcumin incorporation into an oxidized cellulose nanofiber-polyvinyl alcohol hydrogel system promotes wound healing. Mater Des 186:108313. https://doi.org/10.1016/j.matdes.2019.108313
Sharma D, Satapathy BK (2022) Optimization and physical performance evaluation of electrospun nanofibrous mats of PLA, PCL and their blends. J Ind Text 51:6640S-6665S. https://doi.org/10.1177/1528083720944502
Antunes BP, Moreira AF, Gaspar VM, Correia IJ (2015) Chitosan/arginine–chitosan polymer blends for assembly of nanofibrous membranes for wound regeneration. Carbohyd Polym 130:104–112. https://doi.org/10.1016/j.carbpol.2015.04.072
Ahmed L, Atif R, Eldeen TS, Yahya I, Omara A, Eltayeb M (2019) Study the using of nanoparticles as drug delivery system based on mathematical models for controlled release. Int J Latest Technol Eng Manag Appl Sci 8:52–56
Esmaeili E, Khalili M, Sohi AN, Hosseinzadeh S, Taheri B, Soleimani M (2019) Dendrimer functionalized magnetic nanoparticles as a promising platform for localized hyperthermia and magnetic resonance imaging diagnosis. J Cell Physiol 234:12615–12624. https://doi.org/10.1002/jcp.27849
Miguel S, Ribeiro M, Coutinho P, Correia I (2017) Electrospun Polycaprolactone/Aloe Vera_chitosan nanofibrous asymmetric membranes aimed for wound healing applications. Polymers 9:183. https://doi.org/10.3390/polym9050183
Luyt AS, Gasmi S (2018) Influence of TiO2 nanoparticles on the crystallization behaviour and tensile properties of biodegradable PLA and PCL nanocomposites. J Polym Environ 26:2410–2423. https://doi.org/10.1007/s10924-017-1142-y
Suamte L, Tirkey A, Barman J, Jayasekhar Babu P (2023) Various manufacturing methods and ideal properties of scaffolds for tissue engineering applications. Smart Mater Manufact 1:100011. https://doi.org/10.1016/j.smmf.2022.100011
Chen Y-P, Liu H-Y, Liu Y-W, Lee T-Y, Liu S-J (2019) Determination of electrospinning parameters’ strength in Poly(D, L)-lactide-co-glycolide micro/nanofiber diameter tailoring. J Nanomater 2019:1–8. https://doi.org/10.1155/2019/2626085
Yuan TT, DiGeorge Foushee AM, Johnson MC, Jockheck-Clark AR, Stahl JM (2018) Development of electrospun chitosan-polyethylene oxide/fibrinogen biocomposite for potential wound healing applications. Nanoscale Res Lett 13:88. https://doi.org/10.1186/s11671-018-2491-8
Oh E, Kim E, Park Y (2018) Evaluation of the moisture transfer property of waterproof breathable fabric under low-temperature conditions depending on the pore size and distribution. Cloth Text Res J 36:310–323. https://doi.org/10.1177/0887302X18783089
Prasad S, DuBourdieu D, Srivastava A, Kumar P, Lall R (2021) Metal-curcumin complexes in therapeutics: an approach to enhance pharmacological effects of curcumin. Int J Mol Sci 22:7094. https://doi.org/10.3390/ijms22137094
Gholami M, Zeighami H, Bikas R, Heidari A, Rafiee F, Haghi F (2020) Inhibitory activity of metal-curcumin complexes on quorum sensing related virulence factors of Pseudomonas aeruginosa PAO1. AMB Express 10:111. https://doi.org/10.1186/s13568-020-01045-z
Huo P, Han X, Zhang W, Zhang J, Kumar P, Liu B (2021) Electrospun nanofibers of Polycaprolactone/collagen as a sustained-release drug delivery system for artemisinin. Pharmaceutics 13:1228. https://doi.org/10.3390/pharmaceutics13081228
Griffitt RJ, Weil R, Hyndman KA, Denslow ND, Powers K, Taylor D, Barber DS (2007) Exposure to copper nanoparticles causes gill injury and acute lethality in Zebrafish ( Danio rerio ). Environ Sci Technol 41:8178–8186. https://doi.org/10.1021/es071235e
Pohanka M (2019) Copper and copper nanoparticles toxicity and their impact on basic functions in the body. Bratislava Med J 120:397–409. https://doi.org/10.4149/BLL_2019_065
Chatterjee AK, Chakraborty R, Basu T (2014) Mechanism of antibacterial activity of copper nanoparticles. Nanotechnology 25:135101. https://doi.org/10.1088/0957-4484/25/13/135101
Zheng D, Huang C, Huang H, Zhao Y, Khan MRU, Zhao H, Huang L (2020) Antibacterial mechanism of curcumin: a review. Chem Biodiver 17:e2000171. https://doi.org/10.1002/cbdv.202000171
Acknowledgements
Hereby, we extend our gratitude to the stem cell technology research center.
Funding
There are no funders to report for this submission.
Author information
Authors and Affiliations
Contributions
MK analyzed conceptualization, formal analysis, funding acquisition, investigation, methodology, project administration, validation, visualization, and writing—original draft. AA performed methodology, writing—original draft, and investigation. SM developed software and formal analysis. YQA provided data curation and original draft. EAMS prepared data curation. AARC did data curation. RMRP approved data curation. KP conducted data curation. MR revised review & editing. EE carried out conceptualization, project administration, funding acquisition, supervision, resources, formal analysis, validation, and writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khalili, M., Afrouzan, A., Mehrjou, S. et al. Preparation and characterization of nanofibrous scaffolds containing copper nanoparticles and curcumin for wound healing applications. Polym. Bull. (2024). https://doi.org/10.1007/s00289-024-05148-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00289-024-05148-6