Abstract
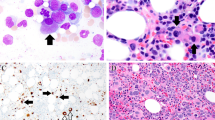
Extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT) lymphoma is a type of low-grade malignant B-cell lymphoma. The aim of this study was to investigate the clinicopathological characteristics of thymic MALT lymphoma. We analyzed the clinical, morphological, immunophenotypical, cytogenetic, and molecular characteristics of 11 cases of thymic MALT lymphoma. The relevant literature was also reviewed. The median age of the 11 patients was 50 (range: 33–60). There was a female predominance with a female-to-male ratio of 10:1. Three patients presented with Sjögren syndrome, autoimmune thrombocytopenia purpura, and type B1 thymoma, respectively. Microscopically, thymic MALT lymphoma was characterized by epithelium-lined cysts that were surrounded by small lymphocytes, centrocyte-like cells, and monocytoid B-cells. Plasmacytic differentiation was observed in two cases. The tumor cells expressed CD20, CD79α, and BCL2. Clonal immunoglobulin genes were detected in all 8 examined cases. Fluorescence in situ hybridization (FISH) for 18q21 was performed in 7 cases, and no translocations involving 18q21 were found. Targeted gene sequencing was performed in five cases with available DNA samples, and TNFAIP3, CARD11, IGLL5, and CCND3 mutations were identified. Thymic MALT lymphoma is a rare type of B cell malignancy with a female predominance and excellent clinical outcomes. Molecular aberrations involving the NF-κB pathway are frequent in thymic MALT lymphoma, suggesting that dysregulation of the NF-κB pathway is an important mechanism underlying the pathogenesis of thymic MALT lymphoma.


Similar content being viewed by others
References
Swerdlow SH, Campo E, Harris NL, et al (2017) WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. International Agency for Research on Cancer (IARC), Lyon, France
Raderer M, Wohrer S, Streubel B et al (2006) Assessment of disease dissemination in gastric compared with extragastric mucosa-associated lymphoid tissue lymphoma using extensive staging: a single-center experience [J]. J Clin Oncol 24(19):3136–3141
Raderer M, Kiesewetter B, Ferreri AJ (2016) Clinicopathologic characteristics and treatment of marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma)[J]. CA Cancer J Clin 66(2):153–171
Kominato S, Nakayama T, Sato F et al (2012) Characterization of chromosomal aberrations in thymic MALT lymphoma [J]. Pathol Int 62(2):93–98
Jung H, Yoo HY, Lee SH et al (2017) The mutational landscape of ocular marginal zone lymphoma identifies frequent alterations in TNFAIP3 followed by mutations in TBL1XR1 and CREBBP[J]. Oncotarget 8(10):17038–17049
Hyeon J, Lee B, Shin SH et al (2018) Targeted deep sequencing of gastric marginal zone lymphoma identified alterations of TRAF3 and TNFAIP3 that were mutually exclusive for MALT1 rearrangement[J]. Mod Pathol 31(9):1418–1428
Go H, Cho HJ, Paik JH et al (2011) Thymic extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue: a clinicopathological and genetic analysis of six cases[J]. Leuk Lymphoma 52(12):2276–2283
Wang L, Ying J, Xue L et al (2013) Clonality analysis in Castleman’s disease and its application in differential diagnosis. J Diag Pathol 20(7):397–400
Dubois S, Viailly PJ, Mareschal S et al (2016) Next-generation sequencing in diffuse large b-cell lymphoma highlights molecular divergence and therapeutic opportunities: a LYSA study[J]. Clin Cancer Res 22(12):2919–2928
Talwalkar SS, Valbuena JR, Abruzzo LV et al (2006) MALT1 gene rearrangements and NF-kappaB activation involving p65 and p50 are absent or rare in primary MALT lymphomas of the breast[J]. Mod Pathol 19(11):1402–1408
Inagaki H, Chan JK, Ng JW et al (2002) Primary thymic extranodal marginal-zone B-cell lymphoma of mucosa-associated lymphoid tissue type exhibits distinctive clinicopathological and molecular features[J]. Am J Pathol 160(4):1435–1443
Zaharie F, Pop LA, Petrushev B et al (2019) Next-generation sequencing-based characterization of the invasion by anatomical contiguity in a primary osseous diffuse large B-cell lymphoma. Correlation between the genetic profile of the malignancy and the clinical outcome of the patient[J]. Histol Histopathol 34(6):663–670
Karvounis E, Kappas I, Angelousi A et al (2020) Mucosa-associated lymphoid tissue lymphoma of the thyroid gland: a systematic review of the literature[J]. Eur Thyroid J 9(1):11–18
Du MQ (2016) MALT lymphoma: a paradigm of NF-kappaB dysregulation[J]. Semin Cancer Biol 39:49–60
Du MQ (2017) MALT lymphoma: genetic abnormalities, immunological stimulation and molecular mechanism[J]. Best Pract Res Clin Haematol 30(1–2):13–23
Vela V, Juskevicius D, Gerlach MM et al (2020) High throughput sequencing reveals high specificity of TNFAIP3 mutations in ocular adnexal marginal zone B-cell lymphomas[J]. Hematol Oncol 38(3):284–292
Moody S, Thompson JS, Chuang SS et al (2018) Novel GPR34 and CCR6 mutation and distinct genetic profiles in MALT lymphomas of different sites[J]. Haematologica 103(8):1329–1336
Nocturne G, Boudaoud S, Miceli-Richard C et al (2013) Germline and somatic genetic variations of TNFAIP3 in lymphoma complicating primary Sjogren’s syndrome[J]. Blood 122(25):4068–4076
Paul J, Soujon M, Wengner AM et al (2017) Simultaneous inhibition of PI3Kdelta and PI3Kalpha induces ABC-DLBCL regression by blocking BCR-dependent and -independent activation of NF-kappaB and AKT[J]. Cancer Cell 31(1):64–78
Momoi A, Nagai K, Isahai N et al (2016) Thymic extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue with 8q24 abnormality[J]. Intern Med 55(7):799–803
Xing W, Guanjun Z, Hongling W, Huan Z et al (2019) Clinicopathological features of primary thymic extranodal marginal zone B cell lymphomaof mucosa associated lymphoid tissue [J]. Chin Clin Oncol 48(4):315–317
Sugimoto KJ, Asahina M, Shimada A et al (2014) IgG3 subclass-positive primary thymic MALT lymphoma without trisomy 3 and trisomy 18: report of a case and review of literature[J]. Int J Clin Exp Pathol 7(12):8980–8987
You S, Sun JS, Park KJ et al (2020) Amyloid deposition in thymic extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue in a patient with myasthenia gravis: a case report[J]. Thoracic Cancer 11(3):781–784
Song W, Wang W, Zhou N (2011) Clinicopathological analysis of thymic mucosa-associated lymphoid tissue lymphoma[J]. Lin Chuang Zhong Liu Xue Za Zhi 16(9):829–832
Sun L, Shi H, Wei L (2012) Clinicopathologic features of primary thymic extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue type. Zhonghua Bing Li Xue Za Zhi 41(4):234–238
Wang Z, Li H, Cao Z et al (2016) Clinicopathologic study of primary thymic extranodal marginal zone lymphoma of mucosa associated lymphoid tissue and lymphoepithelial sialadenitis-like thymic hyperplasia[J]. J Clin Exp Pathol 32(12):1338–42
Shuai H, Li Z, Lang Z (2017) Two cases: mucosa-associated lymphoid tissue lymphoma of the thymus[J]. Shi Yong Fang She Xue Za Zhi 33(6):676–677
Chang X, Chen J, Jiang Y et al (2012) Mucosa-associated lymphoid tissue lymphoma of the thymus: a study of 2 cases[J]. Xie He Yi Xue Za Zhi 3(01):41–46
Xuejiao S, Wenwen S, Na Z et al (2018) Two eases of primary Sjogren’s syndrome complicated with thymus mucosa-associated lymphoid tissue lymphoma[J]. Chin J Gen Pract 17(11):936–937
Xu DM, Wang L, Zhu HY et al (2020) Primary thymic mucosa-associated lymphoid tissue lymphoma: 7 clinical cases report and a review of the literature[J]. Zhonghua Xue Ye Xue Za Zhi 41(1):54–8
Sunada K, Hasegawa Y, Kodama T et al (2007) Thymic and pulmonary mucosa-associated lymphoid tissue lymphomas in a patient with Sjogren’s syndrome and literature review[J]. Respirology 12(1):144–147
Kurabayashi A, Iguchi M, Matsumoto M et al (2010) Thymic mucosa-associated lymphoid tissue lymphoma with immunoglobulin-storing histiocytosis in Sjogren’s syndrome[J]. Pathol Int 60(2):125–130
Royer B, Cazals-Hatem D, Sibilia J et al (1997) Lymphomas in patients with Sjogren’s syndrome are marginal zone B-cell neoplasms, arise in diverse extranodal and nodal sites, and are not associated with viruses[J]. Blood 90(2):766–775
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the institutional review boards of the National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College (NCC3092).
Consent to participate
Informed consent was obtained from the patients for publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, X., Miao, Y., Cao, Z. et al. Characterization of molecular genetics and clinicopathology in thymic MALT lymphoma. Ann Hematol 101, 91–97 (2022). https://doi.org/10.1007/s00277-021-04671-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-021-04671-0