Abstract
Purpose
Although the middle temporal artery is used for maxillofacial and otological flap surgeries, the anatomical knowledge of the artery is insufficient to corroborate its usage. This study has investigated the interrelationship between the artery and the temporal fascia to enhance its availability.
Methods
The middle temporal artery was dissected in ten cadavers, and its spatial relations with the temporal fascia and muscle and the adjacent structures were examined.
Results
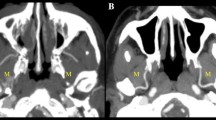
The middle temporal artery arose behind the mandibular head or neck and in front of the external acoustic meatus. It penetrated the temporal fascia external to the junction between the zygomatic process and the supramastoid crest. The artery gave off a thin branch in the space between the superficial and the deep layers of the fascia and is divided into two branches piercing the deep layer to supply the temporalis. The anterior branch anastomosed with the deep temporal artery; furthermore, it gave off the slender ramus coursing on the base of the zygomatic process to communicate with the masseteric artery. The posterior branch passed along the supramastoid crest, gave off a slender ramus and ascended in the groove of the temporal bone.
Conclusion
The branching pattern of the middle temporal artery and its positions relative to the temporal fascia and the landmark structures are helpful in identifying the artery, designing favourable flaps and avoiding unfavourable bleeding during surgery. They are also beneficial in developing the clinical usage of the artery.





Similar content being viewed by others
References
Bradley M, Patten AM (1953) The cardiovascular system. In: Schaeffer JP (ed) Morris’ human anatomy, 11th edn. The Blakiston Company, New York, pp 611–828
Standring S (2005) Head and Neck. In: Standring S, Ellis H, Healy JC, Johnson D, Williams A (eds) Gray’s anatomy, 39th edn. Elsevier Churchill Livingstone, London, pp 439–723
Thane GD (1894) Myology; angeiology. In: Schäfer EA, Thane GD (eds) Quain’s elements of anatomy, vol 2. Longman Green and Co, London, pp 199–350
Walles EW (1972) The blood vascular and lymphatic systems. In: Romanes GJ (ed) Cunningham’s textbook of anatomy, 11th edn. Oxford University Press, London, pp 837–967
Al-Kayat A, Bramley P (1979) A modified pre-auricular approach to the temporomandibular joint and malar arch. Br J Oral Surg 17:91–103
Mani V, Panda AK (2003) Versatility of temporalis myofascial flap in maxillofacial reconstruction—analysis of 30 cases. Int J Oral Maxillofac Surg 32:368–372
Black B, Kelly S (1994) Mastoidectomy reconstruction: revascularizing the canal wall repair. Am J Otol 15:91–95
Black B (1998) The use of vascular flaps in middle ear surgery. Am J Otol 19:420–427
Gluth MB, Sunde J (2013) Vascularized reconstruction of partial external auditory canal wall defects using the middle temporal artery flap. Otol Neurotol 35:e31–e35
O’ SullivanAtlas PGMD (2004) Use of soft tissue vascular flaps for mastoid cavity obliteration. Laryngoscope 114:957–959
Singh V, Atlas M (2007) Obliteration of the persistently discharging mastoid cavity using the middle temporal artery flap. Otolaryngol Head Neck Surg 137:433–438
Talmage GD, Sunde J, Walker DD, Atlas MD, Gluth MB (2016) Anatomic basis of the middle temporal artery periosteal rotational flap in otologic surgery. Laryngoscope 126:1426–1432
Rubio RR, Lawton MT, Kola O, Tabani H, Yousef S, Meybodi AT, Burkhardt JK, El-Sayed I, Benet A (2018) The middle temporal artery: surgical anatomy and exposure for cerebral revascularization. World Neurosurg 110:e79–e83
Daraei P, Mattox DE (2018) Landmarks for the preservation of the middle temporal artery during mastoid surgery: cadaveric dissection study. Am J Otolaryngol 39:6–9
Abul-Hassan HS, von Drasek AG, Acland RD (1986) Surgical anatomy and blood supplyof the facial layers of the temporal region. Plast Reconstr Surg 77:17–28
Beheiry EE, Abdel-Hamid FAM (2007) An anatomical study of the temporal fascia and related temporal pads of fat. Plast Reconstr Surg 119:136–144
Nakajima H, Imanishi N, Minabe T (1995) The arterial anatomy of the temporal region and the vascular basis of various temporal flaps. Br J Plast Surg 48:439–450
Cheung LK (1996) The blood supply of the human temporalis muscle: a vascular corrosion cast study. J Anat 189:431–438
Cheung LK (1996) The vascular anatomy of the human temporalis muscle: implications for surgical splitting techniques. Int J Oral Maxillofac Surg 25:414–421
Rusu MC, Jianu AM, Rădoi PM (2021) Anatomic variations of the superficial temporal artery. Surg Radiol Anat 43:445–450
Koziej M, Wnuk J, Polak J, Trybus M, Pękala P, Pękala J, Hołda M, Antoszewski B, Tomaszewski K (2020) The superficial temporal artery: a meta-analysis of its prevalence and morphology. Clin Anat 33:1130–1137
Qiu Y, Yang C, Chen M, Qiu W (2016) Can a novel surgical approach to the temporomandibular joint improve access and reduce complications? J Oral Maxillofac Surg 74:1336–1342
Kapoor KM, Bertossi D, Li CQ, Saputra DI, Heydenrych I, Yavuzer R (2020) A systematic literature review of the middle temporal vein anatomy: ‘venous danger zone’ in temporal fossa for filler injections. Aesthetic Plast Surg 44:1803–1810
Acknowledgements
The authors sincerely thank those who donated their bodies to science so that anatomical research could be performed. Results from such research can potentially increase mankind’s overall knowledge that can then improve patient care. Therefore, these donors and their families deserve our highest gratitude.
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
The author contributed to the study conception and design, this is completely the author’s own work, and the author approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The author has no conflicts of interest to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sakamoto, Y. The branching pattern of the middle temporal artery and the relation with the temporal fascia. Surg Radiol Anat 43, 1867–1874 (2021). https://doi.org/10.1007/s00276-021-02790-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-021-02790-x