Abstract
Purpose
Analyze the impact of endovascular revascularization on major amputation rates and wound healing for patients with diabetic foot ulcers (DFUs).
Materials and Methods
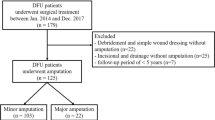
Single-center retrospective study from 2014–2018 including 314 patients with DFUs submitted to endovascular revascularizations. Group A—patients with a successful endovascular revascularization (n = 285; 90.8%); Group B—patients submitted to a failed attempt of endovascular revascularization (n = 29; 9.2%). Baseline data were not significantly different between the 2 groups (p > 0.05). Both groups were compared regarding: major amputation rates; wound healing, mortality and adverse events. Survival and regression analyses were used.
Results
Mean follow-up time was 734.1 ± 610.2 days. Major amputation rates were 3.9% versus 24.1% (p < 0.0001) and complete wound healing was 53.7% versus 20.7% (p < 0.0001) for patients from Group A versus Group B, respectively. Major adverse events were registered in 2 patients (one from each group); minor adverse events included 10 patients from Group A and 2 patients from Group B (p = 0.3654). Major amputation rates were: 3.9% versus 27.5% at 1 year; 4.6% versus 27.5% at 2–5 years for Group A versus Group B, respectively (p < 0.0001). Survival rates were: 87.8% at 1 year; 84.4% at 2 years; and 77.9% at 5 years with no significant differences between groups. Predictors for major amputation included failed revascularization (p < 0.0001), older age (p = 0.0394), prior stroke (0.0018), dialysis (0.0476). Predictors for mortality included older age (p < 0.0001) and coronary artery disease (p = 0.0388).
Conclusion
Endovascular revascularization for patients with DFUs is safe and has a significant impact on limb salvage and wound healing.



Similar content being viewed by others
References
Schaper NC, van Netten JJ, Apelqvist J, et al. Practical guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes Metab Res Rev. 2020 Mar;36(Suppl 1):e3266. https://doi.org/10.1002/dmrr.3266.
Hinchliffe R, et al. Effectiveness of revascularization of the ulcerated foot in patients with diabetes and peripheral artery disease: a systematic review. Diabetes Metab Res Rev. 2016;32(Suppl. 1):136–44.
Odink H, et al. Technical and clinical long-term results of infrapopliteal percutaneous transluminal angioplasty for critical limb ischemia. J Vasc Interv Radiol. 2012;23:461–7.
Peregrin J, et al. PTA of Infrapopliteal arteries: long-term clinical follow-up and analysis of factors influencing clinical outcome. Cardiovasc Intervent Radiol. 2010;33:720–5.
Hinchliffe RJ, Forsythe RO, Apelqvist J, et al. Guidelines on diagnosis, prognosis, and management of peripheral artery disease in patients with foot ulcers and diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020 Mar;36(Suppl 1):e3276. https://doi.org/10.1002/dmrr.3276.
Fossaceca R, et al. Endovascular treatment of diabetic foot in a selected population of patients with below-the-knee disease: is the angiosome model effective? Cardiovasc Intervent Radiol. 2013;36:637–44.
Wagner FW Jr. The dysvascular foot: a system for diagnosis and treatment. Foot Ankle. 1981;2:64–122.
Lavery LA, Armstrong DG, Murdoch DP, Peters EJ, Lipsky BA. Validation of the Infectious diseases society of America’s diabetic foot infection classification system. Clin Infect Dis. 2007;44:562–5.
Filippiadis DK, Binkert C, Pellerin O, Hoffmann RT, Krajina A, Pereira PL. Cirse quality assurance document and standards for classification of complications: the cirse classification system. Cardiovasc Intervent Radiol. 2017 Aug;40(8):1141–6.
Musuuza J, et al. A systematic review of multidisciplinary teams to reduce major amputations for patients with diabetic foot ulcers. J Vasc Surg. 2019. https://doi.org/10.1016/j.jvs.2019.08.244.
Mendes JJ, Neves J. Diabetic foot infections: current diagnosis and treatment. J Diabetic Foot Complic. 2012;4(2):26–45.
Lipsky BA, Berendt AR, Cormia PB, et al. 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2012;54(12):e132–e173173.
Highlander P, Shinabarger AB. Perioperative laboratory assessment of diabetic infections undergoing amputation: a systematic review. Foot Ankle Spec. 2013;6(6):465–70.
Schper NC, Andros G, Apelqvist J, et al. Specific guidelines for the diagnosis and treatment of peripheral arterial disease in a patient with diabetes and ulceration of the foot 2011. Diabetes Metab Res Rev. 2012;28(suppl 1):236–7.
Duarte B, Formiga A, Neves J. Dakin's solution in the treatment of severe diabetic foot infections. Int Wound J. 2019;17(2):277–84.
American Diabetes Association. Diabetes 1996 vital statistics. Alexandria, VA: American Diabetes Association; 1996.
Sen P, Demirdal T, Emir B. Meta-analysis of risk factors for amputation in diabetic foot infections. Diabetes Metab Res Rev. 2019;35(7):e3165. https://doi.org/10.1002/dmrr.3165.
Acknowledgements
These data were submitted as a manuscript and accepted for CIRSE 2020 in September.
Funding
No grants or funding were obtained for this specific manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Tiago Bilhim is a paid consultant for Merit Medical and has received speaker fees for Philips Medical, Cook Medical, Terumo and is a stock holder for EmbolX.
Nuno Vasco Costa is a paid consultant for Merit Medical.
Filipe Veloso Gomes is a paid consultant for Terumo.
Ethical Approval
Institutional review board approval was waived to perform this retrospective analysis.
Informed Consent
Informed Consent was obtained from all patients.
Consent for Publication
Consent for Publication was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Caetano, A.P., Conde Vasco, I., Veloso Gomes, F. et al. Successful Revascularization has a Significant Impact on Limb Salvage Rate and Wound Healing for Patients with Diabetic Foot Ulcers: Single-Centre Retrospective Analysis with a Multidisciplinary Approach. Cardiovasc Intervent Radiol 43, 1449–1459 (2020). https://doi.org/10.1007/s00270-020-02604-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-020-02604-4
Keywords
- Diabetic foot ulcers (DFUs)
- Diabetic foot disease
- Diabetic foot wounds
- Diabetic foot infections
- Ulceration of the foot
- Percutaneous transluminal angioplasty (PTA)
- Critical limb ischemia (CLI)
- Infrapopliteal arteries
- Infragenicular arteries
- Peripheral artery disease
- Below-the-knee disease
- Major amputation
- Limb salvage