Abstract
Background
Rhinoplasty, a leading cosmetic surgical procedure, often involves the use of opioids for postoperative pain management. This raises concerns due to potential opioid side effects and overprescription. Liposomal bupivacaine offers a promising alternative, but its efficacy in rhinoplasty remains under-investigated. This study assesses the impact of liposomal bupivacaine on postoperative pain and opioid consumption following rhinoplasty.
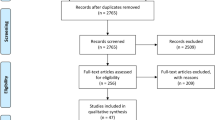
Methods
A retrospective study was conducted on patients undergoing rhinoplasty between January 2014 and September 2020. Postoperative pain scores were assessed at intervals up to 16 h, and opioid consumption was monitored. Patients were stratified into two groups: those receiving postoperative liposomal bupivacaine (Group 1) and those who did not (Group 2).
Results
No significant disparities in demographics or surgical specifics were identified between groups. Group 1 consistently reported lower pain scores, notably at 30 min (1.4 vs. 3.7, p = 0.0006) and 2 h (2.2 vs. 3.38, p = 0.0417). Cumulatively, Group 1’s average pain score was 2.4, significantly lower than Group 2’s 3.4 (p = 0.0023). Group 1 also demonstrated reduced opioid consumption, with oxycodone and oral morphine equivalent (OME) intake being notably lower (p = 0.005 and p = 0.0428, respectively).
Conclusion
Liposomal bupivacaine presents as an efficacious alternative for post-rhinoplasty pain management, reducing both perceived pain and opioid consumption. While promising, the findings necessitate validation through larger, prospective studies considering the inherent limitations of this preliminary investigation.
-
This study evaluates the efficacy of liposomal bupivacaine as a pain management strategy in postoperative care for rhinoplasty and septorhinoplasty procedures, with the potential to reduce reliance on opioids.
-
The findings indicate that patients receiving liposomal bupivacaine experienced significantly lower pain scores postoperatively and less overall opioid consumption, thereby enhancing patient comfort and safety.
Level of Evidence III
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.



Similar content being viewed by others
References
ASPS National Clearinghouse of Plastic Surgery Procedural Statistics (2020) Plastic surgery statistics report 2020
Gadkaree SK, Shaye DA, Occhiogrosso J, Lee LN (2019) Association between pain and patient satisfaction after rhinoplasty. JAMA Facial Plast Surg 21:475
Sclafani AP, Kim M, Kjaer K et al (2019) Postoperative pain and analgesic requirements after septoplasty and rhinoplasty. Laryngoscope 129:2020
Barinsky GL, Bresler AY, Paskhover B (2020) Liposomal bupivacaine in rhinoplasty: an underused tool. J Oral Maxillofac Surg 78:1239–1240
Dasta J, Ramamoorthy S, Patou G, Sinatra R (2012) Bupivacaine liposome injectable suspension compared with bupivacaine HCl for the reduction of opioid burden in the postsurgical setting. Curr Med Res Opin 28:1609–1615
Motakef S et al (2017) Liposomal bupivacaine in implant-based breast reconstruction. Plast Reconstr Surg Glob Open 5:1–7
Ilfeld BM, Malhotra N, Furnish TJ, Donohue MC, Madison SJ (2013) Liposomal bupivacaine as a single-injection peripheral nerve block: a dose-response study. Anesth Analg 117:1248–1256
Bergese SD et al (2012) Efficacy profile of liposome bupivacaine, a novel formulation of bupivacaine for postsurgical analgesia. J Pain Res 5:107–116
Vyas KS et al (2016) Systematic review of liposomal bupivacaine (exparel) for postoperative analgesia. Plast Reconstr Surg 138:748e–756e
Argoff CE (2020) Opioid-induced constipation: a review of health-related quality of life, patient burden, practical clinical considerations, and the impact of peripherally acting μ-opioid receptor antagonists. Clin J Pain 9:716–722
Sethi RKV, Lee LN, Quatela OE, Richburg KG, Shaye DA (2019) Opioid prescription patterns after rhinoplasty. JAMA Facial Plast Surg 21:76–77
Patel S, Sturm A, Bobian M (2018) Opioid use by patients after rhinoplasty. JAMA Facial Plast Surg 20:24–30
Manahan MA, Fedok F, Davidson C, Ahmad J, Constantinides M, Davis R, Friedman O, Gilman R, Ishii L, Keyes G, Lin SJ, Marcus B, Matarasso A, Most SP, Quereshy F, Sinno S, Steinbacher D, Tollefson T, Rohrich RJ (2021) Evidence-based performance measures for rhinoplasty: a multidisciplinary performance measure set. Plast Reconstr Surg 147:222e–230e
Alaniz L, Vu C, Arora J, Stulginski A, Zhu X, Cordero J, Vyas RM, Pfaff MJ (2023) Effective local anesthetic use in nasal surgery: a systematic review and meta-analysis of randomized controlled studies. Plast Reconstr Surg Glob Open 11(8):e5151
Collins JB, Song J, Mahabir RC (2013) Onset and duration of intradermal mixtures of bupivacaine and lidocaine with epinephrine. Can J Plast Surg 21:51–53
EXPAREL (bupivacaine liposome injectable suspension). [Online]. Available at https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/022496s9lbl.pdf. Accessed 28 Aug 2023
Acknowledgements
The authors declare that they have no conflict of interest to disclose. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments. For this type of study formal consent is not required.
Funding
The authors declare that they have no commercial interests in the subject of this study and have received no financial or material support relevant to this research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alameddine, K.O., Richards, B.A., Vyas, K. et al. Evaluating the Efficacy of Liposomal Bupivacaine in Postoperative Pain Management for Rhinoplasty: A Retrospective Study. Aesth Plast Surg 48, 1722–1727 (2024). https://doi.org/10.1007/s00266-023-03656-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-023-03656-w