Abstract
Background
Post-operative infection is a significant complication of breast implant surgery that may require extensive use of antibiotics and surgical interventions. Here, we developed a biomaterial coating that is chemically bonded to silicone implants which delivers antimicrobial ions over time.
Methods
After coating the silicone implants with a “mediator” polymer (γ-PGA), the implants were impregnated with silver (Ag) ions. Antimicrobial effects of these implants were assayed with modified Kirby-Bauer disk diffusion method. The silicone disks were transferred to a plate with fresh bacteria. Control was intended to simulate an intra-operative wash.
Results
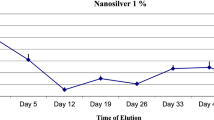
The Ag-γ-PGA coated silicone demonstrated antimicrobial effects against the most common etiological agents of breast implant infections, including Pseudomonas aeruginosa, Staphylococcus aureus, Staphylococcus epidermidis, Escherichia coli and Klebsiella pneumoniae. There was no effect of inhibition of bacterial growth around the control silicone or the silicone coated only with γ-PGA. The zone of inhibition was generally larger around the Ag-γ-PGA coated silicone as compared to the silicone irrigated with gentamicin, and continued antibacterial effect was also observed at 48 hours in the Ag-γ-PGA coated silicone for all bacteria groups with the exception of P. aeruginosa. Gentamicin-irrigated silicone did not inhibit bacterial growth at 48 hours.
Conclusion
The observed antibacterial performance of the Ag-γ-PGA coating as compared to simulated intra-operative antibiotic wash is promising and should be further evaluated to develop the next generation of implants with diminished risk for post-operative implant infections.





Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
DellaCroce FJ, Wolfe ET (2013) Breast reconstruction. Surg Clin North Am 93:445–454. https://doi.org/10.1016/j.suc.2012.12.004
Gardani M, Bertozzi N, Grieco MP et al (2017) Breast reconstruction with anatomical implants: a review of indications and techniques based on current literature. Ann Med Surg 21:96–104. https://doi.org/10.1016/j.amsu.2017.07.047
Albornoz CR, Bach PB, Mehrara BJ et al (2013) A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg 131:15–23. https://doi.org/10.1097/PRS.0b013e3182729cde
American Society of Plastics Surgeons (2020) Plastic surgery statistics report. Am Soc Plast Surg 1–23
Champaneria MC, Wong WW, Hill ME, Gupta SC (2012) The evolution of breast reconstruction: a historical perspective. World J Surg 36:730–742. https://doi.org/10.1007/s00268-012-1450-2
Seng P, Bayle S, Alliez A et al (2015) The microbial epidemiology of breast implant infections in a regional referral centre for plastic and reconstructive surgery in the south of France. Int J Infect Dis 35:e62–e66. https://doi.org/10.1016/j.ijid.2015.04.010
Aladily TN, Nathwani BN, Miranda RN et al (2012) Extranodal NK/T-cell lymphoma, nasal type, arising in association with saline breast implant: expanding the spectrum of breast implant-associated lymphomas. Am J Surg Pathol 36:1729–1734. https://doi.org/10.1097/PAS.0b013e31826a006f
Clemens MW, Horwitz SM (2017) NCCN Consensus guidelines for the diagnosis and management of breast implant-associated anaplastic large cell lymphoma. Aesthetic Surg J 37:285–289. https://doi.org/10.1093/asj/sjw259
Hall-Findlay EJ (2011) Breast implant complication review: double capsules and late seromas. Plast Reconstr Surg 127:56–66. https://doi.org/10.1097/PRS.0b013e3181fad34d
Collett DJ, Rakhorst H, Lennox P et al (2019) Current risk estimate of breast implant-associated anaplastic large cell lymphoma in textured breast implants. Plast Reconstr Surg 143:30S-40S. https://doi.org/10.1097/PRS.0000000000005567
Leberfinger AN, Behar BJ, Williams NC et al (2017) Breast implant-associated anaplastic large cell lymphoma: a systematic review. JAMA Surg 152:1161–1168. https://doi.org/10.1001/jamasurg.2017.4026
Bizjak M, Selmi C, Praprotnik S et al (2015) Silicone implants and lymphoma: the role of inflammation. J Autoimmun 65:64–73. https://doi.org/10.1016/j.jaut.2015.08.009
Samargandi OA, Joukhadar N, Al Youha S et al (2018) Antibiotic irrigation of pocket for implant-based breast augmentation to prevent capsular contracture: a systematic review. Plast Surg 26:110–119. https://doi.org/10.1177/2292550317747854
Baghaki S, Soybir GR, Soran A (2014) Guideline for antimicrobial prophylaxis in breast surgery. J Breast Heal 10:79–82. https://doi.org/10.5152/tjbh.2014.1959
Bachour Y, Verweij SP, Gibbs S et al (2018) The aetiopathogenesis of capsular contracture: a systematic review of the literature. J Plast Reconstr Aesthetic Surg 71:307–317. https://doi.org/10.1016/j.bjps.2017.12.002
Cunningham B, McCue J (2009) Safety and effectiveness of Mentor’s MemoryGel implants at 6 years. Aesthetic Plast Surg 33:440–444. https://doi.org/10.1007/s00266-009-9364-6
O’Shaughnessy K (2015) Evolution and update on current devices for prosthetic breast reconstruction. Gland Surg 4:97–110. https://doi.org/10.3978/j.issn.2227-684X.2015.03.09
DeFife KM, Shive MS, Hagen KM et al (1999) Effects of photochemically immobilized polymer coatings on protein adsorption, cell adhesion, and the foreign body reaction to silicone rubber. J Biomed Mater Res 44:298–307. https://doi.org/10.1002/(sici)1097-4636(19990305)44:3%3c298::aid-jbm8%3e3.0.co;2-n
Shin BH, Kim BH, Kim S et al (2018) Silicone breast implant modification review: overcoming capsular contracture. Biomater Res 22:37. https://doi.org/10.1186/s40824-018-0147-5
Park JU, Ham J, Kim S et al (2014) Alleviation of capsular formations on silicone implants in rats using biomembrane-mimicking coatings. Acta Biomater 10:4217–4225. https://doi.org/10.1016/j.actbio.2014.07.007
Oliveira WF, Silva PMS, Silva RCS et al (2018) Staphylococcus aureus and Staphylococcus epidermidis infections on implants. J Hosp Infect 98:111–117. https://doi.org/10.1016/j.jhin.2017.11.008
Mandakhalikar KD, Wang R, Rahmat JN et al (2018) Restriction of in vivo infection by antifouling coating on urinary catheter with controllable and sustained silver release: a proof of concept study. BMC Infect Dis 18:370. https://doi.org/10.1186/s12879-018-3296-1
Ogunleye A, Bhat A, Irorere VU et al (2015) Poly-γ-glutamic acid: production, properties and applications. Microbiology 161:1–17. https://doi.org/10.1099/mic.0.081448-0
Bauer AW, Kirby WM, Sherris JC, Turck M (1966) Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol 45:493–496
Makamba H, Kim JH, Lim K et al (2003) Surface modification of poly(dimethylsiloxane) microchannels. Electrophoresis 24:3607–3619. https://doi.org/10.1002/elps.200305627
Gonzales D, Fan K, Sevoian M (1996) Synthesis and swelling characterizations of a poly gamma-glutamic acid hydrogel. J Polym Sci Part A Polym Chem 34(10):2019–2027. https://doi.org/10.1002/(SICI)1099-0518(19960730)34:10%3c2019::AID-POLA19%3e3.0.CO;2-K
Saini H, Vadekeetil A, Chhibber S, Harjai K (2017) Azithromycin-ciprofloxacin-impregnated urinary catheters avert bacterial colonization, biofilm formation, and inflammation in a murine model of foreign-body-associated urinary tract infections caused by pseudomonas aeruginosa. Antimicrob Agents Chemother 61:e01906-e1916. https://doi.org/10.1128/AAC.01906-16
Hidalgo DA, Sinno S (2016) Current trends and controversies in breast augmentation. Plast Reconstr Surg 137:1142–1150. https://doi.org/10.1097/01.prs.0000481110.31939.e4
van Vugt TAG, Arts JJ, Geurts JAP (2019) Antibiotic-loaded polymethylmethacrylate beads and spacers in treatment of orthopedic infections and the role of biofilm formation. Front Microbiol 10:1626. https://doi.org/10.3389/fmicb.2019.01626
Kuehl R, Brunetto PS, Woischnig AK et al (2016) Preventing Implant-associated infections by silver coating. Antimicrob Agents Chemother 60:2467–2475. https://doi.org/10.1128/AAC.02934-15
Dhiman NK, Agnihotri S, Shukla R (2019) Silver-based polymeric nanocomposites as antimicrobial coatings for biomedical applications bt - nanotechnology in modern animal biotechnology: recent trends and future perspectives. In: Maurya PK (ed) Singh S. Springer Singapore, Singapore, pp 115–171
Ooi AS, Song DH (2016) Reducing infection risk in implant-based breast-reconstruction surgery: challenges and solutions. Breast cancer Dove Med Press 8:161–172. https://doi.org/10.2147/BCTT.S97764
Donlan RM (2000) Role of biofilms in antimicrobial resistance. ASAIO J 46:S47-52. https://doi.org/10.1097/00002480-200011000-00037
Deva AK, Adams WPJ, Vickery K (2013) The role of bacterial biofilms in device-associated infection. Plast Reconstr Surg 132(5):1319–1328. https://doi.org/10.1097/PRS.0b013e3182a3c105
Ahn CY, Ko CY, Wagar EA et al (1996) Microbial evaluation: 139 implants removed from symptomatic patients. Plast Reconstr Surg 98:1225–1229. https://doi.org/10.1097/00006534-199612000-00016
Macadam SA, Mehling BM, Fanning A et al (2007) Nontuberculous mycobacterial breast implant infections. Plast Reconstr Surg 119:337–344. https://doi.org/10.1097/01.prs.0000244924.61968.d2
Cain DW, Cidlowski JA (2017) Immune regulation by glucocorticoids. Nat Rev Immunol 17:233–247. https://doi.org/10.1038/nri.2017.1
Peters-Golden M, Henderson WRJ (2007) Leukotrienes. N Engl J Med 357:1841–1854. https://doi.org/10.1056/NEJMra071371
Zeplin PH, Larena-Avellaneda A, Schmidt K (2010) Surface modification of silicone breast implants by binding the antifibrotic drug halofuginone reduces capsular fibrosis. Plast Reconstr Surg 126:266–274. https://doi.org/10.1097/PRS.0b013e3181dbc313
Walker JN, Hanson BM, Pinkner CL et al (2019) Insights into the microbiome of breast implants and periprosthetic tissue in breast implant-associated anaplastic large cell lymphoma. Sci Rep 9:10393. https://doi.org/10.1038/s41598-019-46535-8
Risks E (2020) Preliminary opinion on the safety of breast implants in relation to anaplastic large cell lymphoma. 1–43
Clemens MW (2021) Breast Implant-Associated Anaplastic Large Cell Lymphoma: Origin and Outcome. 77–87. https://doi.org/10.1007/978-3-030-57121-4
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest statement
The authors declare that they have no conflicts of interest to disclose.
Statement of Human and Animal Rights, or Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Heno, F., Azoulay, Z., Khalfin, B. et al. Comparing the Antimicrobial Effect of Silver Ion-Coated Silicone and Gentamicin-Irrigated Silicone Sheets from Breast Implant Material. Aesth Plast Surg 45, 2980–2989 (2021). https://doi.org/10.1007/s00266-021-02348-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-021-02348-7