Abstract
Purpose
To assess the diagnostic performance of quantitative and qualitative imaging features of hepatic cirrhosis on CT.
Methods
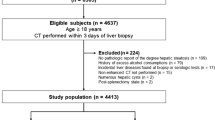
A single-center retrospective cohort study was performed on all patients who had undergone non-targeted liver biopsy < 3 months following abdominal CT imaging between 2007 and 2020. Histopathology was required as a reference standard for hepatic cirrhosis diagnosis. Two readers independently assessed all CT quantitative and qualitative features, blinded to the clinical history and the reference standard. The diagnostic performance of each imaging feature was assessed using multivariate regression and logistic regression in a recursive feature elimination framework.
Results
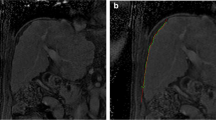
98 consecutive patients met inclusion criteria including 26 with histopathologically confirmed hepatic cirrhosis, and 72 without cirrhosis. Liver surface nodularity (p < 0.0001), lobar redistribution (p < 0.0001), and expanded gallbladder fossa (p < 0.0016) were qualitative CT features associated with liver cirrhosis consistent between both reviewers. Liver surface nodularity demonstrated highest sensitivity (73–77%) and specificity (79–82%). Falciform space width was the only quantitative feature associated with cirrhosis, for a single reviewer (p < 0.04). Using a recursive feature elimination framework, liver surface nodularity and falciform space width were the strongest performing features for identifying cirrhosis. No feature combinations strengthened diagnostic performance.
Conclusion
Many quantitative and qualitative CT imaging signs of hepatic cirrhosis have either poor accuracy or poor inter-observer agreement. Qualitative imaging features of hepatic cirrhosis on CT performed better than quantitative metrics, with liver surface nodularity the most optimal feature for diagnosing hepatic cirrhosis.
Graphical abstract








Similar content being viewed by others
References
Garcia-Tsao G, Friedman S, Iredale J, Pinzani M. Now there are many (stages) where before there was one: In search of a pathophysiological classification of cirrhosis. Hepatology. 2010;51(4):1445–9. https://doi.org/https://doi.org/10.1002/hep.23478
Tsochatzis EA, Bosch J, Burroughs AK. Liver cirrhosis. Lancet. 2014;383(9930):1749–61. https://doi.org/https://doi.org/10.1016/S0140-6736(14)60121-5
Statistics Canada. Table 13-10-0801-01. Leading ca uses of death, total population (age standardization using 2011 population). https://doi.org/10.25318/1310080101-eng
Heron M. National Vital Statistics Reports Deaths: leading causes for 2017. Natl Vital Stat Rep. 2019;68(6):1–77.
Flemming JA, Djerboua M, Booth CM TN. Increasing burden of cirrhosis projected to 2040 in Canada: implications for prevention, screening, and management. Int Liver Congr. 2020;73:S45.
Best AF, Haozous EA, de Gonzalez AB, Chernyavskiy P, Freedman ND, Hartge P, et al. Premature mortality projections in the USA through 2030: a modelling study. Lancet Public Health. 2018;3(8):e374–84. https://doi.org/https://doi.org/10.1016/S2468-2667(18)30114-2
Ravaioli F, Colecchia A, Alemanni LV, Vestito A, Dajti E, Marasco G, et al. Role of imaging techniques in liver veno-occlusive disease diagnosis: recent advances and literature review. Expert Rev Gastroenterol Hepatol. 2019;13(5):463–84. https://doi.org/https://doi.org/10.1080/17474124.2019.1588111
Iqbal U, Perumpail B, Akhtar D, Kim D, Ahmed A. The Epidemiology, Risk Profiling and Diagnostic Challenges of Nonalcoholic Fatty Liver Disease. Medicines. 2019;6(1):41. https://doi.org/https://doi.org/10.3390/medicines6010041
Myers RP, Fong A, Shaheen AAM. Utilization rates, complications and costs of percutaneous liver biopsy: A population-based study including 4275 biopsies. Liver Int. 2008;28(5):705–12. https://doi.org/https://doi.org/10.1111/j.1478-3231.2008.01691.x
Perrault J, McGill DB, Ott BJ, Taylor WF. Liver biopsy: Complications in 1000 inpatients and outpatients. Gastroenterology. 1978;74(1):103–6. https://doi.org/https://doi.org/10.1016/0016-5085(78)90364-5
Kamphuisen PW, Wiersma TG, Mulder CJJ, De Vries RA. Plugged-percutaneous liver biopsy in patients with impaired coagulation and ascites. Pathophysiol Haemost Thromb. 2002;32(4):190–3. https://doi.org/https://doi.org/10.1159/000070426
Horvath B, Allende D, Xie H, Guirguis J, Jeung J, Lapinski J, et al. Interobserver Variability in Scoring Liver Biopsies with a Diagnosis of Alcoholic Hepatitis. Alcohol Clin Exp Res. 2017;41(9):1568–73. https://doi.org/https://doi.org/10.1111/acer.13438
Vuppalanchi R, Ünalp A, Van Natta ML, Cummings OW, Sandrasegaran KE, Hameed T, et al. Effects of Liver Biopsy Sample Length and Number of Readings on Sampling Variability in Nonalcoholic Fatty Liver Disease. Clin Gastroenterol Hepatol. 2009;7(4):481–6. https://doi.org/https://doi.org/10.1016/j.cgh.2008.12.015
Carey E, Carey WD. Noninvasive tests for liver disease, fibrosis, and cirrhosis: Is liver biopsy obsolete? Cleve Clin J Med. 2010;77(8):519–27. https://doi.org/https://doi.org/10.3949/ccjm.77a.09138
Tang A, Cloutier G, Szeverenyi NM, Sirlin CB. Ultrasound elastography and MR elastography for assessing liver fibrosis: Part 1, principles and techniques. Am J Roentgenol. 2015;205(1):22–32. https://doi.org/https://doi.org/10.2214/AJR.15.14552
Bertot LC, Jeffrey GP, Wallace M, MacQuillan G, Garas G, Ching HL, et al. Nonalcoholic fatty liver disease-related cirrhosis is commonly unrecognized and associated with hepatocellular carcinoma. Hepatol Commun. 2017;1(1):53–60. https://doi.org/https://doi.org/10.1002/hep4.1018
Axley P, Mudumbi S, Sarker S, Kuo YF, Singal AK. Patients with stage 3 compared to stage 4 liver fibrosis have lower frequency of and longer time to liver disease complications. PLoS One. 2018;13(8):1–11. https://doi.org/https://doi.org/10.1371/journal.pone.0197117
Harbin P, Robert J, Ferrucci T. Diagnosis of cirrhosis based on regional changes in hepatic morphology. Radiology. 1980;135:273–83. https://doi.org/https://doi.org/10.1148/radiology.135.2.7367613
Ito K, Mitchell DG, Kim MJ, Awaya H, Koike S, Matsunaga N. Right Posterior Hepatic Notch Sign: A Simple Diagnostic MR Finding of Cirrhosis. J Magn Reson Imaging. 2003;18(5):561–6. https://doi.org/https://doi.org/10.1002/jmri.10387
Lafortune M, Matricardi L, Denys A, Favret M, Déry R, Pomier-Layrargues G. Segment 4 (the quadrate lobe): A barometer of cirrhotic liver disease at US. Radiology. 1998;206(1):157–60. https://doi.org/https://doi.org/10.1148/radiology.206.1.9423666
Awaya H, Mitchell DG, Kamishima T, Holland G, Ito K, Matsumoto T. Cirrhosis: Modified caudate-right lobe ratio. Radiology. 2002;224(3):769–74. https://doi.org/https://doi.org/10.1148/radiol.2243011495
Kok CT. Enlargement of the hilar periportal space. Radiology. 2008;248(2):699–700. https://doi.org/https://doi.org/10.1148/radiol.2482060463
Yoshikawa J, Matsui O, Takashima T, Sugiura H, Katayama K, Nishida Y, et al. Focal fatty change of the liver adjacent to the falciform ligament: CT and sonographic findings in five surgically confirmed cases. Am J Roentgenol. 1987;149(3):491–4. https://doi.org/https://doi.org/10.2214/ajr.149.3.491
Bolondi L, Gandolfi L, Arienti V, Caletti GC, Corcioni E, Gasbarrini G, et al. Ultrasonography in the diagnosis of portal hypertension: Diminished response of portal vessels to respiration. Radiology. 1982;142(1):167–72. https://doi.org/https://doi.org/10.1148/radiology.142.1.7053528
Kok CT. The right posterior hepatic notch sign. Radiology. 2008;248(1):317–8. https://doi.org/https://doi.org/10.1148/radiol.2481051024
Li S, Sun X, Chen M, Ying Z, Wan Y, Pi L, et al. Liver Fibrosis Conventional and Molecular Imaging Diagnosis Update. J Liver. 2019;08(01):1–21.
Landis JR, Koch GG. The Measurement of Observer Agreement for Categorical Data. Biometrics. 1977;33(1):159. https://doi.org/https://doi.org/10.2307/2529310
Kudo M, Zheng RQ, Kim SR, Okabe Y, Osaki Y, Iijima H, et al. Diagnostic accuracy of imaging for liver cirrhosis compared to histologically proven liver cirrhosis. Intervirology. 2008;51:17–26. https://doi.org/https://doi.org/10.1159/000122595
Yeom SK, Lee CH, Cha SH, Park CM. Prediction of liver cirrhosis, using diagnostic imaging tools. World J Hepatol. 2015;7(17):2069–79. https://doi.org/https://doi.org/10.4254/wjh.v7.i17.2069
Elkassem AA, Allen BC, Lirette ST, Cox KL, Remer EM, Pickhardt PJ, et al. Multiinstitutional Evaluation of the Liver Surface Nodularity Score on CT for Staging Liver Fibrosis and Predicting Liver-Related Events in Patients with Hepatitis C. Am J Roentgenol. 2021; https://doi.org/https://doi.org/10.2214/AJR.21.27062
Sterling RK, Lissen E, Clumeck N, Sola R, Correa MC, Montaner J, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43(6):1317–25. https://doi.org/https://doi.org/10.1002/hep.21178
Smith AD, Branch CR, Zand K, Subramony C, Zhang H, Thaggard K, et al. Liver surface nodularity quantification from routine ct images as a biomarker for detection and evaluation of cirrhosis. Radiology. 2016;280(3):771–81. https://doi.org/https://doi.org/10.1148/radiol.2016151542
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rubino, J.G., Nasirzadeh, A.R., van der Pol, C.B. et al. Quantitative and qualitative liver CT: imaging feature association with histopathologically confirmed hepatic cirrhosis. Abdom Radiol 47, 2314–2324 (2022). https://doi.org/10.1007/s00261-022-03550-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-022-03550-0