Abstract
Purpose
Diagnosis of lymph node metastasis (LNM) is critical for patients with pancreatic ductal adenocarcinoma (PDAC). We aimed to build deep learning radiomics (DLR) models of dual-energy computed tomography (DECT) to classify LNM status of PDAC and to stratify the overall survival before treatment.
Methods
From August 2016 to October 2020, 148 PDAC patients underwent regional lymph node dissection and scanned preoperatively DECT were enrolled. The virtual monoenergetic image at 40 keV was reconstructed from 100 and 150 keV of DECT. By setting January 1, 2021, as the cut-off date, 113 patients were assigned into the primary set, and 35 were in the test set. DLR models using VMI 40 keV, 100 keV, 150 keV, and 100 + 150 keV images were developed and compared. The best model was integrated with key clinical features selected by multivariate Cox regression analysis to achieve the most accurate prediction.
Results
DLR based on 100 + 150 keV DECT yields the best performance in predicting LNM status with the AUC of 0.87 (95% confidence interval [CI]: 0.85–0.89) in the test cohort. After integrating key clinical features (CT-reported T stage, LN status, glutamyl transpeptadase, and glucose), the AUC was improved to 0.92 (95% CI: 0.91–0.94). Patients at high risk of LNM portended significantly worse overall survival than those at low risk after surgery (P = 0.012).
Conclusions
The DLR model showed outstanding performance for predicting LNM in PADC and hold promise of improving clinical decision-making.



Similar content being viewed by others
Code availability
The code of this study is publicly accessible at http://www.radiomics.net.cn/owncloud/index.php/s/7DQTr9qLiFbEJup.
References
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74:2913–21.
Brown ZJ, Cloyd JM. Surgery for pancreatic cancer: recent progress and future directions. Hepatobiliary Surg Nutr. 2021;10:376–8.
Durán H, Olivares S, Ielpo B, et al. Prognostic value of lymph node status for actual long-term survival in resected pancreatic cancer. Surg Technol Int. 2020;37:79–84.
Potjer TP. Pancreatic cancer surveillance and its ongoing challenges: is it time to refine our eligibility criteria? Gut. 2021 Jun 18:gutjnl-2021-324739. https://doi.org/10.1136/gutjnl-2021-324739
Perlmutter BC, Hossain MS, Naples R, et al. Survival impact based on hepatic artery lymph node status in pancreatic adenocarcinoma: a study of patients receiving modern chemotherapy. J Surg Oncol. 2021;123:399–406.
Takahashi H, Ohigashi H, Ishikawa O, et al. Perineural invasion and lymph node involvement as indicators of surgical outcome and pattern of recurrence in the setting of preoperative gemcitabine-based chemoradiation therapy for resectable pancreatic cancer. Ann Surg. 2012;255:95–102.
Masuda T, Dann AM, Elliott IA, et al. A comprehensive assessment of accurate lymph node staging and preoperative detection in resected pancreatic cancer. J Gastrointest Surg. 2018;22:295–302.
Kumon RE, Repaka A, Atkinson M, et al. Lymph node characterization in vivo using endoscopic ultrasound spectrum analysis with electronic array echo endoscopes. Endoscopy. 2012;44:618–21.
Nanashima A, Sakamoto I, Hayashi T, et al. Preoperative diagnosis of lymph node metastasis in biliary and pancreatic carcinomas: evaluation of the combination of multi-detector CT and serum CA19-9 level. Dig Dis Sci. 2010;55:3617–26.
Zhang Z, Procissi D, Li W, et al. High resolution MRI for non-invasive mouse lymph node mapping. J Immunol Methods. 2013;400–401:23–9.
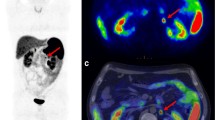
Wang S, Shi H, Yang F, Teng X, Jiang B. The value of 18F-FDG PET/CT and carbohydrate antigen 19–9 in predicting lymph node micrometastases of pancreatic cancer. Abdom Radiol (NY). 2019;44:4057–62.
Masui T, Sato A, Nakano K, et al. Predictive value of the Ki67 index for lymph node metastasis of small non-functioning pancreatic neuroendocrine neoplasms. Surg Today. 2019;49:593–600.
Xiang ZJ, Hu T, Wang Y, Wang H, Xu L, Cui N. Neutrophil-lymphocyte ratio (NLR) was associated with prognosis and immunomodulatory in patients with pancreatic ductal adenocarcinoma (PDAC). Biosci Rep. 2020 Jun 26;40(6):BSR20201190.https://doi.org/10.1042/BSR20201190
Wang SC, Parekh JR, Porembka MR, et al. A pilot study evaluating serum MMP7 as a preoperative prognostic marker for pancreatic ductal adenocarcinoma patients. J Gastrointest Surg. 2016;20:899–904.
Andrianifahanana M, Moniaux N, Schmied BM, et al. Mucin (MUC) gene expression in human pancreatic adenocarcinoma and chronic pancreatitis: a potential role of MUC4 as a tumor marker of diagnostic significance. Clin Cancer Res. 2001;7:4033–40.
Nishiwada S, Sho M, Banwait JK, et al. A microRNA signature identifies pancreatic ductal adenocarcinoma patients at risk for lymph node metastases. Gastroenterology. 2020;159:562–74.
Dong D, Fang MJ, Tang L, et al. Deep learning radiomic nomogram can predict the number of lymph node metastasis in locally advanced gastric cancer: an international multicenter study. Ann Oncol. 2020;31:912–20.
Huang YQ, Liang CH, He L, et al. Development and validation of a radiomics nomogram for preoperative prediction of lymph node metastasis in colorectal cancer. J Clin Oncol. 2016;34:2157–64.
Li Q, Fan X, Luo TY, Lv FJ, Huang XT. Differentiating malignant and benign necrotic lung lesions using kVp-switching dual-energy spectral computed tomography. BMC Med Imaging. 2021;21:81.
Wang X, Liu D, Zeng X, et al. Dual-energy CT quantitative parameters for the differentiation of benign from malignant lesions and the prediction of histopathological and molecular subtypes in breast cancer. Quant Imaging Med Surg. 2021;11:1946–57.
Morgan DE. The role of dual-energy computed tomography in assessment of abdominal oncology and beyond. Radiol Clin North Am. 2018;56:565–85.
Nair JR, DeBlois F, Ong T, et al. Dual-energy CT: balance between iodine attenuation and artifact reduction for the evaluation of head and neck cancer. J Comput Assist Tomogr. 2017;41:931–6.
Kim J-E, Nam N-E, Shim J-S, Jung Y-H, Cho B-H, Hwang JJ. Transfer learning via deep neural networks for implant fixture system classification using periapical radiographs. J Clin Med. 2020;9(4):1117. https://doi.org/10.3390/jcm9041117.
Russakovsky O, Deng J, Su H, et al. Imagenet large scale visual recognition challenge[J]. International journal of computer vision, 2015, 115(3): 211–52. https://doi.org/10.1007/s11263-015-0816-y
Zhang Z, Mo L, Huang C, Xu P, written on behalf of AME Big-Data Clinical Trial Collaborative Group. Binary logistic regression modeling with TensorFlowTM. Ann Transl Med. 2019;7:591.
Gutiérrez M. Data, data flows, and model specifications for linking multi-level contribution margin accounting with multi-level fixed-charge problems. Data Brief. 2021;35:106931.
Liu Z, Li Z, Qu J, et al. Radiomics of multiparametric MRI for pretreatment prediction of pathologic complete response to neoadjuvant chemotherapy in breast cancer: a multicenter study. Clin Cancer Res. 2019;25:3538–47.
Beer L, Toepker M, Ba-Ssalamah A, et al. Objective and subjective comparison of virtual monoenergetic vs. polychromatic images in patients with pancreatic ductal adenocarcinoma. Eur Radiol. 2019;29:3617–25.
Xu D, Wang J, Liu T, et al. Quantitative definitions of pain, CA19-9, and tumor size as high-risk features of resectable pancreatic cancer: a single-center retrospective cohort study. Gland Surg. 2021;10:770–9.
Tanaka M, Heckler M, Mihaljevic AL, et al. Systematic review and metaanalysis of lymph node metastases of resected pancreatic neuroendocrine tumors. Ann Surg Oncol. 2021;28:1614–24.
Cui Y, Wu J, Zong M, et al. Proteomic profiling in pancreatic cancer with and without lymph node metastasis. Int J Cancer. 2009;124:1614–21.
Zou Y, Zheng M, Qi Z, et al. Dual-energy computed tomography could reliably differentiate metastatic from non-metastatic lymph nodes of less than 0.5 cm in patients with papillary thyroid carcinoma. Quant Imaging Med Surg. 2021;11:1354–67.
Li J, Dong D, Fang M, et al. Dual-energy CT-based deep learning radiomics can improve lymph node metastasis risk prediction for gastric cancer. Eur Radiol. 2020;30:2324–33.
Forghani R, Chatterjee A, Reinhold C, et al. Head and neck squamous cell carcinoma: prediction of cervical lymph node metastasis by dual-energy CT texture analysis with machine learning. Eur Radiol. 2019;29:6172–81.
Tawfik AM, Razek AA, Kerl JM, Nour-Eldin NE, Bauer R, Vogl TJ. Comparison of dual-energy CT-derived iodine content and iodine overlay of normal, inflammatory and metastatic squamous cell carcinoma cervical lymph nodes. Eur Radiol. 2014;24:574–80.
Zhang X, Zheng C, Yang Z, et al. Axillary sentinel lymph nodes in breast cancer: quantitative evaluation at dual-energy CT. Radiology. 2018;289:337–46.
Li K, Yao Q, Xiao J, et al. Contrast-enhanced CT radiomics for predicting lymph node metastasis in pancreatic ductal adenocarcinoma: a pilot study. Cancer Imaging. 2020;20:12.
Bian Y, Guo S, Jiang H, et al. Relationship between radiomics and risk of lymph node metastasis in pancreatic ductal adenocarcinoma. Pancreas. 2019;48:1195–203.
Gao J, Han F, Jin Y, Wang X, Zhang J. A radiomics nomogram for the preoperative prediction of lymph node metastasis in pancreatic ductal adenocarcinoma. Front Oncol. 2020;10:1654.
Xie T, Wang X, Li M, Tong T, Yu X, Zhou Z. Pancreatic ductal adenocarcinoma: a radiomics nomogram outperforms clinical model and TNM staging for survival estimation after curative resection. Eur Radiol. 2020;30:2513–24.
Sala E, Ursprung S. Artificial intelligence in radiology: the computer’s helping hand needs guidance. Radiol Artif Intell. 2020;2:e200207.
Philbrick KA, Yoshida K, Inoue D, et al. What does deep learning see? Insights from a classifier trained to predict contrast enhancement phase from CT images. AJR Am J Roentgenol. 2018;211:1184–93.
Panwar H, Gupta PK, Siddiqui MK, Morales-Menendez R, Bhardwaj P, Singh V. A deep learning and grad-CAM based color visualization approach for fast detection of COVID-19 cases using chest X-ray and CT-scan images. Chaos Solitons Fractals. 2020;140:110190.
Takahashi H, Akita H, Tomokuni A, et al. Preoperative gemcitabine-based chemoradiation therapy for borderline resectable pancreatic cancer: impact of venous and arterial involvement status on surgical outcome and pattern of recurrence. Ann Surg. 2016;264:1091–7.
Ravikumar R, Fusai G. Preoperative gemcitabine-based chemoradiation therapy for resectable and borderline resectable pancreatic cancer. Ann Surg. 2015;262:e103.
Takahashi H, Ohigashi H, Gotoh K, et al. Preoperative gemcitabine-based chemoradiation therapy for resectable and borderline resectable pancreatic cancer. Ann Surg. 2013;258:1040–50.
Acknowledgements
The authors would like to acknowledge the instrumental and technical support of Multimodal Biomedical Imaging Experimental Platform, Institute of Automation, Chinese Academy of Sciences.
Funding
This study was funded by Ministry of Science and Technology of China under Grant No. 2017YFA0205200, National Natural Science Foundation of China under Grant Nos. 62027901, 81227901, and 81930053, the Youth Innovation Promotion Association CAS under Grant No. Y202040, and the Project of High-Level Talents Team Introduction in Zhuhai City (Zhuhai HLHPTP201703). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Conception and design: Chao An, Kun Wang, Suiqing Zhuo, J. Tian; development of methodology: Kun Wang; acquisition of data (provided animals, acquired and managed patients, provided facilities, etc.): Chao An, Sheng Li, Lizhi Liu, Dongping Jiang, Suiqing Zhuo, Ning Hai, Linling Jiang, Guangying Ruan; analysis and interpretation of data (e.g., statistical analysis, biostatistics, and computational analysis): Chao An, Dongyang Li, Wangzhong Li, Tong Tong, Kun Wang, J. Tian; writing, review, and/or revision of the manuscript: Chao An, Dongyang Li, Kun Wang, Yan Fu, J. Tian; administrative, technical, or material support (i.e., reporting or organizing data and constructing databases): J. Tian; study supervision: Kun Wang, Suiqing Zhuo.
Corresponding authors
Ethics declarations
Ethics approval
This retrospective study was approved by the Institutional Review Board of Sun Yat-sen University Cancer Center (B2019-012–01) and was conducted following the principles of the Declaration of Helsinki. The requirement for written informed consent was waived because of the retrospective nature of the study. The key raw data of this study were uploaded to the Research Data Deposit database (www.researchdata.org.cn. RDD2021002019).
Consent to participate
Yes.
Consent to publication
Yes.
Conflict of interest
The authors declare no competing interests.
Open access
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creative.commonsh.org/licenses/by/4.0/.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Advanced Image Analyses (Radiomics and Artificial Intelligence)
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
An, C., Li, D., Li, S. et al. Deep learning radiomics of dual-energy computed tomography for predicting lymph node metastases of pancreatic ductal adenocarcinoma. Eur J Nucl Med Mol Imaging 49, 1187–1199 (2022). https://doi.org/10.1007/s00259-021-05573-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-021-05573-z