Abstract
Objective
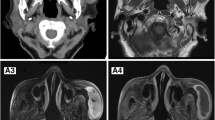
To identify if morphology of the entering and exiting nerve involved by a nerve sheath tumour in the brachial plexus can help differentiate between benign (B) and malignant (M) peripheral nerve sheath tumours (PNSTs).
Materials and methods
Retrospective review of 85 patients with histologically confirmed primary PNSTs of the brachial plexus over a 12.5-year period. Clinical data and all available MRI studies were independently evaluated by 2 consultant musculoskeletal radiologists blinded to the final histopathological diagnosis assessing for maximal lesion dimension, visibility and morphology of the entering and exiting nerve, and other well-documented features of PNSTs.
Results
The study included 47 males and 38 females with mean age 46.7 years (range, 8–81 years). There were 73 BPNSTs and 12 MPNSTs. The entering nerve was not identified in 5 (7%), was normal in 17 (23%), was tapered in 38 (52%) and showed lobular enlargement in 13 (18%) BPNSTs compared with 0 (0%), 0 (0%), 2 (17%) and 10 (83%) MPNSTs respectively. The exiting nerve was not identified in 5 (7%), was normal in 20 (27%), was tapered in 42 (58%) and showed lobular enlargement in 6 (8%) BPNSTs compared with 4 (33%), 0 (0%), 2 (17%) and 6 (50%) MPNSTs respectively. Increasing tumour size, entering and exiting nerve morphology and suspected MRI diagnosis were statistically significant differentiators between BPNST and MPNST (p < 0.001). IOC for nerve status was poor to fair but improved to good if normal/tapered appearance were considered together with improved specificity of 81–91% for BPNST and sensitivity of 75–83%.
Conclusions
Morphology of the adjacent nerve is a useful additional MRI feature for distinguishing BPNST from MPNST of the brachial plexus.





Similar content being viewed by others
References
Saifuddin A. Imaging tumours of the brachial plexus. Skelet Radiol. 2003;32:375–87.
Ogose A, Hotta T, Morita T, Yamamura S, Hosaka N, Kobayashi H, et al. Tumors of peripheral nerves: correlation of symptoms, clinical signs, imaging features, and histologic diagnosis. Skelet Radiol. 1999;28:183–8.
Li CS, Huang GS, Wu HD, Chen WT, Shih LS, Lii JM, et al. Differentiation of soft tissue benign and malignant peripheral nerve sheath tumors with magnetic resonance imaging. Clin Imaging. 2008;32:121–7.
Matsumine A, Kusuzaki K, Nakamura T, Nakazora S, Niimi R, Matsubara T, et al. Differentiation between neurofibromas and malignant peripheral nerve sheath tumors in neurofibromatosis 1 evaluated by MRI. J Cancer Res Clin Oncol. 2009;135:891–900.
Wasa J, et al. MRI features in the differentiation of malignant peripheral nerve sheath tumors and neurofibromas. AJR. 2010;194:1568–74.
Demehri S, Belzberg A, Blakeley J, Fayad LM. Conventional and functional MR imaging of peripheral nerve sheath tumors: initial experience. AJNR Am J Neuroradiol. 2014;35(8):1615–20.
Karsy M, Guan J, Ravindra VM, Stilwill S, Mahan MA. Diagnostic quality of magnetic resonance imaging interpretation for peripheral nerve sheath tumors: can malignancy be determined? J Neurol Surg A Cent Eur Neurosurg. 2016;77(6):495–504.
Soldatos T, Fisher S, Karri S, Ramzi A, Sharma R, Chhabra A. Advanced MRI imaging of peripheral nerve sheath tumors including diffusion imaging. Semin Musculoskelet Radiol. 2015;19:179–90.
Well L, Salamon J, Kaul MG, et al. Differentiation of peripheral nerve sheath tumors in patients with neurofibromatosis type 1 using diffusion-weighted magnetic resonance imaging. Neuro-Oncology. 2019;21(4):508–16.
Wu JS, Hochman MG. Soft-tissue tumors and tumorlike lesions: a systematic imaging approach. Radiology. 2009;253:297–316.
Salunke AA, Chen Y, Tan JH, et al. Intramuscular schwannoma: clinical and magnetic resonance imaging features. Singap Med J. 2015;56(10):555–7.
Bhargava R, Parham DM, Lasater OE, et al. MR imaging differentiation of benign and malignant peripheral nerve sheath tumors: use of the target sign. Pediatr Radiol. 1997;27:124–9.
Varma DG, Moulopoulos A, Sara AS, et al. MR imaging of extracranial nerve sheath tumors. J Comput Assist Tomogr. 1992;16(3):448–53.
Shimose S, Sugita T, Kubo T, et al. Major-nerve schwannomas versus intramuscular schwannomas. Acta Radiol. 2007;48:672–7.
Ahlawat S, Fayad LM. Imaging cellularity in benign and malignant peripheral nerve sheath tumors: utility of the “target sign” by diffusion weighted imaging. Eur J Radiol. 2018;102:195–201.
Koga H, Matsumoto S, Manabe J, Tanizawa T, Kawaguchi N. Definition of the target sign and its use for the diagnosis of schwannomas. Clin Orthop Relat Res. 2007;464:224–9.
Zhang Z, Deng L, Ding L, Meng Q. MR imaging differentiation of malignant soft tissue tumors from peripheral schwannomas with large size and heterogeneous signal intensity. Eur J Radiol. 2015;84(5):940–6.
Mazal AT, Ashikyan O, Cheng J, Le LQ, Chhabra A. Diffusion-weighted imaging and diffusion tensor imaging as adjuncts to conventional MRI for the diagnosis and management of peripheral nerve sheath tumors: current perspectives and future directions. Eur Radiol. 2019;29(8):4123–32.
Kim DH, Murovic JA, Tiel RL, Moes G, Kline DG. A series of 397 peripheral neural sheath tumors: 30-year experience at Louisiana State University Health Sciences Center. J Neurosurg. 2005;102(2):246–55.
Ahlawat S, Blakeley JO, Rodriguez FJ, Fayad LM. Imaging biomarkers for malignant peripheral nerve sheath tumors in neurofibromatosis type 1 [published correction appears in Neurology. 2020 Mar 17;94(11):504]. Neurology. 2019;93(11):e1076–84.
Schmidt M, Kasprian G, Amann G, Duscher D, Aszmann OC. Diffusion tensor tractography for the surgical management of peripheral nerve sheath tumors. Neurosurg Focus. 2015;39(3):E17.
Chhabra A, Thakkar RS, Andreisek G, et al. Anatomic MR imaging and functional diffusion tensor imaging of peripheral nerve tumors and tumorlike conditions. AJNR Am J Neuroradiol. 2013;34(4):8.
Murphey MD, Smith WS, Smith SE, Kransdorf MJ, Temple HT. Imaging of musculoskeletal neurogenic tumors: radiologic-pathologic correlation 1. Radiographics. 1999;19:1253–80.
Mauermann ML, Amrami KK, Kuntz NL, et al. Longitudinal study of intraneural perineurioma- a benign, focal hypertrophic neuropathy of youth. Brain. 2009;132:2265–76.
Lusk MD, Kline DG, Garcia CA. Tumors of the brachial plexus. Neurosurgery. 1987;21(4):439–53.
Jia X, Yang J, Chen L, Yu C, Kondo T. Primary brachial plexus tumors: clinical experiences of 143 cases. Clin Neurol Neurosurg. 2016;148:91–5.
Brahmi M, Thiesse P, Ranchere D, et al. Diagnostic accuracy of PET/CT-guided percutaneous biopsies for malignant peripheral nerve sheath tumors in neurofibromatosis type 1 patients. PLoS One. 2015;10(10):e0138386 Published 2015 Oct 7.
Pianta M, Chock E, Schlicht S, McCombe D. Accuracy and complications of CT-guided core needle biopsy of peripheral nerve sheath tumours. Skelet Radiol. 2015;44(9):1341–9.
Tøttrup M, Eriksen JD, Hellfritzsch MB, Sørensen FB, Baad-Hansen T. Diagnostic accuracy of ultrasound-guided core biopsy of peripheral nerve sheath tumors. J Clin Ultrasound. 2020;48(3):134–8.
Chee DW, Peh WC, Shek TW. Pictorial essay: imaging of peripheral nerve sheath tumours. Can Assoc Radiol J. 2011;62(3):176–82.
Kakkar C, Shetty CM, Koteshwara P, Bajpai S. Telltale signs of peripheral neurogenic tumors on magnetic resonance imaging. Indian J Radiol Imaging. 2015;25(4):453–8.
WHO Classification of Tumours Editorial Board. WHO Classification of Tumours of Soft Tissue and Bone. 5th ed. Lyon, France: IARC Press; 2020.
Acknowledgments
The authors would like to acknowledge Paul Bassett for statistical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pressney, I., Khoo, M., Khan, R. et al. Morphology of the entering and exiting nerve as a differentiating feature of benign from malignant peripheral nerve sheath tumours of the brachial plexus. Skeletal Radiol 50, 1557–1565 (2021). https://doi.org/10.1007/s00256-020-03689-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-020-03689-1