Abstract
Background
Lung ultrasound (US), which is radiation-free and cheaper than chest radiography (CXR), may be a useful modality for the diagnosis of pediatric pneumonia, but there are limited data from low- and middle-income countries.
Objectives
The aim of this study was to evaluate the diagnostic performance of non-radiologist, physician-performed lung US compared to CXR for pneumonia in children in a resource-constrained, African setting.
Materials and methods
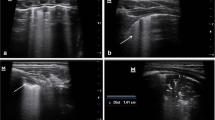
Children under 5 years of age enrolled in a South African birth cohort study, the Drakenstein Child Health Study, who presented with clinically defined pneumonia and had a CXR performed also had a lung US performed by a study doctor. Each modality was reported by two readers, using standardized methodology. Agreement between modalities, accuracy (sensitivity and specificity) of lung US and inter-rater agreement were assessed. Either consolidation or any abnormality (consolidation or interstitial picture) was considered as endpoints. In the 98 included cases (median age: 7.2 months; 53% male; 69% hospitalized), prevalence was 37% vs. 39% for consolidation and 52% vs. 76% for any abnormality on lung US and CXR, respectively. Agreement between modalities was poor for consolidation (observed agreement=61%, Kappa=0.18, 95% confidence interval [95% CI]: − 0.02 to 0.37) and for any abnormality (observed agreement=56%, Kappa=0.10, 95% CI: − 0.07 to 0.28). Using CXR as the reference standard, sensitivity of lung US was low for consolidation (47%, 95% CI: 31–64%) or any abnormality (5%, 95% CI: 43–67%), while specificity was moderate for consolidation (70%, 95% CI: 57–81%), but lower for any abnormality (58%, 95% CI: 37–78%). Overall inter-observer agreement of CXR was poor (Kappa=0.25, 95% CI: 0.11–0.37) and was significantly lower than the substantial agreement of lung US (Kappa=0.61, 95% CI: 0.50–0.75). Lung US demonstrated better agreement than CXR for all categories of findings, showing a significant difference for consolidation (Kappa=0.72, 95% CI: 0.58–0.86 vs. 0.32, 95% CI: 0.13–0.51).
Conclusion
Lung US identified consolidation with similar frequency to CXR, but there was poor agreement between modalities. The significantly higher inter-observer agreement of LUS compared to CXR supports the utilization of lung US by clinicians in a low-resource setting.
Graphical Abstract









Similar content being viewed by others
Data availability
The data presented in this study is available on reasonable request from the corresponding author.
References
Global Burden of Disease Child and Adolescent Health Collaboration, Kassebaum N, Kyu HH, Zoeckler L, et al (2017) Child and adolescent health from 1990 to 2015: findings from the global burden of diseases, injuries, and risk factors 2015 study. JAMA Pediatr 171:573–592. https://doi.org/10.1001/jamapediatrics.2017.0250
GBD 2015 LRI Collaborators (2017) Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory tract infections in 195 countries: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect Dis 17:1133–1161. https://doi.org/10.1016/S1473-3099(17)30396-1
Bradley JS, Byington CL, Shah SS et al (2011) The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis 53:e25-76. https://doi.org/10.1093/cid/cir531
World Health Organization (2014) Integrated Management of Childhood Illness (IMCI) Chart Booklet. 1–76
Harris M, Clark J, Coote N et al (2011) British Thoracic Society guidelines for the management of community acquired pneumonia in children: update 2011. Thorax 66:ii1-23. https://doi.org/10.1136/thoraxjnl-2011-200598
Shah SN, Bachur RG, Simel DL, Neuman MI (2017) Does this child have pneumonia?: the rational clinical examination systematic review. JAMA 318:462–471. https://doi.org/10.1001/jama.2017.9039
Lovrenski J, Petrović S, Balj-Barbir S et al (2016) Stethoscope vs. ultrasound probe - which is more reliable in children with suspected pneumonia? Acta Med Acad 45:39–50. https://doi.org/10.5644/ama2006-124.155
Bada C, Carreazo NY, Chalco JP, Huicho L (2007) Inter-observer agreement in interpreting chest X-rays on children with acute lower respiratory tract infections and concurrent wheezing. Sao Paulo Med J 125:150–154. https://doi.org/10.1590/s1516-31802007000300005
Correia MA, Mello MJG, Petribú NC et al (2011) Agreement on radiological diagnosis of acute lower respiratory tract infection in children. J Trop Pediatr 57:204–207. https://doi.org/10.1093/tropej/fmq071
Seear M, Awasthi S, Gowraiah V et al (2016) Predictive accuracy of chest radiographs in diagnosing tachypneic children. Indian J Pediatr 83:930–936. https://doi.org/10.1007/s12098-016-2057-7
Harel-Sterling M, Diallo M, Santhirakumaran S et al (2019) Emergency department resource use in pediatric pneumonia: point-of-care lung ultrasonography versus chest radiography. J Ultrasound Med 38:407–414. https://doi.org/10.1002/jum.14703
Pereda MA, Chavez MA, Hooper-Miele CC et al (2015) Lung ultrasound for the diagnosis of pneumonia in children: a meta-analysis. Pediatrics 135:714–722. https://doi.org/10.1542/peds.2014-2833
Heuvelings CC, Bélard S, Familusi MA et al (2019) Chest ultrasound for the diagnosis of paediatric pulmonary diseases: a systematic review and meta-analysis of diagnostic test accuracy. Br Med Bull 129:35–51. https://doi.org/10.1093/bmb/ldy041
Orso D, Ban A, Guglielmo N (2018) Lung ultrasound in diagnosing pneumonia in childhood: a systematic review and meta-analysis. J Ultrasound 21:183–195. https://doi.org/10.1007/s40477-018-0306-5
Xin H, Li J, Hu H-Y (2018) Is lung ultrasound useful for diagnosing pneumonia in children?: a meta-analysis and systematic review. Ultrasound Q 34:3–10. https://doi.org/10.1097/RUQ.0000000000000330
Najgrodzka P, Buda N, Zamojska A et al (2019) Lung ultrasonography in the diagnosis of pneumonia in children-a metaanalysis and a review of pediatric lung imaging. Ultrasound Q 35:157–163. https://doi.org/10.1097/RUQ.0000000000000411
Zar HJ, Barnett W, Myer L et al (2015) Investigating the early-life determinants of illness in Africa: the Drakenstein Child Health Study. Thorax 70:592–594. https://doi.org/10.1136/thoraxjnl-2014-206242
Cherian T, Mulholland EK, Carlin JB et al (2005) Standardized interpretation of paediatric chest radiographs for the diagnosis of pneumonia in epidemiological studies. Bull World Health Organ 83:353–359. /S0042–96862005000500011
Cicchetti DV, Feinstein AR (1990) High agreement but low kappa: II. Resolving the paradoxes. J Clin Epidemiol 43:551–558. https://doi.org/10.1016/0895-4356(90)90159-m
Ginsburg AS, Lenahan JL, Jehan F et al (2021) Performance of lung ultrasound in the diagnosis of pediatric pneumonia in Mozambique and Pakistan. Pediatr Pulmonol 56:551–560. https://doi.org/10.1002/ppul.25176
Yan J-H, Yu N, Wang Y-H et al (2020) Lung ultrasound vs chest radiography in the diagnosis of children pneumonia: systematic evidence. Medicine 99:e23671. https://doi.org/10.1097/MD.0000000000023671
Bloise S, La Regina DP, Pepino D et al (2021) Lung ultrasound compared to chest X-ray for the diagnosis of CAP in children. Pediatr Int 63:448–453. https://doi.org/10.1111/ped.14469
Liu X, Lian R, Tao Y et al (2015) Lung ultrasonography: an effective way to diagnose community-acquired pneumonia. Emerg Med J 32:433–438. https://doi.org/10.1136/emermed-2013-203039
Amatya Y, Rupp J, Russell FM et al (2018) Diagnostic use of lung ultrasound compared to chest radiograph for suspected pneumonia in a resource-limited setting. Int J Emerg Med 11:8. https://doi.org/10.1186/s12245-018-0170-2
Guitart C, Esteban E, Becerra J et al (2021) A training plan to implement lung ultrasound for diagnosing pneumonia in children. Pediatr Res. https://doi.org/10.1038/s41390-021-01928-2
Copetti R, Cattarossi L (2008) Ultrasound diagnosis of pneumonia in children. Radiol Med 113:190–198. https://doi.org/10.1007/s11547-008-0247-8
Shah VP, Tunik MG, Tsung JW (2013) Prospective evaluation of point-of-care ultrasonography for the diagnosis of pneumonia in children and young adults. JAMA Pediatr 167:119–125. https://doi.org/10.1001/2013.jamapediatrics.107
Zhan C, Grundtvig N, Klug BH (2018) Performance of bedside lung ultrasound by a pediatric resident: a useful diagnostic tool in children with suspected pneumonia. Pediatr Emerg Care 34:618–622. https://doi.org/10.1097/PEC.0000000000000888
Jones BP, Tay ET, Elikashvili I et al (2016) Feasibility and safety of substituting lung ultrasonography for chest radiography when diagnosing pneumonia in children: a randomized controlled trial. Chest 150:131–138. https://doi.org/10.1016/j.chest.2016.02.643
Acknowledgements
We thank the participants of the Drakenstein Child Health Study and their families and the study and clinical staff. We are also grateful to and would like to thank Eckart von Delft for interpreting the chest radiographs.
Funding
The study was funded by the Bill and Melinda Gates Foundation (OPP 1017641) with additional grants from the Medical Research Council of South Africa, National Research Foundation and National Institute of Health and H3Africa (1U01AI110466–01A1).
Author information
Authors and Affiliations
Contributions
S.A. conceived the study and design. J.A.M.S. and S.A. performed data collection. S.S.B.V., J.A.M.S. and S.A. performed data analysis. S.S.B.V., J.A.M.S. and S.A. drafted the initial manuscript. T.K., D.M.L.R. and H.J.R. assisted with edits and review of the drafts. S.S.B.V. and S.A. performed reviews and revisions. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Venkatakrishna, S.S.B., Stadler, J.A.M., Kilborn, T. et al. Evaluation of the diagnostic performance of physician lung ultrasound versus chest radiography for pneumonia diagnosis in a peri-urban South African cohort. Pediatr Radiol 54, 413–424 (2024). https://doi.org/10.1007/s00247-023-05686-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-023-05686-7