Abstract
Background
Magnetic resonance imaging (MRI) features of active sacroiliac joint inflammation include joint space fluid and enhancement, but it is unclear to what extent these are present in normal children.
Objective
To describe normal MRI appearances of pediatric sacroiliac joint spaces in boys and girls of varying ages.
Materials and methods
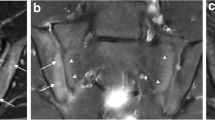
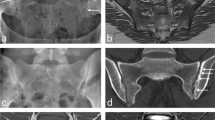
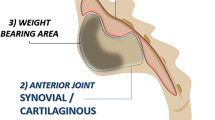
In this ethics-approved prospective study, 251 children (119 boys, 132 girls; mean age: 12.4 years, range: 6.1–18.0 years), had both oblique-coronal T1-weighted and short tau inversion recovery (STIR) sacroiliac joint MRI. Of these, 127 were imaged for other reasons and had asymptomatic sacroiliac joints (“normal cohort”) while 124 had low back pain with no features of sacroiliitis on initial clinical MRI review (“low-back-pain cohort”). Post-gadolinium T1-weighted sequences were available in 16/127 normal and 124/124 low-back-pain subjects. Three experienced radiologists scored high signal in the sacroiliac joint space on STIR (score 0=absent; 1=high signal compared to normal bone marrow present anywhere in the joint but not as bright as fluid [compared to vessels, cerebrospinal fluid]; 2=definite fluid signal in part of the joint; 3=definite fluid signal, entire vertical height, majority of slices) and, when available, joint space post-contrast enhancement (0=no high signal/enhancement; 1=thin, symmetrical, mildly increased linear high signal present in the joint space; 2=focal, thick or intense enhancement). Associations between joint signal scores, age, gender and sacral apophyseal closure were analysed.
Results
Increased signal on STIR (score 1–3) was present in 74.7% of pediatric sacroiliac joint spaces, as intense as fluid in 18.4%. There was no significant difference in proportion by gender, side or cohort, but girls showed peak signal earlier than boys (10 years old vs. 12 years old, respectively). On post-gadolinium T1-weighted sequences, a thin rim of increased signal was nearly universally seen in sacroiliac joint spaces without focal, intense or thick post-contrast enhancement.
Conclusion
Sacroiliac joint spaces of most children demonstrate mildly increased signal on STIR, compared to normal bone marrow, and thin rim-like enhancement on post-contrast T1 images, likely related to cartilage. These findings should not be confused with sacroiliitis.




Similar content being viewed by others
References
Burgos-Vargas R (2002) The juvenile-onset spondyloarthritides. Rheum Dis Clin N Am 28:531–560
Petty RE, Southwood TR, Manners P et al (2004) International League of Association for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton 2001. J Rheumatol 31:390–392
Colbert RA (2010) Classification of juvenile spondyloarthritis: enthesitis-related arthritis and beyond. Nat Rev Rheumatol 6:477–485
Sieper J, Rudwaleit M, Baraliakos X et al (2009) The Assessment of SpondyloArthritis International Society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis 68 Suppl 2:ii1–ii44
Oostveen J, Prevo R, den Boer J, van de Laar M (1999) Early detection of sacroiliitis on magnetic resonance imaging and subsequent development of sacroiliitis on plain radiography. A prospective, longitudinal study. J Rheumatol 26:1953–1958
Jaremko JL, Liu L, Winn NJ et al (2014) Diagnostic utility of magnetic resonance imaging and radiography in juvenile spondyloarthritis: evaluation of the sacroiliac joints in controls and affected subjects. J Rheumatol 41:963–970
Weiss PF, Xiao R, Biko DM, Chauvin NA (2016) Assessment of sacroiliitis at diagnosis of juvenile spondyloarthritis by radiography, magnetic resonance imaging, and clinical examination. Arthritis Care Res (Hoboken) 68:187–194
Lambert RGW, Bakker PAC, van der Heijde D et al (2016) Defining active sacroiliitis on MRI for classification of axial spondyloarthritis: update by the ASAS MRI working group. Ann Rheum Dis 75:1958–1963
Maksymowych WP, Lambert RG, Østergaard M et al (2019) MRI lesions in the sacroiliac joints of patients with spondyloarthritis: an update of definitions and validation by the ASAS MRI working group. Ann Rheum Dis 78:1550–1558
Puhakka KB, Melsen F, Jurik AG et al (2004) MR imaging of the normal sacroiliac joint with correlation to histology. Skeletal Radiol 33:15–28
Otobo TM, Conaghan PG, Maksymowych WP et al (2019) Preliminary definitions for sacroiliac joint pathologies in the OMERACT juvenile idiopathic arthritis magnetic resonance imaging score (OMERACT JAMRIS-SIJ). J Rheumatol 46:1192–1197
De Grove V, Willekens I, Lenchik L et al (2018) Fluid distribution in ankle and midfoot joints: MR findings in asymptomatic volunteers. Surg Radiol Anat 40:481–487
Ginalski JM, Landry M, Meuli RA (1993) Normal range of intraarticular fluid in the knee of healthy volunteers: easy evaluation with MRI. Eur Radiol 3:135–137
Mitchell DG, Rao V, Dalinka M et al (1986) MRI of joint fluid in the normal and ischemic hip. AJR Am J Roentgenol 146:1215–1218
Weber U, Jurik AG, Zejden A et al (2018) Frequency and anatomic distribution of magnetic resonance imaging features in the sacroiliac joints of young athletes: exploring "background noise" toward a data-driven definition of sacroiliitis in early spondyloarthritis. Arthritis Rheumatol 70:736–745
Chauvin NA, Xiao R, Brandon TG et al (2019) MRI of the sacroiliac joint in healthy children. AJR Am J Roentgenol 212:1303–1309
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Herregods N, Jans LBO, Chen M et al (2021) Normal subchondral high T2 signal on MRI mimicking sacroiliitis in children: frequency, age distribution, and relationship to skeletal maturity. Eur Radiol 31:3498–3507
Oudjhane K (2015) Normal development. In: Stein-Wexler R, Wootton-Gorges S, Ozonoff M (eds) Pediatric orthopedic imaging, 1st edn. Springer, New York
Soliman A, De Sanctis V, Elalaily R, Bedair S (2014) Advances in pubertal growth and factors influencing it: can we increase pubertal growth? Indian J Endocrinol Metab 18:S53–S62
Rieter JFMM, Tanturri de Horatio L, Nusman CM et al (2016) The many shades of enhancement: timing of post-gadolinium images strongly influences the scoring of juvenile idiopathic arthritis wrist involvement on MRI. Pediatr Radiol 46:1562–1567
Herregods N, Dehoorne J, Joos R et al (2015) Diagnostic value of MRI features of sacroiliitis in juvenile spondyloarthritis. Clin Radiol 70:1428–1438
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Herregods, N., Jans, L.B.O., Paschke, J. et al. Magnetic resonance imaging findings in the normal pediatric sacroiliac joint space that can simulate disease. Pediatr Radiol 51, 2530–2538 (2021). https://doi.org/10.1007/s00247-021-05168-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-021-05168-8