Abstract
Purpose
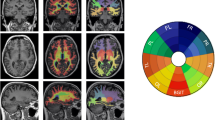
We investigated the volumetric changes in the components of the cholinergic pathway for patients with early mild cognitive impairment (EMCI) and those with late mild cognitive impairment (LMCI). The effect of patients’ apolipoprotein 4 (APOE-ε4) allele status on the structural changes were analyzed.
Methods
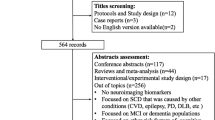
Structural magnetic resonance imaging data were collected. Patients’ demographic information, plasma data, and validated global cognitive composite scores were included. Relevant features were extracted for constructing machine learning models to differentiate between EMCI (n = 312) and LMCI (n = 541) and predict patients’ neurocognitive function. The data were analyzed primarily through one-way analysis of variance and two-way analysis of covariance.
Results
Considerable differences were observed in cholinergic structural changes between patients with EMCI and LMCI. Cholinergic atrophy was more prominent in the LMCI cohort than in the EMCI cohort (P < 0.05 family-wise error corrected). APOE-ε4 differentially affected cholinergic atrophy in the LMCI and EMCI cohorts. For LMCI cohort, APOE-ε4 carriers exhibited increased brain atrophy (left amygdala: P = 0.001; right amygdala: P = 0.006, and right Ch123, P = 0.032). EMCI and LCMI patients showed distinctive associations of gray matter volumes in cholinergic regions with executive (R2 = 0.063 and 0.030 for EMCI and LMCI, respectively) and language (R2 = 0.095 and 0.042 for EMCI and LMCI, respectively) function.
Conclusions
Our data confirmed significant cholinergic atrophy differences between early and late stages of mild cognitive impairment. The impact of the APOE-ε4 allele on cholinergic atrophy varied between the LMCI and EMCI groups.







Similar content being viewed by others
Data availability
The datasets presented in this study are available in the Alzheimer’s Disease Neuroimaging Initiative (ADNI) repository, https://adni.loni.usc.edu/.
References
Lin SY, Lin PC, Lin YC et al (2022) The Clinical Course of Early and Late Mild Cognitive Impairment. Front Neurol 13:685636
Morris JC, Storandt M, Miller JP et al (2001) Mild cognitive impairment represents early-stage Alzheimer disease. Arch Neurol 58:397–405
Jessen F, Wolfsgruber S, Wiese B et al (2014) AD dementia risk in late MCI, in early MCI, and in subjective memory impairment. Alzheimers Dement 10:76–83
Aisen PS, Petersen RC, Donohue MC et al (2010) Clinical Core of the Alzheimer’s Disease Neuroimaging Initiative: progress and plans. Alzheimers Dement 6:239–246
Cai S, Huang L, Zou J et al (2015) Changes in thalamic connectivity in the early and late stages of amnestic mild cognitive impairment: a resting-state functional magnetic resonance study from ADNI. PLoS ONE 10:e0115573
Weiner MW, Veitch DP, Aisen PS et al (2015) 2014 Update of the Alzheimer’s Disease Neuroimaging Initiative: A review of papers published since its inception. Alzheimer’s Dementia 11:e1-120
Jessen F, Wolfsgruber S, Wiese B et al (2014) AD dementia risk in late MCI, in early MCI, and in subjective memory impairment. Alzheimer’s Dementia 10:76–83
Edmonds EC, McDonald CR, Marshall A et al (2019) Early versus late MCI: Improved MCI staging using a neuropsychological approach. Alzheimer’s Dementia 15:699–708
Jitsuishi T, Yamaguchi A (2022) Searching for optimal machine learning model to classify mild cognitive impairment (MCI) subtypes using multimodal MRI data. Sci Rep 12:4284
Zamani J, Sadr A, Javadi AH (2022) Classification of early-MCI patients from healthy controls using evolutionary optimization of graph measures of resting-state fMRI, for the Alzheimer’s disease neuroimaging initiative. PLoS ONE 17:e0267608
Mesulam MM (2013) Cholinergic circuitry of the human nucleus basalis and its fate in Alzheimer’s disease. J Comparative Neurol 521:4124–4144
Schmitz TW, Mur M, Aghourian M, Bedard M-A, Spreng RN (2018) Longitudinal Alzheimer’s Degeneration Reflects the Spatial Topography of Cholinergic Basal Forebrain Projections. Cell Rep 24:38–46
Arendt T, Brückner MK, Morawski M, Jäger C, Gertz H-J (2015) Early neurone loss in Alzheimer’s disease: cortical or subcortical? Acta Neuropathol Commun 3:1–11
Baker-Nigh A, Vahedi S, Davis EG et al (2015) Neuronal amyloid-β accumulation within cholinergic basal forebrain in ageing and Alzheimer’s disease. Brain 138:1722–1737
Braak H, Del Tredici K (2015) The preclinical phase of the pathological process underlying sporadic Alzheimer’s disease. Brain 138:2814–2833
Schmitz T, Nathan Spreng R (2016) Alzheimer’s Disease Neuroimaging I (2016) Basal forebrain degeneration precedes and predicts the cortical spread of Alzheimer’s pathology. Nat Commun 7:13249
Kondo H, Zaborszky L (2016) Topographic organization of the basal forebrain projections to the perirhinal, postrhinal, and entorhinal cortex in rats. J Comparative Neurol 524:2503–2515
Fernández-Cabello S, Kronbichler M, Van Dijk KRA et al (2020) Basal forebrain volume reliably predicts the cortical spread of Alzheimer’s degeneration. Brain 143:993–1009
Castellano JM, Kim J, Stewart FR et al (2011) Human apoE Isoforms Differentially Regulate Brain Amyloid-β Peptide Clearance. Sci Translat Med 3:89ra57-89ra57
Chai AB, Lam HHJ, Kockx M, Gelissen IC (2021) Apolipoprotein E isoform-dependent effects on the processing of Alzheimer's amyloid-β. Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids 1866:158980 https://doi.org/10.1016/j.bbalip.2021.158980
Chen Z-R, Huang J-B, Yang S-L, Hong F-F (2022) Role of Cholinergic Signaling in Alzheimer & Disease. Molecules 27:1816
Ramos-Rodriguez JJ, Pacheco-Herrero M, Thyssen D et al (2013) Rapid β-Amyloid Deposition and Cognitive Impairment After Cholinergic Denervation in APP/PS1 Mice. J Neuropathol Exp Neurol 72:272–285
Hampel H, Mesulam M-M, Cuello AC et al (2018) The cholinergic system in the pathophysiology and treatment of Alzheimer’s disease. Brain 141:1917–1933
Hoskin JL, Al-Hasan Y, Sabbagh MN (2018) Nicotinic Acetylcholine Receptor Agonists for the Treatment of Alzheimer’s Dementia: An Update. Nicotine Tob Res 21:370–376
Bott JB, Héraud C, Cosquer B et al (2016) APOE-Sensitive Cholinergic Sprouting Compensates for Hippocampal Dysfunctions Due to Reduced Entorhinal Input. J Neurosci 36:10472–10486
Weiner MW, Veitch DP, Aisen PS et al (2012) The Alzheimer’s Disease Neuroimaging Initiative: a review of papers published since its inception. Alzheimer’s Dementia 8:S1–S68
Crane PK, Carle A, Gibbons LE et al (2012) Development and assessment of a composite score for memory in the Alzheimer’s Disease Neuroimaging Initiative (ADNI). Brain Imaging Behav 6:502–516
Gibbons LE, Carle AC, Mackin RS et al (2012) A composite score for executive functioning, validated in Alzheimer’s Disease Neuroimaging Initiative (ADNI) participants with baseline mild cognitive impairment. Brain Imaging Behav 6:517–527
Eickhoff SB, Stephan KE, Mohlberg H et al (2005) A new SPM toolbox for combining probabilistic cytoarchitectonic maps and functional imaging data. Neuroimage 25:1325–1335
Anthoula T, Marianna S, Penelope M et al (2018) Co morbidity and neuroimaging in Alzheimer’s. Gerontology & Geriatrics Studies. https://scholar.google.com.tw/scholar?hl=zh-TW&as_sdt=0%2C5&q=Anthoula+T%2C+Marianna+S%2C+Penelope+M+et+al+%282018%29+Co+morbidity+and+Neuroimaging+in+Alzheimer%E2%80%99s.+Gerontology+%26+Geriatrics+Studies
Zaborszky L, Hoemke L, Mohlberg H, Schleicher A, Amunts K, Zilles K (2008) Stereotaxic probabilistic maps of the magnocellular cell groups in human basal forebrain. Neuroimage 42:1127–1141
Gaser C, Kurth F (2017) Manual computational anatomy toolbox-CAT12. University of Jena, Structural brain mapping Group at the Departments of Psychiatry and Neurology
Nemoto K, Dan I, Rorden C et al (2011) Lin4Neuro: a customized Linux distribution ready for neuroimaging analysis. BMC Med Imaging 11:3–3
Núñez C, Callén A, Lombardini F, Compta Y, Stephan-Otto C, AsDN I (2020) Different cortical gyrification patterns in Alzheimer’s disease and impact on memory performance. Ann Neurol 88:67–80
Gaser C, Dahnke R, Thompson PM, Kurth F, Luders E, Initiative AsDN (2022) CAT – A Computational Anatomy Toolbox for the Analysis of Structural MRI Data. bioRxiv. https://doi.org/10.1101/2022.06.11.495736:2022.2006.2011.495736
Smith SM, Nichols TE (2009) Threshold-free cluster enhancement: addressing problems of smoothing, threshold dependence and localisation in cluster inference. Neuroimage 44:83–98
Cortes C, Vapnik V (1995) Support-vector networks Machine learning 20:273–297
Camps-Valls G, Gómez-Chova L, Calpe-Maravilla J et al (2004) Robust support vector method for hyperspectral data classification and knowledge discovery. IEEE Trans Geosci Remote Sens 42:1530–1542
Guo S, Lai C, Wu C et al (2017) Conversion discriminative analysis on mild cognitive impairment using multiple cortical features from MR images. Front Aging Neurosci 9:146
Bisong E (2019) Building machine learning and deep learning models on Google cloud platform. Springer
Paper (2020) Hands-on Scikit-Learn for Machine Learning Applications. Apress https://doi.org/10.1007/978-1-4842-5373-1
Garreta R, Moncecchi G (2013) Learning scikit-learn: machine learning in python. Packt Publishing Ltd. https://scholar.google.com.tw/scholar?hl=zh-TW&as_sdt=0%2C5&q=Garreta+R%2C+Moncecchi+G+%282013%29+Learning+scikit-learn%3A+machine+learning+in+python.+Packt+Publishing+Ltd&btnG=
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Bachli MB, Sedeño L, Ochab JK et al (2020) Evaluating the reliability of neurocognitive biomarkers of neurodegenerative diseases across countries: A machine learning approach. Neuroimage 208:116456
Liu Y, Tan L, Wang H-F et al (2016) Multiple effect of APOE genotype on clinical and neuroimaging biomarkers across Alzheimer’s disease spectrum. Mol Neurobiol 53:4539–4547
Jack CR Jr, Knopman DS, Jagust WJ et al (2010) Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. The Lancet Neurology 9:119–128
Lim YY, Laws SM, Villemagne VL et al (2016) Aβ-related memory decline in APOE ε4 noncarriers: Implications for Alzheimer disease. Neurology 86:1635–1642
Bekdash RA (2021) The Cholinergic System, the Adrenergic System and the Neuropathology of Alzheimer’s Disease. Int J Mol Sci 22:1273
Schmitz TW, Soreq H, Poirier J, Spreng RN (2020) Longitudinal basal forebrain degeneration interacts with trem2/c3 biomarkers of inflammation in presymptomatic Alzheimer’s disease. J Neurosci 40:1931–1942
La Joie R, Bejanin A, Fagan AM et al (2018) Associations between [18F] AV1451 tau PET and CSF measures of tau pathology in a clinical sample. Neurology 90:e282–e290
Suzuki K, Hirakawa A, Ihara R et al (2020) Effect of apolipoprotein E ε4 allele on the progression of cognitive decline in the early stage of Alzheimer’s disease. Alzheimer’s Dementia: Translat Res Clin Interventions 6:e12007
O’Donoghue MC, Murphy SE, Zamboni G, Nobre AC, Mackay CE (2018) APOE genotype and cognition in healthy individuals at risk of Alzheimer’s disease: A review. Cortex 104:103–123
Acknowledgements
Data collection and sharing for this project was funded by the Alzheimer’s Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012). ADNI was funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: AbbVie, Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen; Bristol-Myers Squibb Company; CereSpir, Inc.; Cogstate; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche Ltd. and its affiliated company Genentech, Inc.; Fujirebio; GE Healthcare; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research & Development LLC.; Lumosity; Lundbeck; Merck & Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. This Canadian Institutes of Health Research was providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). This grantee organization was the Northern California Institute for Research and Education, and this study was coordinated by the Alzheimer’s Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California.
Funding
This study was supported by Taipei Medical University Hospital, with grants numbered 105TMU-TMUH-05, 106TMU-TMUH-21, and 107TMU-TMUH-09, along with a grant number TMU110-F-011 from Taipei Medical University. Additionally, funding was provided by the Ministry of Science and Technology, Republic of China, under grant number MOST108-2221-E-038–007-MY2.
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Conflicts of interest/Competing interests
We declare that we have no conflict of interest. Hui-Hsien Lin worked for Rotary Trading Co., Ltd. The other authors confirmed that the study was carried out without any affiliations or financial ties that could be seen as a possible conflict of interest and that Rotary Trading Co., Ltd did not participate in analysis or writing of this manuscript.
Ethics approval
All procedures performed in the ADNI studies involving human participants were in accordance with the ethical standards of the institutional research committees and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Written informed consent was obtained from all participants or their authorized representatives. The study procedures were approved by the institutional review boards of all participating sites and more details can be found at: (http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf).
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Data used in preparation of this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in analysis or writing of this report. A complete listing of ADNI investigators can be found at: http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lai, YL.L., Hsu, FT., Yeh, SY. et al. Atrophy of the cholinergic regions advances from early to late mild cognitive impairment. Neuroradiology 66, 543–556 (2024). https://doi.org/10.1007/s00234-024-03290-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-024-03290-6