Abstract
Purpose
The purpose of this study was to evaluate differences in endovascular treatment (EVT) outcomes in M1 segment middle cerebral artery occlusion (MCAO) patients with different pathologic subtypes.
Methods
Patients with MCAO who received EVT from July 2014 to December 2020 were categorized into three groups: embolism without internal carotid artery steno-occlusion (MCAO-E), in situ atherosclerotic thrombosis (MCAO-AS) and embolism from tandem ICA steno-occlusion (MCAO-T). Baseline characteristics, EVT-related factors and clinical outcomes were compared between groups. Multivariable regression analyses were performed to evaluate the relationship between aetiologic classification and outcomes at 90 days after stroke.
Results
Among eligible patients (n = 220), MCAO-E (n = 129, 58.6%) was the most common aetiology, followed by MCAO-AS (n = 47, 21.4%) and MCAO-T (n = 44, 20.0%). Patients with MCAO-E were significantly older but had a lower rate of dyslipidaemia and smoking history than those with MCAO-AS. Although patients with MCAO-AS and MCAO-T more often required rescue balloon angioplasty and stenting (p < 0.001), no significant difference in the rate of final recanalization was found. Patients in the MCAO-AS group obtained better functional outcomes (90-day modified Rankin Scale score, 0–2) (p = 0.002) and lower mortality than in the MCAO-E group (p = 0.009). On multivariable logistic regression, we failed to find that stroke subtype was an independent predictor of functional outcomes and mortality.
Conclusions
Patients with acute MCA M1 occlusion stroke due to different pathogeneses had comparable successful recanalization rates and functional independence at 90 days. The optimal management for MCAO patients with different aetiologies requires further research.





Similar content being viewed by others
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Statistical code is available upon reasonable request.
References
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A et al (2015) Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 372:2296–2306. https://doi.org/10.1056/NEJMoa1503780
Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T et al (2016) Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol 15:1138–1147. https://doi.org/10.1016/S1474-4422(16)30177-6
Wang Y, Zhao X, Liu L, Soo YO, Pu Y, Pan Y et al (2014) Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in China: the Chinese Intracranial Atherosclerosis (CICAS) Study. Stroke 45:663–669. https://doi.org/10.1161/STROKEAHA.113.003508
Kim GE, Yoon W, Kim SK, Kim BC, Heo TW, Baek BH et al (2016) Incidence and clinical significance of acute reocclusion after emergent angioplasty or stenting for underlying intracranial stenosis in patients with acute stroke. AJNR Am J Neuroradiol 37:1690–1695. https://doi.org/10.3174/ajnr.A4770
Al Kasab S, Almadidy Z, Spiotta AM, Turk AS, Chaudry MI, Hungerford JP et al (2017) Endovascular treatment for AIS with underlying ICAD. J Neurointerv Surg 9:948–951. https://doi.org/10.1136/neurintsurg-2016-012529
Lee JS, Hong JM, Lee KS, Suh HI, Choi JW, Kim SY (2016) Primary stent retrieval for acute intracranial large artery occlusion due to atherosclerotic disease. J Stroke 18:96–101. https://doi.org/10.5853/jos.2015.01347
Tsang ACO, Orru E, Klostranec JM, Yang IH, Lau KK, Tsang FCP et al (2019) Thrombectomy outcomes of intracranial atherosclerosis-related occlusions. Stroke 50:1460–1466. https://doi.org/10.1161/STROKEAHA.119.024889
Dobrocky T, Kaesmacher J, Bellwald S, Piechowiak E, Mosimann PJ, Zibold F et al (2019) Stent-retriever thrombectomy and rescue treatment of M1 occlusions due to underlying intracranial atherosclerotic stenosis: cohort analysis and review of the literature. Cardiovasc Intervent Radiol 42:863–872. https://doi.org/10.1007/s00270-019-02187-9
Lee JS, Lee SJ, Yoo JS, Hong JH, Kim CH, Kim YW et al (2018) Prognosis of acute intracranial atherosclerosis-related occlusion after endovascular treatment. J Stroke 20:394–403. https://doi.org/10.5853/jos.2018.01627
Jia B, Feng L, Liebeskind DS, Huo X, Gao F, Ma N et al (2018) Mechanical thrombectomy and rescue therapy for intracranial large artery occlusion with underlying atherosclerosis. J Neurointerv Surg 10:746–750. https://doi.org/10.1136/neurintsurg-2017-013489
Yoon W, Kim SK, Park MS, Kim BC, Kang HK (2015) Endovascular treatment and the outcomes of atherosclerotic intracranial stenosis in patients with hyperacute stroke. Neurosurgery 76(680):686. https://doi.org/10.1227/NEU.0000000000000694 discussion 686
Lee D, Lee DH, Suh DC, Kim BJ, Kwon SU, Kwon HS et al (2020) Endovascular treatment in patients with cerebral artery occlusion of three different etiologies. J Stroke 22:234–244. https://doi.org/10.5853/jos.2019.02404
Guglielmi V, LeCouffe NE, Zinkstok SM, Compagne KCJ, Eker R, Treurniet KM et al (2019) Collateral circulation and outcome in atherosclerotic versus cardioembolic cerebral large vessel occlusion. Stroke 50:3360–3368. https://doi.org/10.1161/STROKEAHA.119.026299
Assis Z, Menon BK, Goyal M, Demchuk AM, Shankar J, Rempel JL et al (2018) Acute ischemic stroke with tandem lesions: technical endovascular management and clinical outcomes from the ESCAPE trial. J Neurointerv Surg 10:429–433. https://doi.org/10.1136/neurintsurg-2017-013316
Samuels OB, Joseph GJ, Lynn MJ, Smith HA, Chimowitz MI (2000) A standardized method for measuring intracranial arterial stenosis. AJNR Am J Neuroradiol 21:643–646
Fiorelli M, Bastianello S, von Kummer R, del Zoppo GJ, Larrue V, Lesaffre E et al (1999) Hemorrhagic transformation within 36 hours of a cerebral infarct: relationships with early clinical deterioration and 3-month outcome in the European Cooperative Acute Stroke Study I (ECASS I) cohort. Stroke 30:2280–2284. https://doi.org/10.1161/01.str.30.11.2280
Tan IY, Demchuk AM, Hopyan J, Zhang L, Gladstone D, Wong K et al (2009) CT angiography clot burden score and collateral score: correlation with clinical and radiologic outcomes in acute middle cerebral artery infarct. AJNR Am J Neuroradiol 30:525–531. https://doi.org/10.3174/ajnr.A1408
Christoforidis GA, Mohammad Y, Kehagias D, Avutu B, Slivka AP (2005) Angiographic assessment of pial collaterals as a prognostic indicator following intra-arterial thrombolysis for acute ischemic stroke. AJNR Am J Neuroradiol 26:1789–1797
Yang W, Zhang Y, Li Z, Zhang L, Li H, Hua W et al (2021) Differences in safety and efficacy of endovascular treatment for acute ischemic stroke: a propensity score analysis of intracranial atherosclerosis-related occlusion versus embolism. Clin Neuroradiol 31:457–464. https://doi.org/10.1007/s00062-020-00899-x
Treurniet KM, Yoo AJ, Berkhemer OA, Lingsma HF, Boers AM, Fransen PS et al (2016) Clot burden score on baseline computerized tomographic angiography and intra-arterial treatment effect in acute ischemic stroke. Stroke 47:2972–2978. https://doi.org/10.1161/STROKEAHA.116.014565
Hao Y, Yang D, Wang H, Zi W, Zhang M, Geng Y et al (2017) Predictors for symptomatic intracranial hemorrhage after endovascular treatment of acute ischemic stroke. Stroke 48:1203–1209. https://doi.org/10.1161/STROKEAHA.116.016368
Huo X, Sun D, Raynald JB, Tong X, Wang A et al (2022) Endovascular treatment in acute ischemic stroke with large vessel occlusion according to different stroke subtypes: data from ANGEL-ACT registry. Neurol Ther 11:151–165. https://doi.org/10.1007/s40120-021-00301-z
Kim SJ, Seok JM, Bang OY, Kim GM, Kim KH, Jeon P et al (2009) MR mismatch profiles in patients with intracranial atherosclerotic stroke: a comprehensive approach comparing stroke subtypes. J Cereb Blood Flow Metab 29:1138–1145. https://doi.org/10.1038/jcbfm.2009.38
Albers GW, Thijs VN, Wechsler L, Kemp S, Schlaug G, Skalabrin E et al (2006) Magnetic resonance imaging profiles predict clinical response to early reperfusion: the diffusion and perfusion imaging evaluation for understanding stroke evolution (DEFUSE) study. Ann Neurol 60:508–517. https://doi.org/10.1002/ana.20976
Baek JH, Kim BM, Heo JH, Kim DJ, Nam HS, Kim YD (2018) Outcomes of endovascular treatment for acute intracranial atherosclerosis-related large vessel occlusion. Stroke 49:2699–2705. https://doi.org/10.1161/STROKEAHA.118.022327
Huang X, Cai Q, Xiao L, Gu M, Liu Y, Zhou Z et al (2019) Influence of procedure time on outcome and hemorrhagic transformation in stroke patients undergoing thrombectomy. J Neurol 266:2560–2570. https://doi.org/10.1007/s00415-019-09451-5
Anadani M, Finitsis S, Clarencon F, Richard S, Marnat G, Bourcier R et al (2022) Collateral status reperfusion and outcomes after endovascular therapy: insight from the endovascular treatment in ischemic stroke (ETIS) registry. J Neurointerv Surg 14:551–557. https://doi.org/10.1136/neurintsurg-2021-017553
Rebello LC, Bouslama M, Haussen DC, Grossberg JA, Dehkharghani S, Anderson A et al (2017) Stroke etiology and collaterals: atheroembolic strokes have greater collateral recruitment than cardioembolic strokes. Eur J Neurol 24:762–767. https://doi.org/10.1111/ene.13287
Timsit SG, Sacco RL, Mohr JP, Foulkes MA, Tatemichi TK, Wolf PA et al (1993) Brain infarction severity differs according to cardiac or arterial embolic source. Neurology 43:728–733. https://doi.org/10.1212/wnl.43.4.728
Funding
This work was supported by the Anhui University Provincial Natural Science Research Project (No. KJ2021A0843) and the Scientific Research Project for middle-aged and young people of Wannan Medical College (No. WK2020F24).
Author information
Authors and Affiliations
Contributions
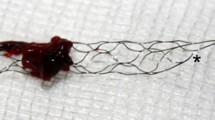
XX, XH, and ZZ planned and conceived the study. WH and GL collected the data. QY and KY analyzed the image; YG and XY interpreted the data. XX, KY, WW, and JX wrote and critically revised the manuscript. All the authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
We declare that we have no conflict of interest.
Ethics approval
Subjects (or their parents or guardians) have given their written informed consent for being treated. The paper is exempt from ethical committee approval, since endovascular thrombectomy is considered the standard of care for treating acute ischemic stroke, and there has been no disclosure of the patients’ information in this paper.
Consent to participate
The need for individual patient consent has been waived.
Consent for publication
The need for individual patient consent has been waived; therefore consent for publication is not required.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiangjun Xu, Ke Yang and Junfeng Xu contributed equally to this work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, X., Yang, K., Xu, J. et al. Endovascular treatment in patients with middle cerebral artery occlusion of different aetiologies. Neuroradiology 65, 609–618 (2023). https://doi.org/10.1007/s00234-022-03078-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-022-03078-6