Abstract
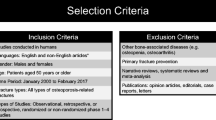
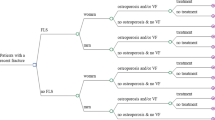
Fracture liaison services (FLS) have been proven clinically effective and cost-effective in preventing subsequent fractures among patients with an existing fragility fracture. Little is known about their monetary benefits such as their return on investment (ROI). This systematic review aimed to investigate the ROI of FLS and identify the FLS characteristics with better ROI. Studies on the cost-effectiveness of FLS published between January 2000 and December 2022 were searched from MEDLINE, EMBASE, PubMed, and Cochrane Central. Two independent reviewers conducted study selection and data extraction. ROI was calculated based on the difference between monetary benefits and FLS costs divided by the FLS costs. Subgroup analysis of ROI was performed across FLS types and FLS design details. A total of 23 FLS were included in this review. The majority of them were targeting patients aged over 50 years having fractures without identified sites. The mean ROI of these FLS was 10.49 (with a median ROI of 7.57), and 86.96% of FLS had positive ROI. FLS making treatment recommendations yielded the highest ROI (with a mean ROI of 18.39 and a median of 13.60). Incorporating primary care providers (with a mean ROI of 16.04 and a median of 13.20) or having them as program leaders (with a mean ROI of 12.07 and a median of 12.07) has demonstrated a high ROI. FLS for specific fracture sites had great monetary return. Intensive FLS such as type A and B FLS programs had higher ROI than non-intensive type C and D FLS. This review revealed a 10.49-fold monetary return of FLS. Identified characteristics contributing to greater economic return informed value-for-money FLS designs. Findings highlight the importance of FLS and the feasibility of expanding their contribution in mitigating the economic burden of osteoporotic fracture and are conducive to the promotion of FLS internationally.

Similar content being viewed by others
Data Availability
All data analyzed as part of this study are included in this published article.
References
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17(12):1726–1733. https://doi.org/10.1007/s00198-006-0172-4 [publishedOnline First: 20060916]
Dobre R, Niculescu DA, Petca RC et al (2021) Adherence to anti-osteoporotic treatment and clinical implications after hip fracture: a systematic review. J Pers Med 11(5). https://doi.org/10.3390/jpm11050341 [published Online First: 20210424]
Long H, Cao R, Zhang H et al (2022) Incidence of hip fracture among middle-aged and older Chinese from 2013 to 2015: results from a nationally representative study. Arch Osteoporos 17(1):48. https://doi.org/10.1007/s11657-022-01082-0 [published Online First: 20220311]
Si L, Winzenberg TM, de Graaff B et al (2014) A systematic review and meta-analysis of utility-based quality of life for osteoporosis-related conditions. Osteoporos Int 25(8):1987–1997. https://doi.org/10.1007/s00198-014-2636-2 [published Online First: 20140222]
van Geel TA, van Helden S, Geusens PP et al (2009) Clinical subsequent fractures cluster in time after first fractures. Ann Rheum Dis 68(1):99–102. https://doi.org/10.1136/ard.2008.092775 [published Online First: 20080803]
González-Quevedo D, Pérez-Del-Río V, Moriel-Garceso D et al (2022) A 2-year follow-up of a novel fracture liaison service: can we reduce the mortality in elderly hip fracture patients? A prospective cohort study. Osteoporos Int 33(8):1695–1702. https://doi.org/10.1007/s00198-022-06298-x [published Online First: 20220331]
Javaid MK (2021) Efficacy and efficiency of fracture liaison services to reduce the risk of recurrent osteoporotic fractures. Aging Clin Exp Res 33(8):2061–2067. https://doi.org/10.1007/s40520-021-01844-9 [published Online First: 20210528]
Hoit G, Whelan DB, Atrey A et al (2022) Association of age, sex and race with prescription of anti-osteoporosis medications following low-energy hip fracture in a retrospective registry cohort. PLoS One 17(12):e0278368. https://doi.org/10.1371/journal.pone.0278368 [published Online First: 20221201]
Singh S, Whitehurst DG, Funnell L et al (2019) Breaking the cycle of recurrent fracture: implementing the first fracture liaison service (FLS) in British Columbia, Canada. Arch Osteoporos 14(1):116. https://doi.org/10.1007/s11657-019-0662-6 [published Online First: 20191127]
Akesson K, Marsh D, Mitchell PJ et al (2013) Capture the fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24(8):2135–2152. https://doi.org/10.1007/s00198-013-2348-z [published Online First: 20130416]
van den Berg P, van Haard PMM, van der Veer E et al (2018) A dedicated Fracture Liaison Service telephone program and use of bone turnover markers for evaluating 1-year persistence with oral bisphosphonates. Osteoporos Int 29(4):813–824. https://doi.org/10.1007/s00198-017-4340-5 [published Online First: 20171219]
IOF Capture the Fracture [cited 2023 30th March]. Available from: https://www.capturethefracture.org/ accessed 30th March 2023.,
Mugnier B, Daumas A, Doddoli S et al (2020) Adherence to fracture liaison service programs in patients over 70: the hidden part of the iceberg. Osteoporos Int 31(4):765–774. https://doi.org/10.1007/s00198-020-05290-7 [published Online First: 20200111]
Wu C-H, Tu S-T, Chang Y-F et al (2018) Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: a systematic literature review and meta-analysis. Bone 111:92–100
Li N, Hiligsmann M, Boonen A et al (2021) The impact of fracture liaison services on subsequent fractures and mortality: a systematic literature review and meta-analysis. Osteoporos Int 32(8):1517–1530. https://doi.org/10.1007/s00198-021-05911-9 [published Online First: 20210407]
Aziziyeh R, Perlaza JG, Saleem N et al (2021) Benefits of fracture liaison services (FLS) in four Latin American countries: Brazil, Mexico, Colombia, and Argentina. J Med Econ 24(1):96–102. https://doi.org/10.1080/13696998.2020.1864920
Chang C-B, Yang R-S, Chang L-Y et al (2021) One-year outcomes of an osteoporosis liaison services program initiated within a healthcare system. Osteoporosis Int 32:2163–2172
Yan C, Chen Y, Cao J, Fang K, Shao L, Luo Y, Yang L (2023) The effectiveness of fracture liaison services in patients with hip fractures: a systematic review and meta-analysis of randomized controlled trials. Heliyon 9(10):e20838. https://doi.org/10.1016/j.heliyon.2023.e20838
Wu CH, Kao IJ, Hung WC et al (2018) Economic impact and cost-effectiveness of fracture liaison services: a systematic review of the literature. Osteoporos Int 29(6):1227–1242. https://doi.org/10.1007/s00198-018-4411-2 [published Online First: 20180219]
Thusini S, Milenova M, Nahabedian N et al (2022) Identifying and understanding benefits associated with return-on-investment from large-scale healthcare Quality Improvement programmes: an integrative systematic literature review. BMC Health Serv Res 22(1):1083. https://doi.org/10.1186/s12913-022-08171-3 [published Online First: 20220824]
Masters R, Anwar E, Collins B et al (2017) Return on investment of public health interventions: a systematic review. J Epidemiol Community Health 71(8):827–834. https://doi.org/10.1136/jech-2016-208141 [published Online First: 20170329]
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors) Cochrane handbook for systematic reviews of interventions version 6.4 (updated August 2023): Cochrane, 2023. Available from www.training.cochrane.org/handbook
Stone PW (2005) Return-on-investment models. Appl Nurs Res 18(3):186–189. https://doi.org/10.1016/j.apnr.2005.05.003
McIntosh E (2010) Applied methods of cost-benefit analysis in health care. Oxford University Press
Ganda K, Puech M, Chen J et al (2013) Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporosis Int 24:393–406
Beaupre LA, Lier D, Smith C et al (2020) A 3i hip fracture liaison service with nurse and physician co-management is cost-effective when implemented as a standard clinical program. Arch Osteoporos 15(1):113. https://doi.org/10.1007/s11657-020-00781-w [published Online First: 20200722]
Majumdar SR, Johnson JA, Lier DA et al (2007) Persistence, reproducibility, and cost-effectiveness of an intervention to improve the quality of osteoporosis care after a fracture of the wrist: results of a controlled trial. Osteoporos Int 18(3):261–270. https://doi.org/10.1007/s00198-006-0248-1 [published Online First: 20061104]
Majumdar SR, Lier DA, Beaupre LA et al (2009) Osteoporosis case manager for patients with hip fractures: results of a cost-effectiveness analysis conducted alongside a randomized trial. Arch Intern Med 169(1):25–31. https://doi.org/10.1001/archinte.169.1.25
Majumdar SR, Lier DA, Hanley DA et al (2017) Economic evaluation of a population-based osteoporosis intervention for outpatients with non-traumatic non-hip fractures: the "Catch a Break" 1i [type C] FLS. Osteoporos Int 28(6):1965–1977. https://doi.org/10.1007/s00198-017-3986-3 [published Online First: 20170309]
Majumdar SR, Lier DA, Leslie WD (2013) Cost-effectiveness of two inexpensive postfracture osteoporosis interventions: results of a randomized trial. J Clin Endocrinol Metab 98(5):1991–2000. https://doi.org/10.1210/jc.2013-1034 [published Online First: 20130417]
Majumdar SR, Lier DA, McAlister FA et al (2019) Cost-effectiveness of osteoporosis interventions to improve quality of care after upper extremity fracture: results from a randomized trial (C-STOP Trial). J Bone Miner Res 34(7):1220–1228. https://doi.org/10.1002/jbmr.3699 [published Online First: 20190318]
Majumdar SR, Lier DA, Rowe BH et al (2011) Cost-effectiveness of a multifaceted intervention to improve quality of osteoporosis care after wrist fracture. Osteoporos Int 22(6):1799–1808. https://doi.org/10.1007/s00198-010-1412-1 [published Online First: 20100929]
Saunders H, Sujic R, Bogoch ER et al (2021) Cost-utility analysis of the Ontario fracture screening and prevention program. J Bone Joint Surg Am 103(13):1175–1183. https://doi.org/10.2106/jbjs.20.00795
Senay A, Fernandes JC, Delisle J et al (2021) Patient healthcare trajectory and its impact on the cost-effectiveness of fracture liaison services. J Bone Miner Res 36(3):459–468. https://doi.org/10.1002/jbmr.4216 [published Online First: 20210123]
Yong JH, Masucci L, Hoch JS et al (2016) Cost-effectiveness of a fracture liaison service--a real-world evaluation after 6 years of service provision. Osteoporos Int 27(1):231–240. https://doi.org/10.1007/s00198-015-3280-1 [published Online First: 20150815]
Leal J, Gray AM, Hawley S et al (2017) Cost-effectiveness of orthogeriatric and fracture liaison service models of care for hip fracture patients: a population-based study. J Bone Miner Res 32(2):203–211. https://doi.org/10.1002/jbmr.2995 [published Online First: 20161101]
McLellan AR, Wolowacz SE, Zimovetz EA et al (2011) Fracture liaison services for the evaluation and management of patients with osteoporotic fracture: a cost-effectiveness evaluation based on data collected over 8 years of service provision. Osteoporos Int 22(7):2083–2098. https://doi.org/10.1007/s00198-011-1534-0 [published Online First: 20110524]
Nayak S, Singer A, Greenspan SL (2021) Cost-effectiveness of secondary fracture prevention intervention for Medicare beneficiaries. J Am Geriatr Soc 69(12):3435–3444. https://doi.org/10.1111/jgs.17381 [published Online First: 20210803]
Solomon DH, Patrick AR, Schousboe J et al (2014) The potential economic benefits of improved postfracture care: a cost-effectiveness analysis of a fracture liaison service in the US health-care system. J Bone Miner Res 29(7):1667–1674. https://doi.org/10.1002/jbmr.2180
Cooper MS, Palmer AJ, Seibel MJ (2012) Cost-effectiveness of the Concord Minimal Trauma Fracture Liaison service, a prospective, controlled fracture prevention study. Osteoporos Int 23(1):97–107. https://doi.org/10.1007/s00198-011-1802-z [published Online First: 20110928]
Li N, Si L, Boonen A et al (2022) A model-based cost-effectiveness analysis of fracture liaison services in China. Arch Osteoporos 17(1):132. https://doi.org/10.1007/s11657-022-01170-1 [published Online First: 20221005]
Naranjo A, Prieto-Alhambra D, Sánchez-Martín J et al (2022) Cost-effectiveness analysis of fracture liaison services compared with standard of care in the secondary prevention of fragility fractures in Spain. Clinicoecon Outcomes Res 14:249–264. https://doi.org/10.2147/ceor.S350790 [published Online First: 20220422]
Chien LN, Li YF, Yang RS et al (2022) Real-world cost-effectiveness analysis of the fracture liaison services model of care for hip fracture in Taiwan. J Formos Med Assoc 121(1 Pt 2):425–433. https://doi.org/10.1016/j.jfma.2021.05.028 [published Online First: 20210616]
Peng K, Yang M, Tian M et al (2020) Cost-effectiveness of a multidisciplinary co-management program for the older hip fracture patients in Beijing. Osteoporos Int 31(8):1545–1553. https://doi.org/10.1007/s00198-020-05393-1 [published Online First: 20200326]
Peters JL, Anderson R (2013) The cost-effectiveness of mandatory 20 mph zones for the prevention of injuries. J Public Health 35(1):40–48
Nichol KL (2001) Cost-benefit analysis of a strategy to vaccinate healthy working adults against influenza. Arch Int Med 161(5):749–759
Peng J, Liu Y, Chen L et al (2016) Bisphosphonates can prevent recurrent hip fracture and reduce the mortality in osteoporotic patient with hip fracture: a meta-analysis. Pak J Med Sci 32(2):499–504. https://doi.org/10.12669/pjms.322.9435
Saito T, Sterbenz JM, Malay S et al (2017) Effectiveness of anti-osteoporotic drugs to prevent secondary fragility fractures: systematic review and meta-analysis. Osteoporos Int 28(12):3289–3300. https://doi.org/10.1007/s00198-017-4175-0 [published Online First: 20170802]
Holzmueller CG, Karp S, Zeldow D et al (2016) Development of a cloud-based application for the Fracture Liaison Service model of care. Osteoporos Int 27(2):683–690. https://doi.org/10.1007/s00198-015-3260-5 [published Online First: 20150819]
Miller KL, Steffen MJ, McCoy KD et al (2021) Delivering fracture prevention services to rural US veterans through telemedicine: a process evaluation. Arch Osteoporos 16(1):27. https://doi.org/10.1007/s11657-021-00882-0 [published Online First: 20210210]
Wu CH, Chen CH, Chen PH et al (2018) Identifying characteristics of an effective fracture liaison service: systematic literature review. Osteoporos Int 29(5):1023–1047. https://doi.org/10.1007/s00198-017-4370-z [published Online First: 20180310]
Marsh D, Akesson K, Beaton DE et al (2011) Coordinator-based systems for secondary prevention in fragility fracture patients. Osteoporos Int 22(7):2051–2065. https://doi.org/10.1007/s00198-011-1642-x [published Online First: 20110524]
Zhou RA, Beaulieu ND, Cutler D (2020) Primary care quality and cost for privately insured patients in and out of US Health Systems: evidence from four states. Health Serv Res 55(Suppl 3(Suppl 3)):1098–1106. https://doi.org/10.1111/1475-6773.13590 [published Online First: 20201029]
Osaki M, Okuda R, Saeki Y et al (2021) Efficiency of coordinator-based osteoporosis intervention in fragility fracture patients: a prospective randomized trial. Osteoporos Int 32(3):495–503. https://doi.org/10.1007/s00198-021-05825-6 [published Online First: 20210123]
Kim SW, Won YJ, Chae DS et al (2019) A new Fracture Liaison Service using the mobile application and IoT sensor. Annu Int Conf IEEE Eng Med Biol Soc 2019:3486–3489. https://doi.org/10.1109/embc.2019.8857094
Deloumeau A, Moltó A, Roux C et al (2017) Determinants of short term fracture risk in patients with a recent history of low-trauma non-vertebral fracture. Bone 105:287–291. https://doi.org/10.1016/j.bone.2017.08.018 [published Online First: 20170824]
Robinson R (1993) Cost-benefit analysis. Bmj 307(6909):924–926. https://doi.org/10.1136/bmj.307.6909.924
Weaver CM, Bischoff-Ferrari HA, Shanahan CJ (2019) Cost-benefit analysis of calcium and vitamin D supplements. Arch Osteoporos 14(1):50. https://doi.org/10.1007/s11657-019-0589-y [published Online First: 20190430]
Cameron D, Ubels J, Norström F (2018) On what basis are medical cost-effectiveness thresholds set? Clashing opinions and an absence of data: a systematic review. Glob Health Action 11(1):1447828. https://doi.org/10.1080/16549716.2018.1447828
Wisløff T, Hagen G, Hamidi V et al (2014) Estimating QALY gains in applied studies: a review of cost-utility analyses published in 2010. Pharmacoeconomics 32:367–375
Funding
The study is funded by an MRFF grant (APP1176600). Lizheng Xu is supported by an Australian Government Research Training Program Scholarship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
For this type of study, formal consent is not required.
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, L., Zhao, T., Perry, L. et al. Return on investment of fracture liaison services: a systematic review and analysis. Osteoporos Int 35, 951–969 (2024). https://doi.org/10.1007/s00198-024-07027-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-024-07027-2