Abstract
Introduction and hypothesis
Sacrocolpopexy is considered mainstay treatment for apical or vaginal vault prolapse and is currently most often performed via a minimally invasive approach. Although mesh-related complications after this procedure are uncommon, mesh exposure can have an important impact on the patient’s quality of life. Our objective is to perform a literature review on this complication post laparoscopic or robotic sacrocolpopexy.
Methods
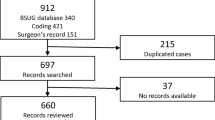
Web of Science and MEDLINE databases were searched for relevant articles published between 2005 and 2021. We retrieved 272 articles of which 83 ultimately were withheld.
Results
Minimally invasive sacrocolpopexy (MISC) implies a low risk of mesh exposure, which is currently estimated at 3.5%. Literature however is marked by substantial methodological heterogeneity. Controversy remains in the debate over prevention of mesh exposure after MISC. Performing a concomitant total hysterectomy is associated with an increased risk compared to subtotal hysterectomy or hysteropexy. Treatment of mesh exposure is challenging as guidelines are lacking. Although supported by few prospective data, patients with asymptomatic mesh exposure are managed conservatively. Surgical intervention, preferentially performed by an experienced pelvic surgeon, is indicated in symptomatic patients.
Conclusions
Mesh exposure is often undiagnosed and remains untreated. There is a gap in evidence exploring risk factors for mesh-related complications and efficient measures for reducing them. Choosing the best treatment option is still difficult. Management should be individualized and optimized at the time of diagnosis. Lack of acknowledgement and experience can result in increased morbidity.

Similar content being viewed by others
Abbreviations
- POP:
-
pelvic organ prolapse
- MISC:
-
minimally invasive sacrocolpopexy
- POP-Q:
-
Pelvic Organ Prolapse-Quantification
References
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with apical vaginal prolapse. Cochrane Database Syst Rev. 2016;10(10):CD012376. https://doi.org/10.1002/14651858.CD012376.
Gluck O, Blaganje M, Veit-Rubin N, Phillips C, Deprest J, O'Reilly B, But I, Moore R, Jeffery S, Haddad JM, Deval B. Laparoscopic sacrocolpopexy: a comprehensive literature review on current practice. Eur J Obstet Gynecol Reprod Biol. 2020;245:94–101.
Coolen AWM, Bui BN, Dietz V, Wang R, van Montfoort APA, Mol BWJ, Roovers JWR, Bongers MY. The treatment of post-hysterectomy vaginal vault prolapse: a systematic review and meta-analysis. Int Urogynecol J. 2017;28(12):1767–83. https://doi.org/10.1007/s00192-017-3493-2.
Haylen BT, Freeman RM, Swift SE, Cosson M, Davila GW, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) & grafts in female pelvic floor surgery. Int Urogynecol J. 2011;22:3–15. https://doi.org/10.1007/s00192-010-1324-9.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Marjoribanks J (2016) Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. (2):CD012079. https://doi.org/10.1002/14651858.CD012079.
Glazener CM, Breeman S, Elders A, Hemming C, Cooper KG, Freeman RM, Smith AR, Reid F, Hagen S, Montgomery I, Kilonzo M, Boyers D, McDonald A, McPherson G, MacLennan G, Norrie J (2017) PROSPECT study group). Mesh, graft, or standard repair for women having primary transvaginal anterior or posterior compartment prolapse surgery: two parallel-group, multicentre, randomised, controlled trials (PROSPECT). Lancet 389(10067):381-392. https://doi.org/10.1016/S0140-6736(16)31596-3.
US Food and Drug Administration. Update on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse: FDA safety communication. July, 2011. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm
Bergersen A, Hinkel C, Funk J, Twiss CO. Management of vaginal mesh exposure: a systematic review. Arab J Urol. 2019;17(1):40–8. https://doi.org/10.1080/2090598X.2019.1589787.
Kisby CK, Linder BJ. Management of vaginal mesh exposures following female pelvic reconstructive surgery. Curr Urol Rep. 2020;21(12):57. https://doi.org/10.1007/s11934-020-01002-0.
Developed by the Joint Writing Group of the American Urogynecologic Society and the International Urogynecological Association. Joint position statement on the management of mesh-related complications for the FPMRS specialist. Int Urogynecol J. 2020;31(4):679–94. https://doi.org/10.1097/SPV.0000000000000853.
Myers EM, Siff L, Osmundsen B, Geller E, Matthews CA. Differences in recurrent prolapse at 1 year after total vs supracervical hysterectomy and robotic sacrocolpopexy. Int Urogynecol J. 2015;26(4):585–9. https://doi.org/10.1007/s00192-014-2551-2.
Matthews CA, Geller EJ, Henley BR, Kenton K, Myers EM, Dieter AA, Parnell B, Lewicky-Gaupp C, Mueller MG, Wu JM. Permanent compared with absorbable suture for vaginal mesh fixation during total hysterectomy and sacrocolpopexy: a randomized controlled trial. Obstet Gynecol. 2020;136(2):355–64. https://doi.org/10.1097/AOG.0000000000003884.
Tagliaferri V, Ruggieri S, Taccaliti C, Gentile C, Didonna T, D'asta M, Legge F, Guida P, Scambia G, Guido M (2020) Comparison of absorbable and permanent sutures for laparoscopic sacrocervicopexy: A randomized controlled trial Acta Obstet Gynecol Scand 24. https://doi.org/10.1111/aogs.13997.
Culligan PJ, Lewis C, Priestley J, Mushonga N. Long-term outcomes of robotic-assisted laparoscopic sacrocolpopexy using lightweight Y-mesh. Female Pelvic Med Reconstr Surg. 2020;26(3):202–6. https://doi.org/10.1097/SPV.0000000000000788.
Dwyer L, Kumakech W, Ward K, Reid F, Smith A. Laparoscopic sacrocolpopexy (LSCP) using an ultra-lightweight polypropylene mesh. Eur J Obstet Gynecol Reprod Biol X. 2019;2:100008. https://doi.org/10.1016/j.eurox.2019.100008.
van Zanten F, van Iersel JJ, Paulides TJC, Verheijen PM, Broeders IAMJ, Consten ECJ, Lenters E, Schraffordt Koops SE. Long-term mesh erosion rate following abdominal robotic reconstructive pelvic floor surgery: a prospective study and overview of the literature. Int Urogynecol J. 2020;31(7):1423–33. https://doi.org/10.1007/s00192-019-03990-1.
Thomas TN, Davidson ERW, Lampert EJ, Paraiso MFR, Ferrando CA. Long-term pelvic organ prolapse recurrence and mesh exposure following sacrocolpopexy. Int Urogynecol J. 2020;31(9):1763–70. https://doi.org/10.1007/s00192-020-04291-8.
Li YL, Chang YW, Yang TH, Wu LY, Chuang FC, Kung FT, Huang KH. Mesh-related complications in single-incision transvaginal mesh (TVM) and laparoscopic abdominal sacrocolpopexy (LASC). Taiwan J Obstet Gynecol. 2020;59(1):43–50. https://doi.org/10.1016/j.tjog.2019.11.006.
van Zanten F, van Iersel JJ, Hartog FE, Aalders KIM, Lenters E, Broeders IAMJ, Schraffordt Koops SE. Mesh exposure after robot-assisted laparoscopic pelvic floor surgery: a prospective cohort study. J Minim Invasive Gynecol. 2019;26(4):636–42. https://doi.org/10.1016/j.jmig.2018.06.015.
Zebede S, Dawood A, Alarab M, Drutz H, Lovatsis D. A streamlined surgical approach to laparoscopic sacrocolpopexy for post-hysterectomy vault prolapse. J Obstet Gynaecol Can. 2016;38(5):446–52. https://doi.org/10.1016/j.jogc.2016.01.006.
Orhan A, Ozerkan K, Vuruskan H, Ocakoglu G, Kasapoglu I, Koşan B, Uncu G. Long-term follow-up of laparoscopic sacrocolpopexy: comparison of two different techniques used in urology and gynecology. Int Urogynecol J. 2019;30(4):623–32. https://doi.org/10.1007/s00192-018-03858-w.
Tan-Kim J, Nager CW, Grimes CL, Luber KM, Lukacz ES, Brown HW, Ferrante KL, Dyer KY, Kirby AC, Menefee SA. A randomized trial of vaginal mesh attachment techniques for minimally invasive sacrocolpopexy. Int Urogynecol J. 2015;26(5):649–56. https://doi.org/10.1007/s00192-014-2566-8.
Illiano E, Ditonno P, Giannitsas K, De Rienzo G, Bini V, Costantini E. Robot-assisted vs laparoscopic sacrocolpopexy for high-stage pelvic organ prolapse: a prospective, randomized, single-center study. Urology. 2019;34:116–23. https://doi.org/10.1016/j.urology.2019.07.043.
Kenton K, Mueller ER, Tarney C, Bresee C, Anger JT. One-year outcomes after minimally invasive sacrocolpopexy. Female Pelvic Med Reconstr Surg. 2016;22(5):382–4. https://doi.org/10.1097/SPV.0000000000000300.
Gupta P, Ehlert M, Bartley J, Gilleran J, Killinger KA, Boura JA, Nagaraju P, Fischer M. Perioperative outcomes, complications, and efficacy of robotic-assisted prolapse repair: a single institution study of 196 patients. Female Pelvic Med Reconstr Surg. 2018;24(6):408–11. https://doi.org/10.1097/SPV.0000000000000472.
El Hamamsy D, Fayyad AM. New onset stress urinary incontinence following laparoscopic sacrocolpopexy and its relation to anatomical outcomes. Int Urogynecol J. 2015;26(7):1041–5. https://doi.org/10.1007/s00192-015-2641-9.
Vieillefosse S, Thubert T, Dache A, Hermieu JF, Deffieux X. Satisfaction, quality of life and lumbar pain following laparoscopic sacrocolpopexy: suture vs. tackers. Eur J Obstet Gynecol Reprod Biol. 2015;187:51–6. https://doi.org/10.1016/j.ejogrb.2015.02.014.
Costantini E, Mearini L, Lazzeri M, Bini V, Nunzi E, di Biase M, Porena M. Laparoscopic versus abdominal sacrocolpopexy: a randomized, controlled trial. J Urol. 2016;196(1):159–65. https://doi.org/10.1016/j.juro.2015.12.089.
Pan K, Cao L, Ryan NA, Wang Y, Xu H. Laparoscopic sacral hysteropexy versus laparoscopic sacrocolpopexy with hysterectomy for pelvic organ prolapse. Int Urogynecol J. 2016;27(1):93–101. https://doi.org/10.1007/s00192-015-2775-9.
Chen Y, Hua K. Medium-term outcomes of laparoscopic sacrocolpopexy or sacrohysteropexy versus vaginal sacrospinous ligament fixation for middle compartment prolapse. Int J Gynaecol Obstet. 2017;137(2):164–9. https://doi.org/10.1002/ijgo.12097.
Linder BJ, Chow GK, Elliott DS. Long-term quality of life outcomes and retreatment rates after robotic sacrocolpopexy. Int J Urol. 2015;22(12):1155–8. https://doi.org/10.1111/iju.12900.
Linder BJ, Anand M, Klingele CJ, Trabuco EC, Gebhart JB, Occhino JA. Outcomes of robotic sacrocolpopexy using only absorbable suture for mesh fixation. Female Pelvic Med Reconstr Surg. 2017;23(1):13–6. https://doi.org/10.1097/SPV.0000000000000326.
Campagna G, Pedone Anchora L, Panico G, Caramazza D, Arcieri M, Cervigni M, Scambia G, Ercoli A. Titanized polypropylene mesh in laparoscopic sacral colpopexy. Int Urogynecol J. 2020;31(4):763–8. https://doi.org/10.1007/s00192-019-04146-x.
Matanes E, Boulus S, Lauterbach R, Amit A, Weiner Z, Lowenstein L (2020) Robotic laparoendoscopic single-site compared with robotic multi-port sacrocolpopexy for apical compartment prolapse. Am J Obstet Gynecol. 222(4):358.e1-358.e11. https://doi.org/10.1016/j.ajog.2019.09.048.
Nightingale G, Phillips C. Long-term safety and efficacy of laparoscopically placed mesh for apical prolapse. Int Urogynecol J. 2021;32(4):871–7. https://doi.org/10.1007/s00192-020-04374-6.
Illiano E, Giannitsas K, Costantini E. Comparison between laparoscopic sacrocolpopexy with hysterectomy and hysteropexy in advanced urogenital prolapse. Int Urogynecol J. 2020;31(10):2069–74. https://doi.org/10.1007/s00192-020-04260-1.
Pacquée S, Nawapun K, Claerhout F, Werbrouck E, Veldman J, Dʼhoore A, Wyndaele J, Verguts J, De Ridder D, Deprest J. Long-term assessment of a prospective cohort of patients undergoing laparoscopic sacrocolpopexy. Obstet Gynecol. 2019;134(2):323–32. https://doi.org/10.1097/AOG.0000000000003380.
Giugale LE, Hansbarger MM, Askew AL, Visco AG, Shepherd JP, Bradley MS. Assessing pelvic organ prolapse recurrence after minimally invasive sacrocolpopexy: does mesh weight matter? Int Urogynecol J. 2021. https://doi.org/10.1007/s00192-021-04681-6.
Kemp MM, Slim K, Rabischong B, Bourdel N, Canis M, Botchorishvili R. Transrectal mesh erosion requiring bowel resection. J Minim Invasive Gynecol. 2017;24(5):717–21. https://doi.org/10.1016/j.jmig.2017.01.002.
Moulder JK, Cohen SL, Morse AN, Einarsson JI. Mesh extrusion through the internal cervical os: an unusual complication following laparoscopic sacrocervicopexy. Female Pelvic Med Reconstr Surg. 2013;19(5):309–11. https://doi.org/10.1097/SPV.0b013e318292eb6d.
Mickelson L, Miklos JR, Moore RD. Laparoscopic repair of enterocervical fistula after mesh erosion into the sigmoid colon and cervix after robotic supracervical hysterectomy and sacrocervicopexy. Female Pelvic Med Reconstr Surg. 2016;22(1):e3–5. https://doi.org/10.1097/SPV.0000000000000211.
Shah HN, Badlani GH. Mesh complications in female pelvic floor reconstructive surgery and their management: a systematic review. Indian J Urol. 2012;28(2):129–53. https://doi.org/10.4103/0970-1591.98453.
Bedford ND, Seman EI, O'Shea RT, Keirse MJ. Effect of uterine preservation on outcome of laparoscopic uterosacral suspension. J Minim Invasive Gynecol. 2013;20(2):172–7. https://doi.org/10.1016/j.jmig.2012.10.014.
Jefferis H, Price N, Jackson S. Laparoscopic hysteropexy: 10 years' experience. Int Urogynecol J. 2017;28(8):1241–8. https://doi.org/10.1007/s00192-016-3257-4.
Kupelian AS, Vashisht A, Sambandan N, Cutner A. Laparoscopic wrap round mesh sacrohysteropexy for the management of apical prolapse. Int Urogynecol J. 2016;27(12):1889–97. https://doi.org/10.1007/s00192-016-3054-0.
Rahmanou P, Price N, Jackson SR. Laparoscopic hysteropexy versus vaginal hysterectomy for the treatment of uterovaginal prolapse: a prospective randomized pilot study. Int Urogynecol J. 2015;26:1687–94.
Rahmanou P, Price N, Jackson SR. Laparoscopic hysteropexy: a novel technique for uterine preservation surgery. Int Urogynecol J. 2014;25(1):139–40.
Price N, Slack A, Jackson SR. Laparoscopic hysteropexy: the initial results of a uterine suspension procedure for uterovaginal prolapse. BJOG Int J Obstet Gynaecol. 2010;17(1):62–6813.
Rahmanou P, White B, Price N, Jackson S. Laparoscopic hysteropexy: 1- to 4-year follow-up of women postoperatively. Int Urogynecol J. 2014;25(1):131–8.
Gutman RE, Rardin CR, Sokol ER, Matthews C, Park AJ, Iglesia CB, Geoffrion R, Sokol AI, Karram M, Cundiff GW, Blomquist JL, Barber MD (2017) Vaginal and laparoscopic mesh hysteropexy for uterovaginal prolapse: a parallel cohort study. Am J Obstet Gynecol. 216(1):38.e1-38.e11. https://doi.org/10.1016/j.ajog.2016.08.035.
Warembourg S, Labaki M, de Tayrac R, Costa P, Fatton B. Reoperations for mesh-related complications after pelvic organ prolapse repair: 8-year experience at a tertiary referral center. Int Urogynecol J. 2017;28(8):1139–51. https://doi.org/10.1007/s00192-016-3256-5.
Izett-Kay ML, Aldabeeb D, Kupelian AS, Cartwright R, Cutner AS, Jackson S, Price N, Vashisht A. Long-term mesh complications and reoperation after laparoscopic mesh sacrohysteropexy: a cross-sectional study. Int Urogynecol J. 2020;31(12):2595–602.
Sanverdi İ, Kılıççı Ç, Polat M, Özkaya E, Kılıç SG, Dizdar M, Karateke A. A new operation technique for uterine prolapse: vaginally-assisted laparoscopic sacrohysteropexy. Turk J Obstet Gynecol. 2017;14(3):181–6.
de Tayrac R, Sentilhes L. Complications of pelvic organ prolapse surgery and methods of prevention. Int Urogynecol J. 2013;24(11):1859–72. https://doi.org/10.1007/s00192-013-2177-9.
Warner WB, Vora S, Hurtado EA, Welgoss JA, Horbach NS, von Pechmann WS. Effect of operative technique on mesh exposure in laparoscopic sacrocolpopexy. Female Pelvic Med Reconstr Surg. 2012;18(2):113–7. https://doi.org/10.1097/SPV.0b013e318249bd54.
Osmundsen BC, Clark A, Goldsmith C, Adams K, Denman MA, Edwards R, Gregory WT. Mesh erosion in robotic sacrocolpopexy. Female Pelvic Med Reconstr Surg. 2012;18(2):86–8. https://doi.org/10.1097/SPV.0b013e318246806d.
Campagna G, Vacca L, Panico G, Rumolo V, Caramazza D, Lombisani A, Rossitto C, Gadonneix P, Scambia G, Ercoli A. Laparoscopic sacral hysteropexy versus laparoscopic sacral colpopexy plus supracervical hysterectomy in patients with pelvic organ prolapse. Int Urogynecol J. 2021. https://doi.org/10.1007/s00192-021-04865-0.
Li PC, Ding DC. Outcomes of laparoscopic hysteropexy and supracervical hysterectomy plus cervicopexy: a retrospective study. Ci Ji Yi Xue Za Zhi. 2019;32(3):262–6. https://doi.org/10.4103/tcmj.tcmj_131_19.
Gracia M, Perelló M, Bataller E, Espuña M, Parellada M, Genís D, Balasch J, Carmona F. Comparison between laparoscopic sacral hysteropexy and subtotal hysterectomy plus cervicopexy in pelvic organ prolapse: a pilot study. Neurourol Urodyn. 2015;34(7):654–8. https://doi.org/10.1002/nau.22641.
Stepanian AA, Miklos JR, Moore RD, Mattox TF. Risk of mesh extrusion and other mesh-related complications after laparoscopic sacral colpopexy with or without concurrent laparoscopic-assisted vaginal hysterectomy: experience of 402 patients. J Minim Invasive Gynecol. 2008;15(2):188–96. https://doi.org/10.1016/j.jmig.2007.11.006.
Dubinskaya A, Hernandez-Aranda D, Wakefield DB, Shepherd JP. Comparing laparoscopic and robotic sacrocolpopexy surgical outcomes with prior versus concomitant hysterectomy. Int Urogynecol J. 2020;31(2):401–7. https://doi.org/10.1007/s00192-019-04017-5.
Berger AA, Tan-Kim J, Menefee SA (2020) Anchor vs suture for the attachment of vaginal mesh in a robotic-assisted sacrocolpopexy: a randomized clinical trial. Am J Obstet Gynecol. 223(2):258.e1-258.e8. https://doi.org/10.1016/j.ajog.2020.05.018
Nolfi AL, Brown BN, Liang R, Palcsey SL, Bonidie MJ, Abramowitch SD, Moalli PA (2016) Host response to synthetic mesh in women with mesh complications. Am J Obstet Gynecol. 215(2):206.e1-8. https://doi.org/10.1016/j.ajog.2016.04.008.
Orenstein SB, Saberski ER, Kreutzer DL, Novitsky YW. Comparative analysis of histopathologic effects of synthetic meshes based on material, weight, and pore size in mice. J Surg Res. 2012;176(2):423–9. https://doi.org/10.1016/j.jss.2011.09.031.
Cundiff GW, Varner E, Visco AG, Zyczynski HM, Nager CW, Norton PA, Schaffer J, Brown MB, Brubaker L; Pelvic Floor Disorders Network (2008) Risk factors for mesh/suture erosion following sacral colpopexy. Am J Obstet Gynecol. 199(6):688.e1-5. https://doi.org/10.1016/j.ajog.2008.07.029
Askew AL, Visco AG, Weidner AC, Truong T, Siddiqui NY, Bradley MS. Does mesh weight affect time to failure after robotic-assisted laparoscopic sacrocolpopexy? Female Pelvic Med Reconstr Surg. 2020;26(9):536–40. https://doi.org/10.1097/SPV.0000000000000632.
Liang R, Knight K, Abramowitch S, Moalli PA. Exploring the basic science of prolapse meshes. Curr Opin Obstet Gynecol. 2016;28(5):413–9. https://doi.org/10.1097/GCO.0000000000000313.
Feola A, Barone W, Moalli P, Abramowitch S. Characterizing the ex vivo textile and structural properties of synthetic prolapse mesh products. Int Urogynecol J. 2013;24(4):559–64. https://doi.org/10.1007/s00192-012-1901-1.
Sindhwani N, Liaquat Z, Urbankova I, Vande Velde G, Feola A, Deprest J. Immediate postoperative changes in synthetic meshes—in vivo measurements. J Mech Behav Biomed Mater. 2015;55:228–35. https://doi.org/10.1016/j.jmbbm.2015.10.015.
Endo M, Feola A, Sindhwani N, Manodoro S, Vlacil J, Engels AC, Claus F, Deprest JA. Mesh contraction: in vivo documentation of changes in apparent surface area utilizing meshes visible on magnetic resonance imaging in the rabbit abdominal wall model. Int Urogynecol J. 2014;25(6):737–43. https://doi.org/10.1007/s00192-013-2293-6.
Sindhwani N, Callewaert G, Deprest T, Housmans S, Van Beckevoort D, Deprest J. Short term post-operative morphing of sacrocolpopexy mesh measured by magnetic resonance imaging. J Mech Behav Biomed Mater. 2018;80:269–76. https://doi.org/10.1016/j.jmbbm.2018.02.012.
Eisenberg VH, Steinberg M, Weiner Z, Alcalay M, Itskovitz-Eldor J, Schiff E, Lowenstein L. Three-dimensional transperineal ultrasound for imaging mesh implants following sacrocolpopexy. Ultrasound Obstet Gynecol. 2014;43(4):459–65. https://doi.org/10.1002/uog.13303.
Eisenberg VH, Steinberg M, Weiner Z, Schiff E, Lowenstein L. Long-term follow-up of sacrocolpopexy mesh implants at two time intervals at least 1 year apart using 4D transperineal ultrasound. Ultrasound Obstet Gynecol. 2017;49(3):398–403. https://doi.org/10.1002/uog.15891.
Tennyson L, Rytel M, Palcsey S, Meyn L, Liang R, Moalli P (2019) Characterization of the T-cell response to polypropylene mesh in women with complications. Am J Obstet Gynecol. 220(2):187.e1-187.e8. https://doi.org/10.1016/j.ajog.2018.11.121.
Committee Opinion No. 694. Management of mesh and graft complications in gynecologic surgery. Obstet Gynecol. 2017;129(4):e102–8.
Wong KS, Nguyen JN, White T, Menefee SA, Walter AJ, Krulewitch CJ, Anderson-Smits CT, Jakus-Waldman SM. Adverse events associated with pelvic organ prolapse surgeries that use implants. Obstet Gynecol. 2013;122(6):1239–45. https://doi.org/10.1097/AOG.0000000000000008.
Hart SR, Weiser EB. Abdominal sacral colpopexy mesh erosion resulting in a sinus tract formation and sacral abscess. Obstet Gynecol. 2004;103(5 Pt 2):1037–40. https://doi.org/10.1097/01.AOG.0000121829.55491.0d.
Taylor GB, Moore RD, Miklos JR. Osteomyelitis secondary to sacral colpopexy mesh erosion requiring laminectomy. Obstet Gynecol. 2006;107(2 Pt 2):475–7. https://doi.org/10.1097/01.AOG.0000187949.87223.06.
Grimes CL, Tan-Kim J, Garfin SR. Nager CW (2012) sacral colpopexy followed by refractory Candida albicans osteomyelitis and discitis requiring extensive spinal surgery. Obstet Gynecol. 2012 Aug;120(2 Pt 2):464–8. https://doi.org/10.1097/AOG.0b013e318256989e.
Abbott S, Unger CA, Evans JM, Jallad K, Mishra K, Karram MM, Iglesia CB, Rardin CR, Barber MD (2014) Evaluation and management of complications from synthetic mesh after pelvic reconstructive surgery: a multicenter study. Am J Obstet Gynecol. 210(2):163.e1-8. https://doi.org/10.1016/j.ajog.2013.10.012.
Arsene E, Giraudet G, Lucot JP, Rubod C, Cosson M. Sacral colpopexy: long-term mesh complications requiring reoperation(s). Int Urogynecol J. 2015;26(3):353–8. https://doi.org/10.1007/s00192-014-2514-7.
Quiroz LH, Gutman RE, Fagan MJ, Cundiff GW. Partial colpocleisis for the treatment of sacrocolpopexy mesh erosions. Int Urogynecol J Pelvic Floor Dysfunct. 2008;9(2):261–6. https://doi.org/10.1007/s00192-007-0416-7.
Sassani JC, Ross JH, Lopa S, Handzel RM, Bradley MS, Bonidie M. Prolapse recurrence after sacrocolpopexy mesh removal: a retrospective cohort study. Female Pelvic Med Reconstr Surg. 2020;26(2):92–6. https://doi.org/10.1097/SPV.0000000000000816.
South MM, Foster RT, Webster GD, Weidner AC, Amundsen CL (2007) Surgical excision of eroded mesh after prior abdominal sacrocolpopexy. Am J Obstet Gynecol. 197(6):615.e1-5. https://doi.org/10.1016/j.ajog.2007.08.012.
Ganatra AM, Rozet F, Sanchez-Salas R, Barret E, Galiano M, Cathelineau X, Vallancien G. The current status of laparoscopic sacrocolpopexy: a review. Eur Urol. 2009;55(5):1089–103. https://doi.org/10.1016/j.eururo.2009.01.048.
Schachar JS, Matthews CA (2020) Robotic-assisted repair of pelvic organ prolapse: a scoping review of the literature. Transl Androl Urol. 9(2):959-970. https://doi.org/10.21037/tau.2019.10.02.
Nygaard I, Brubaker L, Zyczynski HM, Cundiff G, Richter H, Gantz M, Fine P, Menefee S, Ridgeway B, Visco A, Warren LK, Zhang M, Meikle S. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309(19):2016–24. https://doi.org/10.1001/jama.2013.4919.
Meriwether KV, Antosh DD, Olivera CK, Kim-Fine S, Balk EM, Murphy M, Grimes CL, Sleemi A, Singh R, Dieter AA, Crisp CC, Rahn DD (2018) Uterine preservation vs hysterectomy in pelvic organ prolapse surgery: a systematic review with meta-analysis and clinical practice guidelines. Am J Obstet Gynecol. 219(2):129-146.e2. https://doi.org/10.1016/j.ajog.2018.01.018.
Ko KJ, Lee KS. Current surgical management of pelvic organ prolapse: strategies for the improvement of surgical outcomes. Investig Clin Urol. 2019;60(6):413–24. https://doi.org/10.4111/icu.2019.60.6.413.
Author information
Authors and Affiliations
Contributions
Stephanie Deblaere: selection of relevant literature, manuscript writing/editing.
Jan Hauspy: selection of relevant literature, manuscript editing.
Karen Hansen: manuscript editing.
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest regarding the publication of this literature review.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Deblaere, S., Hauspy, J. & Hansen, K. Mesh exposure following minimally invasive sacrocolpopexy: a narrative review. Int Urogynecol J 33, 2713–2725 (2022). https://doi.org/10.1007/s00192-021-04998-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04998-2