Abstract
Introduction and hypothesis
The objective was to identify structural failure sites in rectocele by comparing women with and those without posterior vaginal wall prolapse and accessing their relative contribution to rectocele size based on stress MRI-based measurements.
Methods
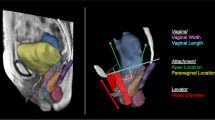
We studied three-dimensional stress MRI at maximal Valsalva of 25 women with (cases) and 25 without (controls) posterior vaginal prolapse of similar age and parity. Vaginal wall factors (posterior wall length and width); attachment factors (paravaginal posterior wall location, posterior fornix height, and perineal height); and hiatal factors (hiatal size and levator ani defects) were measured using Slicer 4.3.0® and a custom Python program. Stepwise linear regression was used to assess the relative contribution of all factors to the posterior prolapse size.
Results
We identified three primary factors with large effect sizes of 2 or greater: two attachment factors—posterior paravaginal descent and perineal height; and one hiatal factor—genital hiatus size. These were the strongest predictors of the presence and size of rectocele, the most common failure sites, found in 60–76% of cases; and highly correlated with one another (r = 0.72–0.84, p < .001). Longer vaginal length, wider distal vagina, lower posterior fornix, and larger levator ani hiatus had smaller effect sizes and were less likely to fall outside the norm (20–24%) than the three primary factors. When considering all the supporting factors, the combination of perineal height, posterior fornix height, and vaginal length explained 73% of the variation in rectocele size.
Conclusions
Lower perineal and lateral posterior vaginal location and enlarged genital hiatus size were strong predictors of rectocele occurrence and size and correlated highly.



Similar content being viewed by others
References
Hale DS, Fenner D. Consistently inconsistent, the posterior vaginal wall. Am J Obstet Gynecol. 2016;214(3):314–20. https://doi.org/10.1016/j.ajog.2015.09.001.
Jones HW III, Rock JA. Te Linde's operative gynecology. 11th ed. Philadelphia: Lippincott, Williams & Wilkins; 2015.
Walters M, Karram M. Urogynecology and reconstructive pelvic surgery. 4th ed. Philadelphia: Saunders; 2014.
Chen L, Lisse S, Larson K, Berger MB, Ashton-Miller JA, DeLancey JO. Structural failure sites in anterior vaginal wall prolapse: identification of a collinear triad. Obstet Gynecol. 2016;128(4):853–62. https://doi.org/10.1097/AOG.0000000000001652.
DeLancey JO. Structural anatomy of the posterior pelvic compartment as it relates to rectocele. Am J Obstet Gynecol. 1999;180(4):815–23.
Hsu Y, Lewicky-Gaupp C, DeLancey JO. Posterior compartment anatomy as seen in magnetic resonance imaging and 3-dimensional reconstruction from asymptomatic nulliparas. Am J Obstet Gynecol. 2008;198(6):651.e1-7.
Leffler KS, Thompson JR, Cundiff GW, Buller JL, Burrows LJ, Schon Ybarra MA. Attachment of the rectovaginal septum to the pelvic sidewall. Am J Obstet Gynecol. 2001;185(1):41–3. https://doi.org/10.1067/mob.2001.116366.
Brandon CJ, Lewicky-Gaupp C, Larson KA, Delancey JO. Anatomy of the perineal membrane as seen in magnetic resonance images of nulliparous women. Am J Obstet Gynecol. 2009;200(5):583.e1–6. https://doi.org/10.1016/j.ajog.2009.03.004.
Stein TA, DeLancey JO. Structure of the perineal membrane in females: gross and microscopic anatomy. Obstet Gynecol. 2008;111(3):686–93. https://doi.org/10.1097/AOG.0b013e318163a9a5.
Larson KA, Yousuf A, Lewicky-Gaupp C, Fenner DE, DeLancey JO. Perineal body anatomy in living women: 3-dimensional analysis using thin-slice magnetic resonance imaging. Am J Obstet Gynecol. 2010;203(5):494.e15–21.e21. https://doi.org/10.1016/j.ajog.2010.06.008.
Berger MB, Kolenic GE, Fenner DE, Morgan DM, DeLancey JOL. Structural, functional, and symptomatic differences between women with rectocele versus cystocele and normal support. Am J Obstet Gynecol. 2018;218(5):510.e1–8. https://doi.org/10.1016/j.ajog.2018.01.033.
Larson KA, Luo J, Guire KE, Chen L, Ashton-Miller JA, DeLancey JO. 3D analysis of cystoceles using magnetic resonance imaging assessing midline, paravaginal, and apical defects. Int Urogynecol J. 2012;23(3):285–93. https://doi.org/10.1007/s00192-011-1586-x.
Trowbridge ER, Fultz NH, Patel DA, DeLancey JO, Fenner DE. Distribution of pelvic organ support measures in a population-based sample of middle-aged, community-dwelling African American and white women in southeastern Michigan. Am J Obstet Gynecol. 2008;198(5):548.e1–6. https://doi.org/10.1016/j.ajog.2008.01.054.
Fialkow MF, Gardella C, Melville J, Lentz GM, Fenner DE. Posterior vaginal wall defects and their relation to measures of pelvic floor neuromuscular function and posterior compartment symptoms. Am J Obstet Gynecol. 2002;187(6):1443–8. https://doi.org/10.1067/mob.2002.129161. discussion 1448–1449.
Betschart C, Chen L, Ashton-Miller JA, Delancey JO. On pelvic reference lines and the MR evaluation of genital prolapse: a proposal for standardization using the Pelvic Inclination Correction System. Int Urogynecol J. 2013;24(9):1421–8. https://doi.org/10.1007/s00192-013-2100-4.
DeLancey JO, Morgan DM, Fenner DE, Kearney R, Guire K, Miller JM, Hussain H, Umek W, Hsu Y, Ashton-Miller JA. Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol. 2007;109(2 Pt 1):295–302. https://doi.org/10.1097/01.AOG.0000250901.57095.ba.
Xie B, Chen L, Xue Z, English EM, Fenner DE, Gaetke-Udager K, Kolenic GE, Ashton-Miller JA, DeLancey JO. Comparison of measurement systems for posterior vaginal wall prolapse on magnetic resonance imaging. Int Urogynecol J. 2019;30(8):1269–77. https://doi.org/10.1007/s00192-019-03939-4.
Lewicky-Gaupp C, Yousuf A, Larson KA, Fenner DE, Delancey JO. Structural position of the posterior vagina and pelvic floor in women with and without posterior vaginal prolapse. Am J Obstet Gynecol. 2010;202(5):497.e1–6. https://doi.org/10.1016/j.ajog.2010.01.001.
Spahlinger DM, Newcomb L, Ashton-Miller JA, DeLancey JO, Chen L. Relationship between intra-abdominal pressure and vaginal wall movements during Valsalva in women with and without pelvic organ prolapse: technique development and early observations. Int Urogynecol J. 2014;25(7):873–81. https://doi.org/10.1007/s00192-013-2298-1.
Sammarco AG, Nandikanti L, Kobernik EK, Xie B, Jankowski A, Swenson CW, DeLancey JOL. Interactions among pelvic organ protrusion, levator ani descent, and hiatal enlargement in women with and without prolapse. Am J Obstet Gynecol. 2017;217(5):614.e1–7. https://doi.org/10.1016/j.ajog.2017.07.007.
Luo J, Larson KA, Fenner DE, Ashton-Miller JA, DeLancey JO. Posterior vaginal prolapse shape and position changes at maximal Valsalva seen in 3-D MRI-based models. Int Urogynecol J. 2012;23(9):1301–6. https://doi.org/10.1007/s00192-012-1760-9.
Sutkin G, Zyczynski HM, Sridhar A, Jelovsek JE, Rardin CR, Mazloomdoost D, Rahn DD, Nguyen JN, Andy UU, Meyer I, Gantz MG, Network NPFD. Association between adjuvant posterior repair and success of native tissue apical suspension. Am J Obstet Gynecol. 2020;222(2):161.e1–8. https://doi.org/10.1016/j.ajog.2019.08.024.
Hsu Y, Chen L, Summers A, Ashton-Miller JA, DeLancey JO. Anterior vaginal wall length and degree of anterior compartment prolapse seen on dynamic MRI. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(1):137–42. https://doi.org/10.1007/s00192-007-0405-x.
Swenson CW, Simmen AM, Berger MB, Morgan DM, DeLancey JO. The long and short of it: anterior vaginal wall length before and after anterior repair. Int Urogynecol J. 2015;26(7):1035–9. https://doi.org/10.1007/s00192-015-2636-6.
Acknowledgements
The authors thank Sarah Block for assistance with manuscript preparation.
Funding
Supported by the National Institutes of Health, grants P50 HD044406 and R01 HD094954.
Author information
Authors and Affiliations
Contributions
L. Chen: Project development, Data collection, Data analysis, Manuscript writing; B. Xie: Data collection, Manuscript writing; D. Fenner: Project development, Manuscript writing; D. Thibault: Manuscript writing; J.A. Ashton-Miller: Project development, Data analysis; J.O.L. DeLancey: Project development, Data collection, Data analysis, Manuscript writing.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Appendices
Appendix 1
Posterior compartment anatomy and measurement strategy. a Conceptual framework of posterior wall support showing normal posterior wall support anatomy: vaginal wall, posterior fornix support, distal support for the perineal body, and the levator ani muscle. b The length and width of a normally supported posterior vaginal wall. c Illustration on how the paravaginal location in normal women changes in women with posterior vaginal prolapse. Arrowheads posterior arcus
Appendix 2
Rights and permissions
About this article
Cite this article
Chen, L., Xie, B., Fenner, D.E. et al. Structural failure sites in posterior vaginal wall prolapse: stress 3D MRI-based analysis. Int Urogynecol J 32, 1399–1407 (2021). https://doi.org/10.1007/s00192-021-04685-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04685-2