Abstract
Background
Pelvic floor disorders (PFDs), include urinary incontinence, overactive bladder, anal incontinence, and pelvic organ prolapse negatively affect physical, psychosocial, and economic wellbeing of women. In developing countries, less than a quarter of women with PFDs seek health care for their problem. Health care seeking for PFDs, and its associated factors, is little known in Ethiopia. This study aimed to assess health care seeking for PFDs, associated factors, and deterrents for seeking care.
Methods
From a community based cross sectional study conducted form August 10 to September 4, 2016 to assess pelvic floor disorders, seven hundred four participants with PFDs drawn for health care seeking behavior analysis. Data were collected through interviewed administered questionnaire. Poisson regression model with robust variance was used to investigate the association of the independent variable with health care seeking behaviors. The results are reported in crude and adjusted prevalence ratio with 95% confidence intervals.
Result
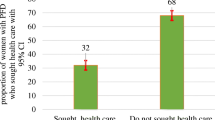
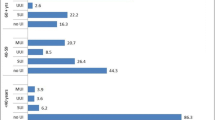
Two hundred twenty five (32%; CI: 26.8–35.5) women sought care for their PFDs. Majority 160 (71%) of them seek care from government health facilities. Middle wealth index Adjusted Prevalence Ratio (APR) = 1.4, CI: 1.1, 1.8), autonomous decision making on own health (APR = 1.3, CI: 1.1, 1.7), and sever impact of PFDs on quality of life (APR = 1.4, CI:1.1, 1.9) were identified as associated factors for health care seeking.
Conclusion
A large number of women with pelvic floor disorder did not seek health care: this calls for urgent and tailored intervention to enhance health care seeking behaviors of women with PFD.


Similar content being viewed by others
References
Doshani A, Teo REC, Mayne CJ, Tincello DG. Uterine prolapse. BMJ. 2007;335:819–23. https://doi.org/10.1136/bmj.39356.604074.BE.
Brækken IH (2010) Pelvic floor muscle function and Pelvic Organ Prolapse Dissertation from the Norwegian School of Sport Sciences; Oslo.
Lawrence JM, Lukacz ES, Nager CW, Hsu J-WY, Luber KM. Prevalence and co-occurrence of pelvic floor disorders in community-dwelling women. Obstet Gynecol. 2008;111:678–85.
Limpawattana P, Kongbunkiat K, Sawanyawisuth K, Sribenjalux W. Help-seeking behaviour for urinary incontinence: experience from a university community. Int J Urol Nurs. 2015;9(3):143–8. https://doi.org/10.1111/ijun.12065.
Pakgohar M, Sabetghadam S, Rahimparvar SFV, Kazemnejad A. Quality of life (QoL) and help-seeking in postmenopausal women with urinary incontinence (UI): a population based study. Arch Gerontol Geriatr. 2014;59:403–7.
Ian M, Karin SC, Sean N, Marion K, Chieh-I C, Alan JW. Global prevalence and economic burden of urgency urinary incontinence: a systematic review. Eur Urol. 2015;65:7 9–9 5. https://doi.org/10.1016/j.eururo.2013.08.031.
Isuzu M, Holly ER. Impact of fecal incontinence and its treatment on quality of life in women. Women's Health (Lond Engl). 2015;11(2):225–38. https://doi.org/10.2217/whe.14.66.
Morhason-Bello I, Adedokun, Ojengbede, Okonkwo, Kolade (2012) Help-seeking behavior among women currently leaking urine in Nigeria: is it any different from the rest of the world? Patient Prefer Adherence: 815. https://doi.org/10.2147/ppa.s24911.
Fritel X, Panjo H, Varnoux N, Ringa V. The individual determinants of care-seeking among middle-aged women reporting urinary incontinence: analysis of a 2273-woman cohort. Neurourol Urodyn. 2014;33(7):1116–22. https://doi.org/10.1002/nau.22461.
Kılıç M (2016) Incidence and risk factors of urinary incontinence in women visiting Family Health Centers. Springerplus. 5(1331). https://doi.org/10.1186/s40064-016-2965-z.
Gjerde JL, Rortveit G, Muleta M, Blystad A. Silently waiting to heal; experiences among women living with urinary incontinence in Northwest Ethiopia. Int Urogynecol J. 2013;24:953–8.
Gjerde JL, Rortveit G, Muleta M, Adefris M, Blystad A. Living with pelvic organ prolapse: voices of women from Amhara region, Ethiopia. Int Urogynecol J. 2017;28(3):361–6. https://doi.org/10.1007/s00192-016-3077-6.
Wu C, Sun T, Guan X, Wang K. Predicting delay to treatment of urinary incontinence among urban community-dwelling women in China. International Journal of Nursing Sciences. 2015;2(1):34–8. https://doi.org/10.1016/j.ijnss.2015.01.015.
Minassian VA, Yan X, Lichtenfeld MJ, Sun H, Stewart WF. The iceberg of health care utilization in women with urinary incontinence. Int Urogynecol J. 2012;23:1087–93.
Central Statistical Agency (2016) Ethiopian demographic Health Sruvillance https://www.usaid.gov/sites/default/files/documents/1860/EthiopiaDHS2016KIR-Final10-17-2016.pdf. Accessed 5 December, 2016.
Assefa N, Oljira L, Baraki N, Demena M, Zelalem D, Ashenafi W, et al. HDSS profile: the Kersa health and demographic surveillance system. Int J Epidemiol. 2016;45(1):94–101. https://doi.org/10.1093/ije/dyv284.
Dheresa M, Worku A, Oljira L, Mengiste B, Assefa N, Berhane Y (2018) One in five women suffer from pelvic floor disorders in Kersa district Eastern Ethiopia: a community-based study. BMC Women's Health. 18(95). https://doi.org/10.1186/s12905-018-0585-1.
Minassian VA, Yan X, Lichtenfeld MJ, Sun H, Stewart WF. Predictors of care seeking in women with urinary incontinence. Neurourol Urodyn. 2012;31:470–4.
Lukacz ES, Lawrence JM, Buckwalter JG, Burchette RJ, Nager CW, Luber KM. Epidemiology of prolapse and incontinence questionnaire: validation of a new epidemiologic survey. Int Urogynecol J. 2005;16:272–84.
Haylen BT, Dd R, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An international Urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26. https://doi.org/10.1007/s00192-009-0976-9.
Gyhagen M, Åkervall S, Milsom I. Clustering of pelvic floor disorders 20 years after one vaginal or one cesarean birth. Int Urogynecol J. 2015;26:1115–21.
Ethiopian Centeral statistics Agency. ETHIOPIA demographic and health survey 2016. Rockville: Key Indicators Report; 2016.
Central Statistical Agency, ICF International. Ethiopia demographic and health survey 2011 central statistical agency and ICF international. Ethiopia and Calverton: Addis Ababa; 2012.
Nosti PA, McDermott CD, Stehman FB, Schilder JM, Woodman PJ. Symptoms of pelvic floor disorders and quality of life measures in postoperative patients WithEndometrial Cancer. Clinical Ovarian & Other Gynecologic Cancer. 2012;5(1):27–30.
Zeleke BM, Ayele TA, Woldetsadik MA, Bisetegn TA, Adane AA (2013) Depression among women with obstetric fistula, and pelvic organ prolapse in northwest Ethiopia. BMC Psychiatry. 13(236). https://doi.org/10.1186/1471-244X-13-236.
Hemachandra NN, Rajapaksa LC, Manderson L. A “usual occurrence:” stress incontinence among reproductive aged women in Sri Lanka. Soc Sci Med. 2009;69:1395–401.
Morrill M, Lukacz ES, Lawrence JM, Nager CW, Contreras R, Luber KM. Seeking healthcare for pelvic floor disorders: a population-based study. Am J Obstet Gynecol. 2007;197(1):86 e81–6. https://doi.org/10.1016/j.ajog.2007.02.051.
Xu D, Wang X, Li J, Wang K. The mediating effect of ‘bothersome’ urinary incontinence on help-seeking intentions among community-dwelling women. J Adv Nurs. 2015;71(2):315–25. https://doi.org/10.1111/jan.12514.
Ethiopian Minstry of Health (2016) Nationla Reproductive Health Strategy 2016–2020. Ethiopia, Addis Ababa.
Slavin SL, Rogers RG, Komesu Y, Omotosho T, Hammil S, Lewis C, et al. Complementary and alternative medicine (CAM) use in women with pelvic floor disorders: a cohort study. Int Urogynecol J. 2009;21(4):431–7. https://doi.org/10.1007/s00192-009-1058-8.
Sung VW, Raker CA, Myers DL, Clark MA. Treatment decision-making and information-seeking preferences in women with pelvic floor disorders. Int Urogynecol J. 2010;21(9):1071–8. https://doi.org/10.1007/s00192-010-1155-8.
Acknowledgements
We would like to acknowledged Haramaya University and Addis Continental Institute of Public health for their technical and financial support. We thankful to women who responded to this survey.
Funding
This study was financially supported by Haramaya University and Addis Continental Institute of Public Health.
Author information
Authors and Affiliations
Contributions
MD, AW, LO, BM, NA, and YB, contributed to the study design, MD, LO, BM and NA carried out the data collection. MD and AW lead the data analysis and MD, YB, AW, LO, BM and NA reviewed the various version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethics and consent
The study protocol was approved by Haramaya University Health and Medical Sciences College institutional health research ethics review committee. Written informed consent was obtained from each participant. In order to protect the confidentiality of the information, names and ID was not included in the written questionnaires.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dheresa, M., Worku, A., Oljira, L. et al. Women’s health seeking behavior for pelvic floor disorders and its associated factors in eastern Ethiopia. Int Urogynecol J 31, 1263–1271 (2020). https://doi.org/10.1007/s00192-020-04309-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04309-1