Abstract
Introduction and hypothesis
In interstitial cystitis/bladder pain syndrome (IC/BPS), pelvic floor dysfunction may contribute significantly to pelvic pain. To determine if pelvic floor hypertonicity manifests alterations on magnetic resonance imaging (MRI) in patients with IC/BPS, we retrospectively compared pelvic measurements between patients and controls.
Methods
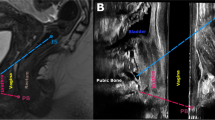
Fifteen women with IC/BPS and 15 age-matched controls underwent pelvic MRI. Two blinded radiologists measured the pelvic musculature, including the H- and M lines, vaginal length, urethral length and cross-sectional area, levator width and length, and posterior puborectalis angle. MRI measures and clinical factors, such as age, parity, and duration of symptoms, were compared using a paired, two-tailed t test.
Results
There were no significant differences in age, parity, or symptom duration between groups. Patients with IC/BPS exhibited shorter levator muscles (right: 5.0 ± 0.7 vs. 5.6 ± 0.8, left: 5.0 ± 0.8 vs. 5.7 ± 0.8 cm, P < 0.002) and a wider posterior puborectalis angle (35.0 ± 8.6 vs. 26.7 ± 7.9°, P < 0.01) compared with controls. The H line was shorter in patients with IC/BPS (7.8 ± 0.8 vs. 8.6 ± 0.9 cm, P < 0.02), while M line did not differ. Total urethral length was similar, but vaginal cuff and bladder neck distances to the H line were longer in patients with IC/BPS (5.7 ± 0.6 vs. 5.1 ± 0.9 cm, P < 0.02; 1.9 ± 0.4 vs. 1.4 ± 0.2 cm, P < 0.001, respectively).
Conclusions
Patients with IC/BPS have pelvic floor hypertonicity on MRI, which manifests as shortened levator, increased posterior puborectalis angles, and decreased puborectal distances. We identified evidence of pelvic floor hypertonicity in patients with IC/BPS, which may contribute to or amplify pelvic pain. Future studies are necessary to determine the MRI utility in understanding pelvic floor hypertonicity in patients with IC/BPS.



Similar content being viewed by others
Abbreviations
- AP:
-
Anteroposterior
- BMI:
-
Body mass index
- CCC:
-
Concordance class correlation
- IC/BPS:
-
Interstitial cystitis/bladder pain syndrome
- MRI:
-
Magnetic resonance imaging
- ROC:
-
Receiver operating characteristic
- SCAT:
-
Subcutaneous adipose tissue
- UPRL:
-
Urethral meatus to the puborectal line
References
Clemens JQ (2010) Afferent neurourology: a novel paradigm. Neurourol Urodyn 29(Suppl 1):S29–S31. doi:10.1002/nau.20792
Barsky AJ, Borus JF (1999) Functional somatic syndromes. Ann Intern Med 130(11):910–921
Butrick CW (2003) Interstitial cystitis and chronic pelvic pain: new insights in neuropathology, diagnosis, and treatment. Clin Obstet Gynecol 46(4):811–823
Peters KM, Carrico DJ, Diokno AC (2008) Characterization of a clinical cohort of 87 women with interstitial cystitis/painful bladder syndrome. Urology 71(4):634–640. doi:10.1016/j.urology.2007.11.013
Peters K, Girdler B, Carrico D, Ibrahim I, Diokno A (2008) Painful bladder syndrome/interstitial cystitis and vulvodynia: a clinical correlation. Int Urogynecol J Pelvic Floor Dysfunct 19(5):665–669. doi:10.1007/s00192-007-0501-y
Schmidt RA, Vapnek JM (1991) Pelvic floor behavior and interstitial cystitis. Semin Urol 9(2):154–159
Simons DG, Travell JG, Simons LS (1999) Travell & Simons’ myofascial pain and dysfunction: the trigger point manual, 2nd edn. Williams & Wilkins, Baltimore
Bassaly R, Tidwell N, Bertolino S, Hoyte L, Downes K, Hart S (2011) Myofascial pain and pelvic floor dysfunction in patients with interstitial cystitis. Int Urogynecol J 22(4):413–418. doi:10.1007/s00192-010-1301-3
Doggweiler-Wiygul R, Wiygul JP (2002) Interstitial cystitis, pelvic pain, and the relationship to myofascial pain and dysfunction: a report on four patients. World J Urol 20(5):310–314. doi:10.1007/s00345-002-0298-8
FitzGerald MP, Payne CK, Lukacz ES, Yang CC, Peters KM, Chai TC, Nickel JC, Hanno PM, Kreder KJ, Burks DA, Mayer R, Kotarinos R, Fortman C, Allen TM, Fraser L, Mason-Cover M, Furey C, Odabachian L, Sanfield A, Chu J, Huestis K, Tata GE, Dugan N, Sheth H, Bewyer K, Anaeme A, Newton K, Featherstone W, Halle-Podell R, Cen L, Landis JR, Propert KJ, Foster HE Jr, Kusek JW, Nyberg LM (2012) Randomized multicenter clinical trial of myofascial physical therapy in women with interstitial cystitis/painful bladder syndrome and pelvic floor tenderness. J Urol 187(6):2113–2118. doi:10.1016/j.juro.2012.01.123
Weiss JM (2001) Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome. J Urol 166(6):2226–2231
Gousse AE, Barbaric ZL, Safir MH, Madjar S, Marumoto AK, Raz S (2000) Dynamic half Fourier acquisition, single shot turbo spin-echo magnetic resonance imaging for evaluating the female pelvis. J Urol 164(5):1606–1613
Comiter CV, Vasavada SP, Barbaric ZL, Gousse AE, Raz S (1999) Grading pelvic prolapse and pelvic floor relaxation using dynamic magnetic resonance imaging. Urology 54(3):454–457
Pannu HK (2003) Dynamic MR imaging of female organ prolapse. Radiol Clin N Am 41(2):409–423
Singh K, Reid WM, Berger LA (2002) Magnetic resonance imaging of normal levator ani anatomy and function. Obstet Gynecol 99(3):433–438
Hsu Y, Summers A, Hussain HK, Guire KE, Delancey JO (2006) Levator plate angle in women with pelvic organ prolapse compared to women with normal support using dynamic MR imaging. Am J Obstet Gynecol 194(5):1427–1433. doi:10.1016/j.ajog.2006.01.055
Ansquer Y, Fernandez P, Chapron C, Frey C, Bennis M, Roy C, Salomon L, Mandelbrot L, Carbonne B (2006) Static and dynamic MRI features of the levator ani and correlation with severity of genital prolapse. Acta Obstet Gynecol Scand 85(12):1468–1475. doi:10.1080/00016340600984837
Ludescher B, Rommel M, Willmer T, Fritsche A, Schick F, Machann J (2011) Subcutaneous adipose tissue thickness in adults - correlation with BMI and recommendations for pen needle lengths for subcutaneous self-injection. Clin Endocrinol (Oxf) 75(6):786–790. doi:10.1111/j.1365-2265.2011.04132.x
Metz CE (1978) Basic principles of ROC analysis. Semin Nucl Med 8(4):283–298
Zweig MH, Campbell G (1993) Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem 39(4):561–577
Wessely S, Nimnuan C, Sharpe M (1999) Functional somatic syndromes: one or many? Lancet 354(9182):936–939. doi:10.1016/S0140-6736(98)08320-2
Tunn R, Delancey JO, Howard D, Ashton-Miller JA, Quint LE (2003) Anatomic variations in the levator ani muscle, endopelvic fascia, and urethra in nulliparas evaluated by magnetic resonance imaging. Am J Obstet Gynecol 188(1):116–121
Hsu Y, Chen L, Huebner M, Ashton-Miller JA, DeLancey JO (2006) Quantification of levator ani cross-sectional area differences between women with and those without prolapse. Obstet Gynecol 108(4):879–883. doi:10.1097/01.AOG.0000233153.75175.34
Nickel JC, Shoskes D, Irvine-Bird K (2009) Clinical phenotyping of women with interstitial cystitis/painful bladder syndrome: a key to classification and potentially improved management. J Urol 182(1):155–160. doi:10.1016/j.juro.2009.02.122
Fenton BW (2007) Limbic associated pelvic pain: a hypothesis to explain the diagnostic relationships and features of patients with chronic pelvic pain. Med Hypotheses 69(2):282–286. doi:10.1016/j.mehy.2006.12.025
Malykhina AP, Qin C, Greenwood-van Meerveld B, Foreman RD, Lupu F, Akbarali HI (2006) Hyperexcitability of convergent colon and bladder dorsal root ganglion neurons after colonic inflammation: mechanism for pelvic organ cross-talk. Neurogastroenterol Motil 18(10):936–948. doi:10.1111/j.1365-2982.2006.00807.x
Kaddumi EG, Hubscher CH (2007) Changes in rat brainstem responsiveness to somatovisceral inputs following acute bladder irritation. Exp Neurol 203(2):349–357. doi:10.1016/j.expneurol.2006.08.011
Rudick CN, Chen MC, Mongiu AK, Klumpp DJ (2007) Organ cross talk modulates pelvic pain. Am J Physiol Regul Integr Comp Physiol 293(3):R1191–R1198. doi:10.1152/ajpregu.00411.2007
Pezzone MA, Liang R, Fraser MO (2005) A model of neural cross-talk and irritation in the pelvis: implications for the overlap of chronic pelvic pain disorders. Gastroenterology 128(7):1953–1964
Kilpatrick LA, Kutch JJ, Tillisch K, Naliboff BD, Labus JS, Jiang Z, Farmer MA, Apkarian AV, Mackey S, Martucci KT, Clauw DJ, Harris RE, Deutsch G, Ness TJ, Yang CC, Maravilla K, Mullins C, Mayer EA (2014) Alterations in resting state oscillations and connectivity in sensory and motor networks in women with interstitial cystitis/painful bladder syndrome. J Urol 192(3):947–955. doi:10.1016/j.juro.2014.03.093
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ackerman, A.L., Lee, U.J., Jellison, F.C. et al. MRI suggests increased tonicity of the levator ani in women with interstitial cystitis/bladder pain syndrome. Int Urogynecol J 27, 77–83 (2016). https://doi.org/10.1007/s00192-015-2794-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2794-6