Abstract
Purpose
To evaluate studies utilizing orthobiologics in the management of femoroacetabular impingement syndrome (FAIS) to (1) assess the indications for usage, and (2) analyze patient-reported outcome measures (PROM) following treatment. It was hypothesized that orthobiologics would (1) be utilized for symptomatic FAIS in the setting of labral or chondral pathology, and (2) improve PROM at most recent follow-up.
Methods
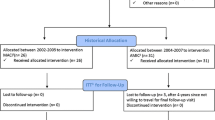
The Pubmed, Ovid Medline, Cochrane, and Web of Science databases were searched for clinical studies evaluating orthobiologics [hyaluronic acid (HA), platelet-rich plasma (PRP), or cell-based therapy (CBT) for treatment of FAIS. Exclusion criteria included orthobiologics used in conjunction with cartilage transfer or scaffolding procedures and a primary indication other than FAIS. Data collection included patient demographics, indications, and baseline and most recent PROM.
Results
Eleven studies (one level I, four level II, four level III, and two level IV evidence) met inclusion criteria, consisting of 440 patients with mean ages ranging from 32.8 to 47 years. All 11 studies demonstrated an improvement in PROM from baseline to most-recent follow-up. Four studies administered PRP either intraoperatively or the day after surgery as an adjunct to labral repair. CBT was used intraoperatively in the setting of acetabular chondral lesions (three studies) and labral repair (one study). When comparing to a control group at most recent follow-up, three PRP cohorts demonstrated similar PROM (n.s.), while one PRP group exhibited worse visual analog pain scores (2.5 vs. 3.4, p = 0.005) and modified Harris Hip Scores (mHHS) (82.6 vs. 78.7, p = 0.049). The four CBT studies reported favorable results compared to a control group, with a significantly higher mHHS at most recent follow-up or mean improvement from baseline in Hip Outcome Score–Activities of Daily Living (p < 0.05). Three studies reported on HA, which was utilized exclusively in the nonoperative setting.
Conclusions
Intraoperative PRP and CBT have been commonly reported in the setting of hip arthroscopy for labral repairs and acetabular chondral lesions, respectively. The CBT cohorts demonstrated more favorable PROM at most recent follow-up when compared to a control group, though these results should be interpreted with caution due to heterogeneity of orthobiologic preparations.
Level of evidence
IV.

Similar content being viewed by others
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Abate M, Scuccimarra T, Vanni D, Pantalone A, Salini V (2014) Femoroacetabular impingement: is hyaluronic acid effective? Knee Surg Sports Traumatol Arthrosc 22(4):889–892
Abrams GD, Frank RM, Fortier LA, Cole BJ (2013) Platelet-rich plasma for articular cartilage repair. Sports Med Arthrosc Rev 21(4):213–219
Abrams GD, Murray IR (2020) Editorial commentary: please don’t call it a mesenchymal stem cell. Arthroscopy 36(8):2134–2136
Altman R, Bedi A, Manjoo A, Niazi F, Shaw P, Mease P (2019) Anti-inflammatory effects of intra-articular hyaluronic acid: a systematic review. Cartilage 10(1):43–52
Anz AW, Hackel JG, Nilssen EC, Andrews JR (2014) Application of biologics in the treatment of the rotator cuff, meniscus, cartilage, and osteoarthritis. J Am Acad Orthop Surg 22(2):68–79
Bennell KL, Paterson KL, Metcalf BR, Duong V, Eyles J, Kasza J, Wang Y, Cicuttini F, Buchbinder R, Forbes A, Harris A, Yu SP, Connell D, Linklater J, Wang BH, Oo WM, Hunter DJ (2021) Effect of intra-articular platelet-rich plasma vs placebo injection on pain and medial tibial cartilage volume in patients with knee osteoarthritis: the RESTORE randomized clinical trial. JAMA 326(20):2021–2030
Berney M, McCarroll P, Glynn L, Lenehan B (2021) Platelet-rich plasma injections for hip osteoarthritis: a review of the evidence. Ir J Med Sci 190(3):1021–1025
Cavinatto L, Hinckel BB, Tomlinson RE, Gupta S, Farr J, Bartolozzi AR (2019) The role of bone marrow aspirate concentrate for the treatment of focal chondral lesions of the knee: a systematic review and critical analysis of animal and clinical studies. Arthroscopy 35(6):1860–1877
Cole BJ, Karas V, Hussey K, Pilz K, Fortier LA (2017) Hyaluronic acid versus platelet-rich plasma: a prospective, double-blind randomized controlled trial comparing clinical outcomes and effects on intra-articular biology for the treatment of knee osteoarthritis. Am J Sports Med 45(2):339–346
Condron NB, Kester BS, Tokish JM, Zumstein MA, Gobezie R, Scheibel M, Cole BJ (2021) Nonoperative and operative soft-tissue, cartilage, and bony regeneration and orthopaedic biologics of the shoulder: an orthoregeneration network (ON) foundation review. Arthroscopy 37(10):3200–3218
Cotter EJ, Wang KC, Yanke AB, Chubinskaya S (2018) Bone marrow aspirate concentrate for cartilage defects of the knee: from bench to bedside evidence. Cartilage 9(2):161–170
DeLong JM, Russell RP, Mazzocca AD (2012) Platelet-rich plasma: the PAW classification system. Arthroscopy 28(7):998–1009
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini FC, Krause DS, Deans RJ, Keating A, Prockop DJ, Horwitz EM (2006) Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 8(4):315–317
Fice MP, Miller JC, Christian R, Hannon CP, Smyth N, Murawski CD, Cole BJ, Kennedy JG (2019) The role of platelet-rich plasma in cartilage pathology: an updated systematic review of the basic science evidence. Arthroscopy 35(3):961-976.e3
Foo GL, Knudsen JS, Bacon CJ, Mei-Dan O, McConkey MO, Brick MJ (2021) Peri-operative platelet-rich plasma in arthroscopic femoroacetabular impingement surgery: a randomized controlled trial. J Hip Preserv Surg 8(1):14–21
Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA (2009) Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med 37(11):2259–2272
Ganz R, Leunig M, Leunig-Ganz K, Harris WH (2008) The etiology of osteoarthritis of the hip. Clin Orthop Relat Res 466(2):264–272
Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA (2003) Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 417:112–120
Gazendam A, Ekhtiari S, Bozzo A, Phillips M, Bhandari M (2021) Intra-articular saline injection is as effective as corticosteroids, platelet-rich plasma and hyaluronic acid for hip osteoarthritis pain: a systematic review and network meta-analysis of randomised controlled trials. Br J Sports Med 55(5):256–261
Griffin DR, Dickenson EJ, Wall PDH, Achana F, Donovan JL, Griffin J, Hobson R, Hutchinson CE, Jepson M, Parsons NR, Petrou S, Realpe A, Smith J, Foster NE, FASHIoN Study Group (2018) Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial. Lancet 391(10136):2225–2235
Hartwell MJ, Zhang AL (2023) Editorial commentary: hip arthroscopy in patients with early degeneration who receive intra-articular bone marrow aspirate concentrate can achieve outcomes similar to nonarthritic patients. Arthroscopy 39(6):1438–1439
Hernigou J, Verdonk P, Homma Y, Verdonk R, Goodman SB, Hernigou P (2022) Nonoperative and operative bone and cartilage regeneration and orthopaedic biologics of the hip: an orthoregeneration network (ON) foundation hip review. Arthroscopy 38(2):643–656
Ivone A, Fioruzzi A, Jannelli E, Castelli A, Ghiara M, Ferranti Calderoni E, Fontana A (2019) Micro-fragmented Adipose Tissue Transplantation (MATT) for the treatment of acetabular delamination. A two years follow up comparison study with microfractures. Acta Biomed 90(Suppl 12):69–75
Jildeh TR, Abbas MJ, Buckley P, Okoroha KR (2021) The use of biologics for hip preservation. Curr Rev Musculoskelet Med 14(2):145–154
Johal H, Khan M, Yung S-HP, Dhillon MS, Fu FH, Bedi A, Bhandari M (2019) Impact of platelet-rich plasma use on pain in orthopaedic surgery: a systematic review and meta-analysis. Sports Health 11(4):355–366
Kucharik MP, Abraham PF, Nazal MR, Varady NH, Eberlin CT, Meek WM, Naessig SA, Martin SD (2021) Treatment of full-thickness acetabular chondral flaps during hip arthroscopy: bone marrow aspirate concentrate versus microfracture. Orthop J Sports Med 9(12):23259671211059170
LaFrance R, Kenney R, Giordano B, Mohr K, Cabrera J, Snibbe J (2015) The effect of platelet enriched plasma on clinical outcomes in patients with femoroacetabular impingement following arthroscopic labral repair and femoral neck osteoplasty. J Hip Preserv Surg 2(2):158–163
Lamplot JD, Rodeo SA, Brophy RH (2020) A practical guide for the current use of biologic therapies in sports medicine. Am J Sports Med 48(2):488–503
Lee YK, Lee GY, Lee JW, Lee E, Kang HS (2016) Intra-articular injections in patients with femoroacetabular impingement: a prospective, randomized, double-blind, cross-over study. J Korean Med Sci 31(11):1822–1827
Lim A, Zhu JB, Khanduja V (2022) The use of intra-articular platelet-rich plasma as a therapeutic intervention for hip osteoarthritis: a systematic review and meta-analysis. Am J Sports Med 51(9):2487–2497
Mariani E, Pulsatelli L, Facchini A (2014) Signaling pathways in cartilage repair. Int J Mol Sci 15(5):8667–8698
Martin SD, Kucharik MP, Abraham PF, Nazal MR, Meek WM, Varady NH (2022) Functional outcomes of arthroscopic acetabular labral repair with and without bone marrow aspirate concentrate. J Bone Joint Surg Am 104(1):4–14
Mishra A, Harmon K, Woodall J, Vieira A (2012) Sports medicine applications of platelet rich plasma. Curr Pharm Biotechnol 13(7):1185–1195
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1097/01.blo.0000096804.78689.c2
Mullins K, Filan D, Carton P (2022) Platelet-rich plasma is not associated with improved outcomes following hip femoroacetabular impingement surgery: very low-quality evidence suggests hyaluronic acid and cell-based therapies may be beneficial—a systematic review of biological treatments. ASMAR 4(4):e1557–e1573
Murray IR, Geeslin AG, Goudie EB, Petrigliano FA, LaPrade RF (2017) Minimum information for studies evaluating biologics in orthopaedics (MIBO): platelet-rich plasma and mesenchymal stem cells. J Bone Joint Surg Am 99(10):809–819
Ometti M, Schipani D, Conte P, Pironti P, Salini V (2020) The efficacy of intra-articular HYADD4-G injection in the treatment of femoroacetabular impingement: results at one year follow up. J Drug Assess 9(1):159–166
Pasculli RM, Callahan EA, Wu J, Edralin N, Berrigan WA (2023) Non-operative management and outcomes of femoroacetabular impingement syndrome. Curr Rev Musculoskelet Med. https://doi.org/10.1007/s12178-023-09863-x
Philippon MJ, Briggs KK, Yen Y-M, Kuppersmith DA (2009) Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br 91(1):16–23
Raeissadat SA, Ghazi Hosseini P, Bahrami MH, Salman Roghani R, Fathi M, Gharooee Ahangar A, Darvish M (2021) The comparison effects of intra-articular injection of Platelet Rich Plasma (PRP), Plasma Rich in Growth Factor (PRGF), Hyaluronic Acid (HA), and ozone in knee osteoarthritis; a one year randomized clinical trial. BMC Musculoskelet Disord 22(1):134. https://doi.org/10.1186/s12891-021-04017-x
Rafols C, Monckeberg JE, Numair J, Botello J, Rosales J (2015) Platelet-rich plasma augmentation of arthroscopic hip surgery for femoroacetabular impingement: a prospective study with 24-month follow-up. Arthroscopy 31(10):1886–1892
Rahman S, Sutedja E, Ayu O, Amirsyah M (2022) The effect of platelet-rich plasma on type I collagen production, VEGF expression, and neovascularization after femoral bone implants: a study on rat models. Orthop Res Rev 14:207–214
Redmond JM, Gupta A, Stake CE, Hammarstedt JE, Finch NA, Domb BG (2015) Clinical results of hip arthroscopy for labral tears: a comparison between intraoperative platelet-rich plasma and bupivacaine injection. Arthroscopy 31(3):445–453
Rivera E, Seijas R, Rubio M, García-Balletbó M, Vilar JM, Boada PL, Cugat R (2020) Outcomes at 2-years follow-up after hip arthroscopy combining bone marrow concentrate. J Invest Surg 33(7):655–663
Robinson PG, Murray IR, Maempel J, Rankin CS, Hamilton D, Gaston P (2019) Use of biologics as an adjunct therapy to arthroscopic surgery for the treatment of femoroacetabular impingement: a systematic review. Orthop J Sports Med 7(12):2325967119890673
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (MINORS): development and validation of a new instrument: methodological index for non-randomized studies. ANZ J Surg 73(9):712–716
Sullivan SW, Aladesuru OM, Ranawat AS, Nwachukwu BU (2021) The use of biologics to improve patient-reported outcomes in hip preservation. J Hip Preserv Surg 8(1):3–13
Wang Z, Sun Q-M, Zhang F-Q, Zhang Q-L, Wang L-G, Wang W-J (2019) Core decompression combined with autologous bone marrow stem cells versus core decompression alone for patients with osteonecrosis of the femoral head: a meta-analysis. Int J Surg 69:23–31
Ye Y, Zhou X, Mao S, Zhang J, Lin B (2018) Platelet rich plasma versus hyaluronic acid in patients with hip osteoarthritis: a meta-analysis of randomized controlled trials. Int J Surg 53:279–287
Yu S, Hu R, Feng H, Huang D (2023) Efficacy of platelet-rich plasma injection in the treatment of frozen shoulder: a systematic review and meta-analysis. J Back Musculoskelet Rehabil 36(3):551–564
Funding
This study was performed at the American Hip Institute Research Foundation.
Author information
Authors and Affiliations
Contributions
TG: data collection/analysis and writing of the manuscript. AJC: data collection/analysis and writing of the manuscript. SKS: data collection/analysis and writing of the manuscript. BDK: data interpretation and revision of the manuscript. AP: data interpretation and revision of the manuscript. BGD: data interpretation and revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
B.G.D has received royalties from Arthrex, Inc., DJO Global, Inc., Medacta USA, Inc., Orthomerica; has received speaking fees from Arthrex, Inc., Stryker Corp, Medacta Inc; has received consulting fees from Arthrex, Inc; has received research support from Arthrex, Inc., Ossur, Stryker Endoscopy, and Medacta Inc; has received any other financial or material support from Arthrex, Inc., Stryker Endoscopy. B.G.D serves on the editorial or governing board for Arthroscopy, a board member for the Arthroscopy Journal, American Hip Institute Research Foundation, AANA Learning Center Committee. The American Hip Institute Research Foundation fund research and is where our study was performed. B.D.K is a member of the Arthroscopy Editorial Board. Ms. George, Dr. Curley, Ms. Saeed, and Dr. Parsa have no conflicts of interest to disclose.
Ethical approval
This study was performed in accordance with the ethical standards in the 1964 Declaration of Helsinki. This study was carried out in accordance with relevant regulations of the US Health Insurance Portability and Accountability Act (HIPAA). Details that might disclose the identity of the subjects under study have been omitted. This study was approved by the IRB. (IRB ID: 5276).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
George, T., Curley, A.J., Saeed, S.K. et al. Orthobiologics as an adjunct in treatment of femoroacetabular impingement syndrome: cell-based therapies facilitate improved postoperative outcomes in the setting of acetabular chondral lesions—a systematic review. Knee Surg Sports Traumatol Arthrosc 31, 6020–6038 (2023). https://doi.org/10.1007/s00167-023-07624-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07624-4