Abstract
Purpose
Current options for treating an Achilles tendon rupture (ATR) include conservative and surgical approaches. Endoscopic flexor hallucis longus (FHL) transfer has been recently proposed to treat acute ruptures, but its cost-effectiveness potential remains to be evaluated. Therefore, the objective of this study was to perform an early cost-effectiveness analysis of endoscopic FHL transfer for acute ATRs, comparing the costs and benefits of current treatments from a societal perspective.
Methods
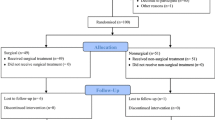
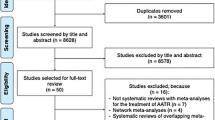
A conceptual model was created, with a decision tree, to outline the main health events during the treatment of an acute ATR. The model was parameterized using secondary data. A systematic review of the literature was conducted to gather information on the outcomes of current treatments. Data related to outcomes of endoscopic FHL transfers in acute Achilles ruptures was obtained from a single prospective study. Analysis was limited to the two first years. The incremental cost-effectiveness ratio was the main outcome used to determine the preferred strategy. A willingness-to-pay threshold of $100,000 per quality-adjusted life-year was used. Sensitivity analyses were performed to determine whether changes in input parameters would cause significant deviation from the reference case results. Specifically, a probability sensitivity analysis was conducted using Monte Carlo simulations, and a one-way sensitivity analysis was conducted by sequentially varying each model parameter within a given range.
Results
For the reference case, incremental cost-effectiveness ratios exceeded the willingness-to-pay threshold for all the surgical approaches. Overall, primary treatment was the main cost driver. Conservative treatment showed the highest direct costs related to the treatment of complications. In the probabilistic sensitivity analysis, at a willingness-to-pay threshold of $100,000, open surgery was cost-effective in 50.9%, minimally invasive surgery in 55.8%, and endoscopic FHL transfer in 72% of the iterations. The model was most sensitive to parameters related to treatment utilities, followed by the costs of primary treatments.
Conclusion
Surgical treatments have a moderate likelihood of being cost-effective at a willingness-to-pay threshold of $100,000, with endoscopic FHL transfer showing the highest likelihood. Following injury, interventions to improve health-related quality of life may be better suited for improved cost-effectiveness.
Level of evidence
Level III.




Similar content being viewed by others
Abbreviations
- AT:
-
Achilles tendon
- ATR:
-
Achilles tendon rupture
- ATRS:
-
Achilles Tendon Total Rupture Score
- CEA:
-
Cost-effectiveness analysis
- CI:
-
Confidence interval
- DVT:
-
Deep venous thrombosis
- FHL:
-
Flexor hallucis longus
- HRQoL:
-
Health-related quality of life
- ICER:
-
Incremental cost-effectiveness ratio
- MIS:
-
Minimally invasive surgery
- NMB:
-
Net monetary benefit
- ORS:
-
Open revision surgery
- PSA:
-
Probabilistic sensitivity analysis
- QALYs:
-
Quality-adjusted life-years
- RTW:
-
Return to work
- WHPs:
-
Wound-healing problems
- WTP:
-
Willingness to pay
References
Abdelatif NMN, Batista JP (2022) Outcomes of percutaneous achilles repair compared with endoscopic flexor hallucis longus tendon transfer to treat achilles tendon ruptures. Foot Ankle Int. https://doi.org/10.1177/10711007221096674
Attia AK, Mahmoud K, d’Hooghe P, Bariteau J, Labib SA, Myerson MS (2021) Outcomes and complications of open versus minimally invasive repair of acute achilles tendon ruptures: a systematic review and meta-analysis of randomized controlled trials. Am J Sports Med. https://doi.org/10.1177/03635465211053619
Barfod KW, Bencke J, Lauridsen HB, Ban I, Ebskov L, Troelsen A (2014) Nonoperative dynamic treatment of acute achilles tendon rupture: the influence of early weight-bearing on clinical outcome: a blinded, randomized controlled trial. J Bone Joint Surg Am 96:1497–1503
Barfod KW, Hansen MS, Hölmich P, Kristensen MT, Troelsen A (2020) Efficacy of early controlled motion of the ankle compared with immobilisation in non-operative treatment of patients with an acute Achilles tendon rupture: an assessor-blinded, randomised controlled trial. Br J Sports Med 54:719–724
Barfod KW, Nielsen EG, Olsen BH, Vinicoff PG, Troelsen A, Holmich P (2020) Risk of deep vein thrombosis after acute achilles tendon rupture: a secondary analysis of a randomized controlled trial comparing early controlled motion of the ankle versus immobilization. Orthop J Sports Med. https://doi.org/10.1177/2325967120915909
Batista JP, Abdelatif NMN, Del Vecchio JJ, Diniz P, Pereira H (2020) Endoscopic flexor hallucis longus transfer for the management of acute achilles tendon ruptures: a prospective case series report with a minimum of 18 months’ follow-up. J Foot Ankle Surg 59:927–937
Baumfeld D, Baumfeld T, Figueiredo AR, de Araujo Junior LF, Macedo B, Silva TAA, Raduan F, Nery C (2017) Endoscopic flexor halluces longus transfer for chronic Achilles Tendon rupture—technique description and early post-operative results. Muscles Ligaments Tendons J 7:341–346
Bishop ME, Comer CD, Kane JM, Maltenfort MG, Raikin SM (2017) Open repair of acute achilles tendon ruptures: is the incidence of clinically significant wound complications overestimated? Foot Ankle Orthop. https://doi.org/10.1177/2473011417699834
Bowers MW, Turner NS, Ryssman DB, Moran SL (2019) Outcomes following treatment of the infected Achilles Tendon. Foot Ankle Orthop. https://doi.org/10.1177/2473011419846943
Buddecke D (2021) Acute achilles tendon ruptures. Clin Podiatr Med Surg 38:201–226
Carmont MR, Heaver C, Pradhan A, Mei-Dan O, Gravare Silbernagel K (2013) Surgical repair of the ruptured Achilles tendon: the cost-effectiveness of open versus percutaneous repair. Knee Surg Sports Traumatol Arthrosc 21:1361–1368
Cetti R, Christensen SE, Ejsted R, Jensen NM, Jorgensen U (1993) Operative versus nonoperative treatment of Achilles tendon rupture. A prospective randomized study and review of the literature. Am J Sports Med 21:791–799
Costa ML, MacMillan K, Halliday D, Chester R, Shepstone L, Robinson AHN, Donell ST (2006) Randomised controlled trials of immediate weight-bearing mobilisation for rupture of the tendo Achillis. J Bone Joint Surg Br 88:69–77
Daroudi R, Akbari Sari A, Nahvijou A, Faramarzi A (2021) Cost per DALY averted in low, middle- and high-income countries: evidence from the global burden of disease study to estimate the cost-effectiveness thresholds. Cost Eff Resour Alloc. https://doi.org/10.1186/s12962-021-00260-0
De la Fuente C, Peña y Lillo R, Carreño G, Marambio H, (2016) Prospective randomized clinical trial of aggressive rehabilitation after acute Achilles tendon ruptures repaired with Dresden technique. Foot 26:15–22
Diniz P, Pacheco J, Guerra-Pinto F, Pereira H, Ferreira FC, Kerkhoffs G (2020) Achilles tendon elongation after acute rupture: is it a problem? A systematic review. Knee Surg Sports Traumatol Arthrosc 28:4011–4030
Ebinesan AD, Sarai BS, Walley GD, Maffulli N (2008) Conservative, open or percutaneous repair for acute rupture of the Achilles tendon. Disabil Rehabil 30:1721–1725
FAIR Health. Accessed June 22, 2021. http://www.fairhealthconsumer.org
Faucett SC, Seagrave RA, Genuario J, Hildebrand G, Metzl JA (2017) Treatment of achilles tendon rupture: a cost-effectiveness analysis. Arthroscopy. https://doi.org/10.1016/j.arthro.2017.08.154
Figueiredo L, Makhni EC, Dierks M, Ferreira FC, Finkelstein S (2021) Early cost estimating model for new bioabsorbable orthopedic implant candidates: a theoretical study. J Mech Behav Biomed Mater. https://doi.org/10.1016/j.jmbbm.2021.104731
Fischer S, Colcuc C, Gramlich Y, Stein T, Abdulazim A, von Welck S, Hoffmann R (2021) Prospective randomized clinical trial of open operative, minimally invasive and conservative treatments of acute Achilles tendon tear. Arch Orthop Trauma Surg 141:751–760
Gonçalves S, Caetano R, Corte-Real N (2015) Salvage flexor hallucis longus transfer for a failed achilles repair: endoscopic technique. Arthrosc Tech. https://doi.org/10.1016/j.eats.2015.03.017
Harkin E, Schiff A, Pinzur M, Schiffman C (2017) Comparative cost of surgical and nonsurgical treatment of acute achilles tendon rupture. Foot Ankle Orthop. https://doi.org/10.1177/2473011417S000188
Hatswell AJ, Bullement A, Briggs A, Paulden M, Stevenson MD (2018) Probabilistic sensitivity analysis in cost-effectiveness models: determining model convergence in cohort models. Pharmacoeconomics 36:1421–1426
Heikkinen J, Lantto I, Piilonen J, Flinkkilä T, Ohtonen P, Siira P, Laine V, Niinimäki J, Pajala A, Leppilahti J (2017) Tendon length, calf muscle atrophy, and strength deficit after acute Achilles tendon rupture: long-term follow-up of patients in a previous study. J Bone Joint Surg Am 99:1509–1515
Karabinas PK, Benetos IS, Lampropoulou-Adamidou K, Romoudis P, Mavrogenis AF, Vlamis J (2014) Percutaneous versus open repair of acute Achilles tendon ruptures. Eur J Orthop Surg Traumatol 24:607–613
Koltsov JCB, Gribbin C, Ellis SJ, Nwachukwu BU (2020) Cost-effectiveness of operative versus non-operative management of acute Achilles tendon ruptures. HSS J 16:39–45
Korkmaz M, Fatih Erkoc M, Yolcu S, Balbaloglu O, Öztemur Z, Karaaslan F (2015) Weight bearing the same day versus non-weight bearing for 4 weeks in Achilles tendon rupture. J Orthop Sci 20:513–516
Lantto I, Heikkinen J, Flinkkila T, Ohtonen P, Siira P, Laine V, Leppilahti J (2016) A prospective randomized trial comparing surgical and nonsurgical treatments of acute achilles tendon ruptures. Am J Sports Med 44:2406–2414
Liu J-Y, Duan W-F, Shen S, Ye Y, Sun Y-Q, He W (2020) Achillon versus modified minimally invasive repair treatment in acute Achilles tendon rupture. J Orthop Surg. https://doi.org/10.1177/2309499020908354
Lonzarić D, Kruščić A, Dinevski D, Povalej Bržan P, Jesenšek Papež B (2017) Primary surgical repair of acute Achilles tendon rupture: comparative results of three surgical techniques. Wien Klin Wochenschr 129:176–185
Lui TH (2012) Minimally invasive flexor hallucis longus transfer in management of acute achilles tendon rupture associated with tendinosis: a case report. Foot Ankle Spec 5:111–114
Lui TH, Chan WC, Maffulli N (2016) Endoscopic flexor hallucis longus tendon transfer for chronic achilles tendon rupture. Sports Med Arthrosc Rev 24:38–41
Majewski M, Rohrbach M, Czaja S, Ochsner P (2006) Avoiding sural nerve injuries during percutaneous Achilles tendon repair. Am J Sports Med 34:793–798
Manent A, López L, Coromina H, Santamaría A, Domínguez A, Llorens N, Sales M, Videla S (2019) Acute achilles tendon ruptures: efficacy of conservative and surgical (percutaneous, open) treatment—a randomized, controlled. Clinical Trial J Foot Ankle Surg 58:1229–1234
Medicare Part D Drug Spending Dashboard. Centers for Medicare & Medicaid Services. Accessed July 4, 2021. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Information-on-Prescription-Drugs/MedicarePartD
Möller M, Lind K, Movin T, Karlsson J (2002) Calf muscle function after Achilles tendon rupture. A prospective, randomised study comparing surgical and non-surgical treatment. Scand J Med Sci Sports 12:9–16
Möller M, Movin T, Granhed H, Lind K, Faxén E, Karlsson J (2001) Acute rupture of tendon Achillis. A prospective randomised study of comparison between surgical and non-surgical treatment. J Bone Joint Surg Br 83:843–848
Needleman L, Cronan JJ, Lilly MP, Merli GJ, Adhikari S, Hertzberg BS, DeJong MR, Streiff MB, Meissner MH (2018) Ultrasound for lower extremity deep venous thrombosis: multidisciplinary recommendations from the society of radiologists in ultrasound consensus conference. Circulation 137:1505–1515
Nilsson L, Thorlund JB, Kjær IL, Kazlauskas A, Christensen M (2021) Long-term follow-up after acute achilles tendon rupture—does treatment strategy influence functional outcomes? Foot (Edinb). https://doi.org/10.1016/j.foot.2020.101769
Nilsson-Helander K, Swärd L, Silbernagel KG, Thomeé R, Eriksson BI, Karlsson J (2008) A new surgical method to treat chronic ruptures and reruptures of the Achilles tendon. Knee Surg Sports Traumatol Arthrosc 16:614–620
Nistor L (1981) Surgical and non-surgical treatment of Achilles Tendon rupture. A prospective randomized study. J Bone Joint Surg Am 63:394–399
Occupational employment and wages in boston-cambridge-nashua—May 2020: New England information office: US bureau of labor statistics. Accessed June 10, 2021. https://www.bls.gov/regions/new-england/news694 release/occupationalemploymentandwages_boston.htm
OCEBM levels of evidence working group OCEBM levels of evidence—centre for evidence-based medicine (CEBM), University of Oxford. Accessed June 20, 2022. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence
Olsson N, Karlsson J, Eriksson BI, Brorsson A, Lundberg M, Silbernagel KG (2014) Ability to perform a single heel-rise is significantly related to patient-reported outcome after Achilles tendon rupture: Achilles tendon rupture, short-term result. Scand J Med Sci Sports 24:152–158
Olsson N, Silbernagel KG, Eriksson BI, Sansone M, Brorsson A, Nilsson-Helander K, Karlsson J (2013) Stable Surgical repair with accelerated rehabilitation versus nonsurgical treatment for acute Achilles Tendon ruptures: a randomized controlled study. Am J Sports Med 41:2867–2876
Ortel TL, Neumann I, Ageno W, Beyth R, Clark NP, Cuker A, Hutten BA, Jaff MR, Manja V, Schulman S, Thurston C, Vedantham S, Verhamme P, Witt DM, FlorezIzcovichNieuwlaatRossSchünemannWierciochZhangZhang DIARSJHWYY (2020) American society of hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism. Blood Adv 4:4693–4738
Parekh SG, Aran FS, Mithani S, Chopra A (2022) Achilles: failed acute repair. Foot Ankle Clin 27:415–430
Park YH, Kim TJ, Choi GW, Kim HJ (2019) Achilles tendinosis does not always precede Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc 27:3297–3303
Reda Y, Farouk A, Abdelmonem I, El Shazly OA (2020) Surgical versus non-surgical treatment for acute Achilles’ tendon rupture. A systematic review of literature and meta-analysis. Foot Ankle Surg 26:280–288
Reito A, Logren H-L, Ahonen K, Nurmi H, Paloneva J (2018) Risk factors for failed nonoperative treatment and rerupture in acute Achilles tendon rupture. Foot Ankle Int 39:694–703
Sanders GD, Maciejewski ML, Basu A (2019) Overview of cost-effectiveness analysis. JAMA 321:1400–1401
Schlereth T (2020) Guideline “diagnosis and non interventional therapy of neuropathic pain” of the German Society of Neurology (deutsche Gesellschaft für Neurologie). Neurol Res Pract. https://doi.org/10.1186/s42466-020-00063-3
Su AW, Bogunovic L, Johnson J, Klein S, Matava MJ, McCormick J, Smith MV, Wright RW, Brophy RH (2020) Operative versus nonoperative treatment of acute Achilles Tendon ruptures: a pilot economic decision analysis. Orthop J Sports. https://doi.org/10.1177/2325967120909918
Truntzer JN, Triana B, Harris AHS, Baker L, Chou L, Kamal RN (2017) Cost-minimization analysis of the management of acute Achilles Tendon rupture. J Am Acad Orthop Surg 25:449–457
Vega J, Vilá J, Batista J, Malagelada F, Dalmau-Pastor M (2018) Endoscopic flexor hallucis longus transfer for chronic noninsertional Achilles Tendon rupture. Foot Ankle Int 39:1464–1472
Walker J, Nicholson G, Jongerius N, Parelkar P, Harris N, Bissas A (2020) Commonly reported isokinetic parameters do not reveal long-term strength deficits of the Triceps surae complex following operative treatment of Achilles tendon rupture. J Biomech. https://doi.org/10.1016/j.jbiomech.2020.109630
Westin O, Nilsson Helander K, Grävare Silbernagel K, Samuelsson K, Brorsson A, Karlsson J (2018) Patients with an Achilles tendon re-rupture have long-term functional deficits in function and worse patient-reported outcome than primary ruptures. Knee Surg Sports Traumatol Arthrosc 26:3063–3072
Westin O, Svensson M, Nilsson Helander K, Samuelsson K, Grävare Silbernagel K, Olsson N, Karlsson J, Hansson Olofsson E (2018) Cost-effectiveness analysis of surgical versus non-surgical management of acute Achilles tendon ruptures. Knee Surg Sports Traumatol Arthrosc 26:3074–3082
Willits K, Amendola A, Bryant D, Mohtadi NG, Giffin JR, Fowler P, Kean CO, Kirkley A (2010) Operative versus nonoperative treatment of acute Achilles Tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am 92:2767–2775
Acknowledgements
This work is financed by national funds from FCT – Fundação para a Ciência e a Tecnologia, I.P., in the scope of the Project UIDB/04565/2020 and UIDP/04565/2020 of the Research Unit Institute for Bioengineering and Biosciences – iBB and the project LA/P/0140/2020 of the Associate Laboratory Institute for Health and Bioeconomy – i4HB.
Funding
not applicable.
Author information
Authors and Affiliations
Contributions
PD, GK, SF, and FCF designed the study. PD and ASF screened and selected clinical studies and extracted clinical study data. PD, JB, NA, HP, and GK created the decision tree, defined model assumptions, and cost items and quantities. PD developed the computational model with support from LF. PD and FCF, analyzed the data. PD drafted the manuscript with input from LF and FCF. JB, NA, HP, GK, and SF revised the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
not applicable.
Informed consent
not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Diniz, P., Ferreira, A.S., Figueiredo, L. et al. Early analysis shows that endoscopic flexor hallucis longus transfer has a promising cost-effectiveness profile in the treatment of acute Achilles tendon ruptures. Knee Surg Sports Traumatol Arthrosc 31, 2001–2014 (2023). https://doi.org/10.1007/s00167-022-07146-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07146-5