Abstract
Introduction
We determined the prevalence of major depression and suicidal ideation, and the associated risk factors in a large sample of Chinese resident physicians.
Methods
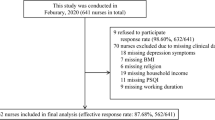
This multi-center cross-sectional study was conducted from December 2019 to February 2020 and involved 1343 residents from eight centers. Extensive characteristics, including demographics, dietary habits, life-related factors, work-related factors, and psychological factors were collected based on a self-reported questionnaire. Specific scales measured the levels of sleep quality, physical activity, depression, perceived organization support, psychological capital, and burnout. Adjusted odds ratios and 95% confidence intervals were determined by binary paired logistic regression.
Results
Of the residents enrolled in the study, 12.90% suffered from major depression and 9.70% suffered from suicidal ideation. Four overlapped independent risk factors were identified for major depression and suicidal ideation: poor sleep quality (OR = 1.317, OR = 1.200); lower optimism of psychological capital (OR = 0.899, OR = 0.835); higher depersonalization, (OR = 1.086, OR = 1.097); and reduced personal accomplishment (OR = 0.963, OR = 0.962). The inappropriate working duration weekly (< 40 h vs. 40–60 h; OR = 2.812, > 60 h vs. 40–60 h; OR = 1.945), and higher emotional exhaustion (OR = 1.121) were the only risk factors for major depression. Higher hope of psychological capital (OR = 1.077) was only for suicidal ideation.
Conclusion
This study revealed a substantial prevalence of major depression and suicidal ideation in Chinese residents, and identified several shared risk factors for major depression and suicidal ideation. These findings enrich the existing theoretical model of depression and demonstrated a critical need for additional studies that investigate intervention strategies that can address the mental health in residents.
Trial registration
Chinese Clinical Trial Registry, ChiCTR1900027707. Registered 24 Nov. 2019, http://www.chictr.org.cn/index.aspx



Similar content being viewed by others
Availability of data and materials
Not applicable.
References
Gotlib IHHC (2009) Handbook of depression. Guilford Publications, New York
Romera I et al (2010) Social and occupational functioning impairment in patients in partial versus complete remission of a major depressive disorder episode. A six-month prospective epidemiological study. Eur Psychiatry 25(1):58–65
Liu Q et al (2019) Changes in the global burden of depression from 1990 to 2017: Findings from the Global Burden of Disease study. J Psychiatr Res
Wang Q, Tian W (2018) Prevalence, awareness, and treatment of depressive symptoms among the middle-aged and elderly in China from 2008 to 2015. Int J Health Plann Manag 33(4):1060–1070
Shanafelt TD et al (2012) Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med 172(18):1377–1385
Fang H et al (2018) Depressive symptoms and workplace-violence-related risk factors among otorhinolaryngology nurses and physicians in Northern China: a cross-sectional study. BMJ Open 8(1):e019514
National Mental Health Survey of Doctors and Medical Students, Australia (2011) http://www.beyondblue.org.au/docs/default-source/default-document-library/bl1132-report-nmhdmss-full-report_web
Donisi V et al (2013) Prediction of community mental health service utilization by individual and ecological level socio-economic factors. Psychiatry Res 209(3):691–698
Schneider SE, Phillips WM (1993) Depression and anxiety in medical, surgical, and pediatric interns. Psychol Rep 72(3 Pt 2):1145–1146
Mata DA et al (2015) Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA 314(22):2373–2383
Lin DT et al (2017) Prevalence and predictors of depression among general surgery residents. Am J Surg 213(2):313–317
Dyrbye LN et al (2014) Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med 89(3):443–451
de Oliveira GJ et al (2013) The prevalence of burnout and depression and their association with adherence to safety and practice standards: a survey of United States anesthesiology trainees. Anesth Analg 117(1):182–193
Wang JN et al (2010) Prevalence and associated factors of depressive symptoms among Chinese doctors: a cross-sectional survey. Int Arch Occup Environ Health 83(8):905–911
Joules NWDTA (2014) Depression in resident physicians: a systematic review. Open J Depress (03):89–100
Bhandari PM et al (2017) Sleep quality, internet addiction and depressive symptoms among undergraduate students in Nepal. BMC Psychiatry 17(1):106
Raniti MB et al (2017) Sleep duration and sleep quality: associations with depressive symptoms across adolescence. Behav Sleep Med 15(3):198–215
UC Berkeley Graduate Assembly (2014) Graduate Student Happiness and Well-being Report. http://ga.berkeley.edu/wellbeingreport
Strine TW et al (2008) The association of depression and anxiety with obesity and unhealthy behaviors among community-dwelling US adults. Gen Hosp Psychiatry 30(2):127–137
Liu L et al (2012) The mediating role of psychological capital on the association between occupational stress and depressive symptoms among Chinese physicians: a cross-sectional study. BMC Public Health 12:219
Liu L et al (2017) Disease activity, resilience and health-related quality of life in Chinese patients with rheumatoid arthritis: a multi-center, cross-sectional study. Health Qual Life Outcomes 15(1):149
Hakanen JJ, Schaufeli WB (2012) Do burnout and work engagement predict depressive symptoms and life satisfaction? A three-wave seven-year prospective study. J Affect Disord 141(2–3):415–424
Ketchen LS et al (2015) Variations in student mental health and treatment utilization across US Colleges and Universities. J Am Coll Health 63(6):388–396
Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16(9):606–613
Craig CL et al (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35(8):1381–1395
Buysse DJ et al (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Eisenberger RSF (2011) Perceived organizational support: Fostering enthusiastic and productive employees. J Appl Psychol 3(71):500–507
Luthans FABAJ (2007) Positive psychological capital: measurement and relationship with performance and satisfaction. Pers Psychol (60):541–572
Zhang KZSDY (2010) Positive psychological capital: measurement and its association with mental health. Stu Psychol Behav (8):58–64
CP L (2003) Work-family conflict and job burnout of doctors and nurses. Chin Ment Health. (17):807–9 (in Chinese)
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res 46(3):399–424
Peduzzi P et al (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49(12):1373–1379
Sullivan P, Buske L (1998) Results from CMA’s huge 1998 physician survey point to a dispirited profession. CMAJ 159(5):525–528
Kocalevent RD, Hinz A, Brahler E (2013) Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry 35(5):551–555
Grover S et al (2018) Psychological problems and burnout among medical professionals of a tertiary care hospital of North India: a cross-sectional study. Indian J Psychiatry 60(2):175–188
Kishore SDDMA (2016) Breaking the culture of silence on physician suicide. Natl Acad Med
Yaghmour NA et al (2017) Causes of death of residents in ACGME-accredited programs 2000 through 2014: implications for the learning environment. Acad Med 92(7):976–983
Maslach C, Schaufeli WB, Leiter MP (2001) Job burnout. Annu Rev Psychol 52:397–422
Shin HNHJY (2013) A longitudinal examination of the relationship between teacher burnout and depression. J Employ Couns (50):124–37
Stehman CR et al (2019) Burnout, drop out, suicide: physician loss in emergency medicine. Part I West J Emerg Med 20(3):485–494
Rodriguez-Socarras M et al (2018) Fatigue syndrome: stress, burnout and depression in Urology. Arch Esp Urol 71(1):46–54
Bakker AB, SWDE (2000) Using equity theory to examine the difference between burnout and depression. Anxiety Stress Coping (13):247–68
Wang Z et al (2017) Associations between occupational stress, burnout and well-being among manufacturing workers: mediating roles of psychological capital and self-esteem. BMC Psychiatry 17(1):364
Heinitz K et al (2018) Positive organizational behavior: longitudinal effects on subjective well-being. PLoS ONE 13(6):e0198588
Rand KL (2009) Hope and optimism: latent structures and influences on grade expectancy and academic performance. J Pers 77(1):231–260
Theory SCH (2002) Rainbows in the mind. PSYCHOL INQ 4(13):249–275
Irwin MR, Olmstead R, Carroll JE (2016) Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry 80(1):40–52
Dantzer R et al (2008) From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci 9(1):46–56
Ursin R (2002) Serotonin and sleep. Sleep Med Rev 6(1):55–69
Mahar I et al (2014) Stress, serotonin, and hippocampal neurogenesis in relation to depression and antidepressant effects. Neurosci Biobehav Rev 38:173–192
Dinis J, Braganca M (2018) Quality of sleep and depression in College students: a systematic review. Sleep Sci 11(4):290–301
Azhar GS, Azhar AZ, Azhar AS (2012) Overwork among residents in india: a medical resident’s perspective. J Family Med Prim Care 1(2):141–143
Saini NK et al (2010) Prevalence of stress among resident doctors working in Medical Colleges of Delhi. Indian J Public Health 54(4):219–223
Dyrbye LN, Thomas MR, Shanafelt TD (2006) Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med 81(4):354–373
West CP et al (2009) Association of resident fatigue and distress with perceived medical errors. JAMA 302(12):1294–1300
Gelfand DV et al (2004) Effect of the 80-hour workweek on resident burnout. Arch Surg 139(9):933–938 (discussion 938–40)
Antiel RM et al (2012) Surgical training, duty-hour restrictions, and implications for meeting the Accreditation Council for Graduate Medical Education core competencies: views of surgical interns compared with program directors. Arch Surg 147(6):536–541
Acknowledgements
We thank International Science Editing (http://www.internationalscienceediting.com) for editing this manuscript. The authors would like to thank all of the study participants.
Funding
This work was supported by the National Key R&D Program of China (Grant Number 2017YFC0907404) and the National Natural Science Foundation of China (Grant Number 71473268). These sponsors had no role in the study design; in the collection, analysis or interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
LS had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: LS. Acquisition of data, analysis and interpretation of data: SB; QC; DY; YZ. Drafting of the manuscript and critical revision of the manuscript for important intellectual content: SB, LS. Statistical analysis: SB, DY; YZ. Obtaining funding and other (figures): LS.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Financial disclosures
Liping Shan certifies that all conflicts of interest, including specific financial interests, relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending) are none.
Ethical statement
Ethical approval (No. 2019PS647K) was provided by the Institutional Research and Ethics Committee of the Shengjing Hospital Affiliated China Medical University. All centers were in accordance with this ethical standards. Informed consent from all eligible subjects were obtained. The clinical research registry UIN is ChiCTR1900027707. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bai, S., Chang, Q., Yao, D. et al. The prevalence and risk factors for major depression and suicidal ideation in medical residents based on a large multi-center cross-sectional study using the propensity score-matched method. Soc Psychiatry Psychiatr Epidemiol 57, 2279–2291 (2022). https://doi.org/10.1007/s00127-022-02351-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-022-02351-6