Abstract
Purpose
Due to the family-oriented cultural and legal context in China, understanding the difference between patients’ and family members’ experiences of psychiatric services not only enriches perspectives of service quality assessment, but also promotes service utilization. This study aimed to compare experiences of psychiatric inpatient services between patients and their family members in China.
Methods
The study included 126 dyads of patients and family members consecutively recruited from the psychiatric inpatient department in a large hospital in China. The responsiveness performance questionnaire was used to measure the experiences of psychiatric inpatient services after patient discharge. After adjusting reporting heterogeneity based on vignettes, dyad difference was examined by intraclass correlation coefficients (ICCs) and paired Wilcoxon signed-rank tests with Bonferroni correction in multigroup testing. Subgroup analyses were conducted within strata of four selected clinical and socio-demographic factors, to test their influence on difference pattern of experiences.
Results
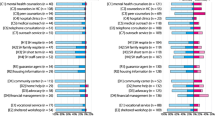
Poor consistency was found for all responsiveness items and the total scores among the 126 dyads and in most subgroup analyses (ICC < 0.6). Paired Wilcoxon signed-rank tests found that patients rated lower than their family members on the item of “asking user’s opinions” in 126-dyad comparison (P < 0.05) and 3 subgroups related to severe mental disorders and income inequality after Bonferroni correction.
Conclusion
Results reveal inconsistent experiences of psychiatric inpatient services within families in China. Moreover, when making medical decisions, family members’ opinions, rather than patients’, are more frequently taken into consideration, especially on conditions where imbalanced decision-making power exists between patients and their family members. In the future, user experience improvement should pay equal attention to patients and family members, and the benefits of family involvement and patients’ rights of shared decision-making should be carefully balanced.
Similar content being viewed by others
References
Fortin M, Cao Z, Fleury MJ (2018) A typology of satisfaction with mental health services based on Andersen’s behavioral model. Soc Psychiatry Psychiatr Epidemiol 53 (6):587–595
Woodward S, Berry K, Bucci S (2017) A systematic review of factors associated with service user satisfaction with psychiatric inpatient services. J Psychiatr Res 92:81–93
Forouzan S, Padyab M, Rafiey H, Ghazinour M, Dejman M, San Sebastian M (2015) Measuring the mental health-care system responsiveness: results of an outpatient survey in Tehran. Front Public Health 3:285
Priebe S, Miglietta E (2019) Assessment and determinants of patient satisfaction with mental health care. World Psychiatry 18 (1):30–31
Doody O, Butler MP, Lyons R, Newman D (2017) Families’ experiences of involvement in care planning in mental health services: an integrative literature review. J Psychiatr Ment Health Nurs 24 (6):412–430
Cree L, Brooks HL, Berzins K, Fraser C, Lovell K, Bee P (2015) Carers’ experiences of involvement in care planning: a qualitative exploration of the facilitators and barriers to engagement with mental health services. BMC Psychiatry 15:208
Rowe J (2012) Great expectations: a systematic review of the literature on the role of family carers in severe mental illness, and their relationships and engagement with professionals. J Psychiatr Ment Health Nurs 19 (1):70–82
Svendsen ML, Ellegaard T, Jeppesen KA, Riiskjær E, Nielsen BK (2021) Family involvement and patient-experienced improvement and satisfaction with care: a nationwide cross-sectional study in Danish psychiatric hospitals. BMC Psychiatry 21 (1):190
Cong Y (2004) Doctor-family-patient relationship: the Chinese paradigm of informed consent. J Med Philos 29 (2):149–178
Dai Q (2003) Informed consent in China: status quo and its future. Med Law Int 6 (1):53–71
Fan R (2000) Informed consent and truth telling: the Chinese Confucian moral perspective. HEC Forum 12 (1):87–95
Zhou JS, Xiang YT, Zhu XM, Liang W, Li H, Yi J et al (2015) Voluntary and involuntary psychiatric admissions in China. Psychiatr Serv 66 (12):1341–1346
Di X, Cheng HG (2013) Competence of consent and associated factors among inpatients of schizophrenia in Changsha, China. Schizophr Res 150 (1):325–326
Chen H, Phillips M, Cheng H, Chen Q, Chen X, Fralick D et al (2012) Mental health law of the People’s Republic of China (english translation with annotations): translated and annotated version of China’s new mental health law. Shanghai Arch Psychiatry 24 (6):305–321
Jiang F, Rakofsky J, Zhou H, Hu L, Liu T, Wu S et al (2019) Satisfaction of psychiatric inpatients in China: clinical and institutional correlates in a national sample. BMC Psychiatry 19 (1):19
Jiang F, Hu L, Zhao R, Zhou H, Wu Y, Rakofsky JJ et al (2019) Satisfaction of family members with inpatient psychiatric care and its correlates: a national survey in China. BMC Psychiatry 19 (1):427
Boyer L, Baumstarck-Barrau K, Cano N, Zendjidjian X, Belzeaux R, Limousin S et al (2009) Assessment of psychiatric inpatient satisfaction: a systematic review of self-reported instruments. Eur Psychiatry 24 (8):540–549
Ewertzon M, Andershed B, Svensson E, Lützén K (2011) Family members’ expectation of the psychiatric healthcare professionals’ approach towards them. J Psychiatr Ment Health Nurs 18 (2):146–157
Dourado BM, Arruda BFT, Salles VB, de Souza Júnior SA, Dourado VM, Pinto JP (2018) Evaluation of family caregiver satisfaction with a mental health inpatient service. Trends Psychiatry Psychother 40 (4):300–309
Tyson P, Ayton A, Ahmed OAA, Bowie P, Worrall-Davies A, Mortimer A (2001) A comparison of the service satisfaction and intervention needs of patients with schizophrenia and their relatives. Int J Psychiatry Clin Pract 5 (4):263–271
Gigantesco A, Picardi A, Chiaia E, Balbi A, Morosini P (2002) Patients’ and relatives’ satisfaction with psychiatric services in a large catchment area in Rome. Eur Psychiatry 17 (3):139–147
Bramesfeld A, Klippel U, Seidel G, Schwartz FW, Dierks ML (2007) How do patients expect the mental health service system to act? Testing the WHO responsiveness concept for its appropriateness in mental health care. Soc Sci Med 65 (5):880–889
Forouzan AS, Rafiey H, Padyab M, Ghazinour M, Dejman M, Sebastian MS (2014) Reliability and validity of a Mental Health System Responsiveness Questionnaire in Iran. Glob Health Action 7:24748
Zhou W, Xiao S, Feng C, Yu Y, Wang D, Hu C, Liu X (2022) Measuring the quality of mental health services from the patient perspective in China: psychometric evaluation of the Chinese version of the World Health Organization responsiveness performance questionnaire. Glob Health Action 15 (1):2035503
Valentine NB, Bonsel GJ, Murray CJ (2007) Measuring quality of health care from the user’s perspective in 41 countries: psychometric properties of WHO’s questions on health systems responsiveness. Qual Life Res 16 (7):1107–1125
Rice N, Robone S, Smith P (2011) Analysis of the validity of the vignette approach to correct for heterogeneity in reporting health system responsiveness. Eur J Health Econ 12 (2):141–162
Murray CJ, Kawabata K, Valentine N (2001) People’s experience versus people’s expectations. Health Aff (Millwood) 20 (3):21–24
Liu Q, Zhou W, Niu L, Yu Y, Chen L, Luo B et al (2019) Comparison of expectations for health services between inpatients from mental health department and endocrinology department in China. Patient Prefer Adherence 13:1851–1860
Zaki R, Bulgiba A, Ismail R, Ismail NA (2012) Statistical methods used to test for agreement of medical instruments measuring continuous variables in method comparison studies: a systematic review. PLoS One 7 (5):e37908
Bruton A, Conway JH, Holgate ST (2000) Reliability: What is it, and how is it measured? Physiotherapy 86 (2):94–99
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15 (2):155–163
Mehta S, Bastero-Caballero RF, Sun Y, Zhu R, Murphy DK, Hardas B et al (2018) Performance of intraclass correlation coefficient (ICC) as a reliability index under various distributions in scale reliability studies. Stat Med 37 (18):2734–2752
Zhou W, Liu Q, Yu Y, Xiao S, Chen L, Khoshnood K et al (2020) Proxy reliability of the 12-item world health organization disability assessment schedule II among adult patients with mental disorders. Qual Life Res 29 (8):2219–2229
Bramesfeld A, Wedegärtner F, Elgeti H, Bisson S (2007) How does mental health care perform in respect to service users’ expectations? Evaluating inpatient and outpatient care in Germany with the WHO responsiveness concept. BMC Health Serv Res 7:99
Antman FM (2014) Spousal Employment and Intra-Household Bargaining Power. Appl Econ Lett 21 (8):560–563
Bland JM, Altman DG (1995) Multiple significance tests: the Bonferroni method. BMJ 310 (6973):170
Gong N, Zhou Y, Cheng Y, Chen X, Li X, Wang X et al (2018) Practice of informed consent in Guangdong, China: a qualitative study from the perspective of in-hospital patients. BMJ Open 8 (10):e020658
Giacco D, Dirik A, Kaselionyte J, Priebe S (2017) How to make carer involvement in mental health inpatient units happen: a focus group study with patients, carers and clinicians. BMC Psychiatry 17 (1):101
Zhu J, Pan T, Yu H, Dong D (2018) Guan (Care/Control): an ethnographic understanding of care for people with severe mental illness from Shanghai’s Urban communities. Cult Med Psychiatry 42 (1):92–111
Huang C, Plummer V, Lam L, Cross W (2020) Shared decision-making in serious mental illness: a comparative study. Patient Educ Couns 103 (8):1637–1644
Acharya DR, Bell JS, Simkhada P, van Teijlingen ER, Regmi PR (2010) Women’s autonomy in household decision-making: a demographic study in Nepal. Reprod Health 7 (1):15
Fulford KWM, Handa A (2021) New resources for understanding patients’ values in the context of shared clinical decision-making. World Psychiatry 20 (3):446–447
Beitinger R, Kissling W, Hamann J (2014) Trends and perspectives of shared decision-making in schizophrenia and related disorders. Curr Opin Psychiatry 27 (3):222–229
Phillips MR, Zhang J, Shi Q, Song Z, Ding Z, Pang S et al (2009) Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001–05: an epidemiological survey. Lancet 373 (9680):2041–2053
Ma H, Shao Y (2019) Commentary: the implementation of china’s mental health law-defined risk criteria for involuntary admission: a national cross-sectional study of involuntarily hospitalized patients. Front Psychiatry 10:121
Jiang F, Zhou H, Rakofsky JJ, Hu L, Liu T, Liu H et al (2018) The implementation of China’s mental health law-defined risk criteria for involuntary admission: a national cross-sectional study of involuntarily hospitalized patients. Front Psychiatry 9:560
Phillips MR, Chen H, Diesfeld K, Xie B, Cheng HG, Mellsop G et al (2013) China’s new mental health law: reframing involuntary treatment. Am J Psychiatry 170 (6):588–591
Funding
This work was supported by the National Social Science Foundation of China, Grant number 17CGL050.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
This study was approved by Institutional Review Board of the Xiangya School of Public Health, Central South University (XYGW-2018-01). All research participants received informed consent of this study, including a detailed explanation for it.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhou, W., Xie, G., Yu, Y. et al. Patients’ and family members’ experiences of psychiatric inpatient services in China: a comparison based on a dyadic design. Soc Psychiatry Psychiatr Epidemiol 57, 2119–2129 (2022). https://doi.org/10.1007/s00127-022-02296-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-022-02296-w