Abstract
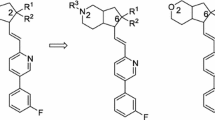
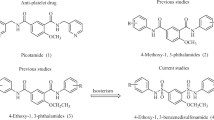
Tetramethylpyrazine (TMP) is commonly used as an antiplatelet drug in clinic. However, the short half-life and low bioavailability limited its applications. 3, 5, 6-Trimethylpyrazine-2-carboxAylic acid (TMP-COOH) and 2-hydroxy-3, 5, 6-trimethylpyrazine (TMP-OH) are the two major active metabolites of TMP in vivo. Both displayed antiplatelet aggregation activity but have obvious disadvantage of rapid metabolism. In this study, conjugates of TMP-COOH/TMP-OH with amino acids were designed to address this issue. We demonstrated that 13 out of 20 conjugates displayed higher antiplatelet aggregation activity than TMP. The optimized compound 4a was further proved to reduce clot retraction, prolong the bleeding time, thrombin time, prothrombin time, activated partial thromboplatin time and reduce fibrinogen content. Taken together, we demonstrated the conjugation strategy could be exploited to develop TMP derivatives for antiplatelet agents.







Similar content being viewed by others
References
Sharifi-Rad J, Rodrigues CF, Sharopov F, Docea AA, Karaca AC, Rad DK, et al. Diet, lifestyle and cardiovascular diseases: linking pathophysiology to cardioprotective effects of natural bioactive compounds. Int J Env Res Pub He. 2020;17:2326.
Lange RA, Hillis LD. The duel between dual antiplatelet therapies. N Engl J Med. 2013;368:1356–7.
Werdan K, Braun-Dullaeus R, Presek P. Anticoagulation in atrial fibrillation: NOAC’s the word. Dtsch Arztebl Int. 2013;110:523–4.
Li W, Liu H, Wei C, Tang M, Kong X, Chen H, et al. Pharmacokinetics and metabolism of Chf197, a ligustrazine derivative, in rats. Fund Clin Pharm. 2015;29:478–87.
Zhang F, Ni GY, Kong DS, Zhang XP, Zhu XJ, Chen L, et al. Ligustrazine attenuates oxidative stress-induced activation of hepatic stellate cells by interrupting platelet-derived growth factor-b receptor-mediated ERK and p38 pathways. Toxicol Appl Pharm. 2012;265:51–60.
Li ZS, Li DL, Huang J, Zhang W, Ding Y, Wang SQ. Preparation of cardiovascular disease-related genes microarray and its application in exploring ligustrazine-induced changes in endothelial gene expression. Pol J Pharm. 2004;56:427–33.
Han JY, Song J, Li XY, Zhu M, Guo W, Xing Z, et al. Ligustrazine suppresses the growth of HRPC cells through the inhibition of cap-dependent translation via both the mTOR and the MEK/ERK pathways. Anticancer Agents Med Chem. 2015;15:764–72.
Liu CF, Lin CH, Chen CF, Huang TC, Lin SC. Antioxidative effects of tetramethylpyrazine on acute ethanol-induced lipid peroxidation. Am J Chin Med. 2005;33:981–8.
Zhang Z, Wei T, Hou J, Li G, Yu S, Xin W. Tetramethylpyrazine scavenges superoxide anion and decreases nitric oxide production in human polymorphonuclear leukocytes. Life Sci. 2003;72:2465–72.
Qian W, Xiong X, Fang Z, Lu H, Wang Z. Protective effect of tetramethylpyrazine on myocardial ischemia-reperfusion injury. Evid-based Compl Alt. 2014;2014:107501.
Chen SY, Hsiao G, Hwang HR, Cheng PY, Lee YM. Tetramethylpyrazine induces heme oxygenase-1 expression and attenuates myocardial ischemia/reperfusion injury in rats. J Biomed Sci. 2006;13:731–40.
Liu X, Rui Z, Xu W, Li C, Zhao Q, Wang X. Synthesis of the novel liqustrazine derivatives and their protective effect on injured vascular endothelial cell damaged by hydrogen peroxide. Bioorg Med Chem Lett. 2003;13:2123–6.
Drag-Zalesinska M, Kulbacka J, Saczko J, Wysocka T, Zabel M, Surowiak P, et al. Esters of betulin and betulinic acid with amino acids have improved water solubility and are selectively cytotoxic toward cancer cells. Bioorg Med Chem Lett. 2009;19:4814–7.
Mcconathy J, Yu W, Jarkas N, Seo W, Schuster D, Goodman M. Radiohalogenated nonnatural amino acids as PET and SPECT tumor imaging agents. Med Res Rev. 2012;32:868–905.
Diaz-Padilla I, Siu LL. Brivanib alaninate for cancer. Expert Opin Inv Drug. 2011;20:577–86.
Cundy KC, Branch R, Chernov-Rogan T, Dias T, Estrada T, Holdet K, et al. XP13512 [(+/−)-1-([(alphaisobutanoyloxyethoxy) carbonyl]amionmethyl)-1-cyclohe -xane acetic acid], a novel gabapentin prodrug: I. Design, synthesis, enzymatic conversion to gabapentin, and transportby intestinal solute transporters. J Pharmacol Exp Ther. 2004;311:315–23.
Lal R, Sukbuntherng J, Tai EH, Upadhyay S, Yao F, Warren M, et al. Arbaclofen placarbil, a novel R-baclofen prodrug: improved absorption, distribution, metabolism, and elimination properties compared with R-baclofen. J Pharm Exp Ther. 2009;330:911–21.
Fu X, Jiang S, Li C, Xin J, Yang Y, Ji R. Design and synthesis of novel bis(L-amino acid) ester prodrugs of 9-[2-(phosphonomethoxy)ethyl]adenine (PMEA) with improved anti-HBV activity. Bioorg Med Chem Lett. 2007;17:465–70.
Nicklin PL, Irwin WJ, Timmins P, Morrison R. Uptake and transport of the ACE-inhibitor ceronapril (SQ 29852) by monolayers of human intestinal absorptive (Caco-2) cells in vitro. Int J Pharm. 1996;140:175–83.
Choi JH, Cha JK, Huh JT. Adenosine diphosphate–induced platelet aggregation might contribute to poor outcomes in atrial fibrillation–related ischemic stroke. J Stroke Cerebrovasc Dis. 2014;23:e215–20.
Dong YX, Zhang XH, Liu MJ, Yang Y, Guo T, Mao YH, et al. Hybrid molecules of scutellarein and tertramethylpyrazine’s active metabolites for ischemic stroke. Bioorg Med Chem Lett. 2019;29:126608.
Samson AL, Alwis I, Maclean J, Priyananda P, Hawkett B, Schoenwaelder S, et al. Endogenous fibrinolysis facilitates clot retraction in vivo. Blood. 2017;130:2453–62.
Durrant TN, van den Bosch MT, Hers I. Integrin αIIbβ3 outside-in signaling. Blood. 2017;130:1607–19.
Lv C, Liu C, Yao Z, Gao X, Sun L, Jia L, et al. The clinical pharmacokinetics and pharmacodynamics of warfarin when combined with compound Danshen: a case study for combined treatment of coronary heart diseases with atrial fibrillation. Front Pharm. 2017;8:00826.
Pan G, Chang L, Zhang J, Liu Y, Ding Z. GSK669, a NOD2 receptor antagonist, inhibits thrombosis and oxidative stress via targeting platelet GPVI. Biochem Pharm. 2021;183:114315.
Hu L, Chang L, Zhang Y, Zhai L, Zhang S, Qi Z, et al. Platelets express activated P2Y12 receptor in patients with diabetes. Circulation. 2017;136:817–33.
Liu MJ, Wu SX, Lei DD, Zhang QY, Dong L, Dong YX. Synthesis and biological evaluation of twin drug of tetramethylpyrazine and scutellarein for ischemic stroke. Chin J N Drug. 2021;30:267–73.
Zhang Y, Ye J, Hu L, Zhang SH, Ding Z. Increased platelet activation and thrombosis in transgenic mice expressing constitutively active P2Y12. J Thromb Haemost. 2012;10:2149–57.
Acknowledgements
This work was supported by National Natural Science Foundation of China (Nos. U1812403 and 81960630), the Department of Science and Technology of Guizhou Province (Nos. 2020-5006, 2020-6011 and 2018-5779), the Department of Education of Guizhou Province (No. 2021-164).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Dong, Y., Wu, S., Liu, M. et al. Conjugates of Tetramethylpyrazine’ metabolites and amino acid as potential antiplatelet agents. Med Chem Res 31, 75–84 (2022). https://doi.org/10.1007/s00044-021-02817-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00044-021-02817-3