Abstract
Aims
Inflammatory bowel disease (IBD) is a global disease. We aim to summarize the latest epidemiological patterns of IBD at the national, regional and global levels to give well-deserved attention and outline facilitating measures to reduce the disease burden.
Methods
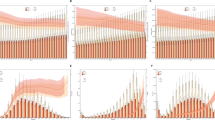
We collected the incidence, prevalence, mortality and disability-adjusted life years (DALYs) of IBD in 204 countries and territories from 1990 to 2019 using data from the Global Burden of Disease Study 2019. We further calculated the estimated annual percentage change (EAPC) to qualify the temporal trends of IBD burden by sex, age and region over the past 30 years.
Results
Globally, a total of 404.55 thousand incident cases, 4898.56 thousand prevalent cases, 41.00 thousand deaths and 1622.50 thousand DALYs of IBD were estimated in 2019. The age-standardized DALYs decreased from 27.2 in 1990 to 20.15 per 100,000 people in 2019, with an EAPC of −1.04. The high socio-demographic index regions presented pronounced age-standardized rates (ASRs) consistently over the last 30 years. The high-income North America had the highest ASRs in 2019, followed by Western Europe and Australasia. No gender difference was observed after being stratified by sex.
Conclusions
The accumulated IBD patients are expected to increase in the future due to the increased rate of IBD in developing countries, and social aging in developed countries. Understanding the changes in epidemiological patterns helps to provide evidence to mitigate the rising burden of IBD.




Similar content being viewed by others
Data availability
All data could be extracted from the online database (http://ghdx.healthdata.org/gbd-results-tool).
Abbreviations
- ASDR:
-
Age-standardized DALY rate
- ASIR:
-
Age-standardized incidence rate
- ASMR:
-
Age-standardized mortality rate
- ASPR:
-
Age-standardized prevalence rate
- ASR:
-
Age-standardized rate
- CI:
-
Confidence interval
- DALY:
-
Disability-adjusted life-year
- EAPC:
-
Estimated annual percentage change
- GBD:
-
Global Burden of Disease Study
- IBD:
-
Inflammatory bowel disease
- SDI:
-
Socio-demographic index
- UI:
-
Uncertainty interval
References
Baumgart DC, Carding SR. Inflammatory bowel disease: cause and immunobiology. Lancet (London, England). 2007;369(9573):1627–40.
Rogler G, Singh A, Kavanaugh A, Rubin DT. Extraintestinal manifestations of inflammatory bowel disease: current concepts, treatment, and implications for disease management. Gastroenterology. 2021;161(4):1118–32.
Kaplan GG. The global burden of IBD: from 2015 to 2025. Nat Rev Gastroenterol Hepatol. 2015;12(12):720–7.
Kawalec P. Indirect costs of inflammatory bowel diseases: Crohn’s disease and ulcerative colitis. A systematic review. Arch Med Sci. 2016;12(2):295–302.
Jairath V, Feagan BG. Global burden of inflammatory bowel disease. The Lancet Gastroenterol Hepatol. 2020;5(1):2–3.
Collaborators GIBD. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet Gastroenterol Hepatol. 2020;5(1):17–30.
Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, Panaccione R, Ghosh S, Wu JCY, Chan FKL, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet (London, England). 2017;390(10114):2769–78.
Piovani D, Danese S. Inflammatory bowel disease: estimates from the global burden of disease 2017 study. Aliment Pharmacol Ther. 2020;51(2):261–70.
Frolkis AD, Lipton DS, Fiest KM, Negrón ME, Dykeman J, deBruyn J, Jette N, Frolkis T, Rezaie A, Seow CH, et al. Cumulative incidence of second intestinal resection in Crohn’s disease: a systematic review and meta-analysis of population-based studies. Am J Gastroenterol. 2014;109(11):1739–48.
Frolkis AD, Dykeman J, Negrón ME, Debruyn J, Jette N, Fiest KM, Frolkis T, Barkema HW, Rioux KP, Panaccione R, et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology. 2013;145(5):996–1006.
Collaborators GRF. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (London, England). 2020;396(10258):1223–49.
Collaborators GDAI. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (London, England). 2020;396(10258):1204–22.
Wang H, Zhao S, Wang S, Zheng Y, Wang S, Chen H, Pang J, Ma J, Yang X, Chen Y. Global magnitude of encephalitis burden and its evolving pattern over the past 30 years. J Infect. 2022;84(6):777–87.
Yang X, Zhang T, Zhang H, Sang S, Chen H, Zuo X. Temporal trend of gastric cancer burden along with its risk factors in China from 1990 to 2019, and projections until 2030: comparison with Japan, South Korea, and Mongolia. Biomark Res. 2021;9(1):84.
Yang X, Fang Y, Chen H, Zhang T, Yin X, Man J, Yang L, Lu M. Global, regional and national burden of anxiety disorders from 1990 to 2019: results from the Global Burden of Disease Study 2019. Epidemiol Psychiatr Scie. 2021;30:e36.
M’Koma AE. Inflammatory bowel disease: an expanding global health problem. Clin Med Insight Gastroenterol. 2013;6:33–47.
Lakatos PL, Vegh Z, Lovasz BD, David G, Pandur T, Erdelyi Z, Szita I, Mester G, Balogh M, Szipocs I, et al. Is current smoking still an important environmental factor in inflammatory bowel diseases? Results from a population-based incident cohort. Inflamm Bowel Dis. 2013;19(5):1010–7.
Lakatos PL, Szamosi T, Lakatos L. Smoking in inflammatory bowel diseases: good, bad or ugly? World J Gastroenterol. 2007;13(46):6134–9.
Ng SC, Bernstein CN, Vatn MH, Lakatos PL, Loftus EV Jr, Tysk C, O’Morain C, Moum B, Colombel JF. Geographical variability and environmental risk factors in inflammatory bowel disease. Gut. 2013;62(4):630–49.
Cosnes J, Carbonnel F, Beaugerie L, Le Quintrec Y, Gendre JP. Effects of cigarette smoking on the long-term course of Crohn’s disease. Gastroenterology. 1996;110(2):424–31.
Shah SC, Khalili H, Gower-Rousseau C, Olen O, Benchimol EI, Lynge E, Nielsen KR, Brassard P, Vutcovici M, Bitton A, et al. Sex-based differences in incidence of inflammatory bowel diseases-pooled analysis of population-based studies from Western countries. Gastroenterology. 2018;155(4):1079-1089.e1073.
Lee JC, Biasci D, Roberts R, Gearry RB, Mansfield JC, Ahmad T, Prescott NJ. Genome-wide association study identifies distinct genetic contributions to prognosis and susceptibility in Crohn’s disease. Nat Genet. 2017;49(2):262–8.
Kaplan GG, Windsor JW. The four epidemiological stages in the global evolution of inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2021;18(1):56–66.
Lirhus SS, Høivik ML, Moum B, Anisdahl K, Melberg HO. Incidence and prevalence of inflammatory bowel disease in norway and the impact of different case definitions: a nationwide registry study. Clin Epidemiol. 2021;13:287–94.
Dhaliwal J, Tuna M, Shah BR, Murthy S, Herrett E, Griffiths AM, Benchimol EI. Incidence of inflammatory bowel disease in south Asian and Chinese people: a population-based Cohort study from Ontario. Can Clin Epidemiol. 2021;13:1109–18.
Niv Y, Abuksis G, Fraser GM. Epidemiology of ulcerative colitis in Israel: a survey of Israeli kibbutz settlements. Am J Gastroenterol. 2000;95(3):693–8.
Birkenfeld S, Zvidi I, Hazazi R, Niv Y. The prevalence of ulcerative colitis in Israel: a twenty-year survey. J Clin Gastroenterol. 2009;43(8):743–6.
Leong RW, Lau JY, Sung JJ. The epidemiology and phenotype of Crohn’s disease in the Chinese population. Inflamm Bowel Dis. 2004;10(5):646–51.
Soon IS, Molodecky NA, Rabi DM, Ghali WA, Barkema HW, Kaplan GG. The relationship between urban environment and the inflammatory bowel diseases: a systematic review and meta-analysis. BMC Gastroenterol. 2012;12:51.
López-Serrano P, Pérez-Calle JL, Pérez-Fernández MT, Fernández-Font JM, Boixeda de Miguel D, Fernández-Rodríguez CM. Environmental risk factors in inflammatory bowel diseases Investigating the hygiene hypothesis: a Spanish case-control study. Scand J Gastroenterol. 2010;45(12):1464–71.
Jakobsen C, Bartek J Jr, Wewer V, Vind I, Munkholm P, Groen R, Paerregaard A. Differences in phenotype and disease course in adult and paediatric inflammatory bowel disease—a population-based study. Aliment Pharmacol Ther. 2011;34(10):1217–24.
Duricova D, Burisch J, Jess T, Gower-Rousseau C, Lakatos PL. Age-related differences in presentation and course of inflammatory bowel disease: an update on the population-based literature. J Crohns Colitis. 2014;8(11):1351–61.
Piovani D, Hassan C, Repici A, Rimassa L, Carlo-Stella C, Nikolopoulos GK, Riboli E, Bonovas S. Risk of cancer in inflammatory bowel diseases: umbrella review and re-analysis of meta-analyses. Gastroenterology. 2022;163:671–84.
Ekbom A, Helmick C, Zack M, Adami HO (2010) Ulcerative colitis and colorectal cancer. A population-based study. N Engl J Med 2010(18):1228–33.
Kaplan GG, Ng SC. Understanding and preventing the global increase of inflammatory Bowel disease. Gastroenterology. 2017;152(2):313-321.e312.
Hou JK, Abraham B, El-Serag H. Dietary intake and risk of developing inflammatory bowel disease: a systematic review of the literature. Am J Gastroenterol. 2011;106(4):563–73.
Riordan AM, Ruxton CH, Hunter JO. A review of associations between Crohn’s disease and consumption of sugars. Eur J Clin Nutr. 1998;52(4):229–38.
Ananthakrishnan AN, Khalili H, Konijeti GG, Higuchi LM, de Silva P, Fuchs CS, Willett WC, Richter JM, Chan AT. Long-term intake of dietary fat and risk of ulcerative colitis and Crohn’s disease. Gut. 2014;63(5):776–84.
Jantchou P, Morois S, Clavel-Chapelon F, Boutron-Ruault MC, Carbonnel F. Animal protein intake and risk of inflammatory bowel disease: the E3N prospective study. Am J Gastroenterol. 2010;105(10):2195–201.
Opstelten JL, de Vries JHM, Wools A, Siersema PD, Oldenburg B, Witteman BJM. Dietary intake of patients with inflammatory bowel disease: a comparison with individuals from a general population and associations with relapse. Clin Nutr (Edinburgh, Scotland). 2019;38(4):1892–8.
Sajadinejad MS, Asgari K, Molavi H, Kalantari M, Adibi P. Psychological issues in inflammatory bowel disease: an overview. Gastroenterol Res Pract. 2012;2012:106502.
Maunder RG, Levenstein S. The role of stress in the development and clinical course of inflammatory bowel disease: epidemiological evidence. Curr Mol Med. 2008;8(4):247–52.
Yang X, Yang L, Zhang T, Zhang H, Chen H, Zuo X. Causal atlas between inflammatory bowel disease and mental disorders: a bi-directional 2-sample Mendelian randomization study. Front Immunol. 2023;14:1267834.
Szigethy EM, Allen JI, Reiss M, Cohen W, Perera LP, Brillstein L, Cross RK, Schwartz DA, Kosinski LR, Colton JB, et al. White Paper AGA: the impact of mental and psychosocial factors on the care of patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2017;15(7):986–97.
Bonaz BL, Bernstein CN. Brain-gut interactions in inflammatory bowel disease. Gastroenterology. 2013;144(1):36–49.
Gracie DJ, Hamlin PJ, Ford AC. The influence of the brain-gut axis in inflammatory bowel disease and possible implications for treatment. The Lancet Gastroenterol Hepatol. 2019;4(8):632–42.
Lewin S, Lees C, Regueiro M, Hart A, Mahadevan U. International organization for the study of inflammatory bowel disease: global strategies for telemedicine and inflammatory Bowel diseases. J Crohns Colitis. 2020;14(14 Suppl 3):S780-s784.
Brenner EJ, Ungaro RC, Gearry RB, Kaplan GG, Kissous-Hunt M, Lewis JD, Ng SC, Rahier JF, Reinisch W, Ruemmele FM, et al. Corticosteroids, but not TNF antagonists, are associated with adverse COVID-19 outcomes in patients with inflammatory Bowel diseases: results from an international registry. Gastroenterology. 2020;159(2):481-491.e483.
Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR, Caprilli R, Colombel JF, Gasche C, Geboes K, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005;19(Suppl A):5a–36a.
Acknowledgements
The authors thank the countless individuals who have contributed to the Global Burden of Disease Study 2019 in various capacities.
Funding
This work was supported by the National Natural Science Foundation of China (82103912), China Postdoctoral Science Foundation (2021M700080), Shandong Provincial Natural Science Foundation (ZR2020QH302), and Clinical Research Center of Shandong University (2021SDUCRCB003). The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all of the data and the final responsibility to submit it for publication.
Author information
Authors and Affiliations
Contributions
Conception and design: Xiaorong Yang, Xiaoyun Yang. Data collection: Lina Cao, Alimu Dayimu, Guan Xiao, Miao Duan, Shuyan Zeng, Hui Wang, Jiahao Zong, Chunhua Sun. Data analyses: Lina Cao, Xiaorong Yang. Results visualization: Lina Cao, Alimu Dayimu, Guan Xiao, Miao Duan, Shuyan Zeng, Hui Wang, Jiahao Zong. Results interpretations: all authors. Manuscript writing_draft: Lina Cao. Manuscript writing_revision: all authors. Final approval of manuscript: all authors.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest.
Ethics approval and consent to participate
The GBD 2019 study is a publicly available database and all data were anonymous. Our study protocol was approved by the Institutional Review Boards of Qilu Hospital of Shandong University with approval number KYLL-202011(KS)-239.
Consent for publication
Not applicable.
Additional information
Responsible Editor: John Di Battista.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cao, L., Dayimu, A., Guan, X. et al. Global evolving patterns and cross-country inequalities of inflammatory bowel disease burden from 1990 to 2019: a worldwide report. Inflamm. Res. 73, 277–287 (2024). https://doi.org/10.1007/s00011-023-01836-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-023-01836-7