Abstract
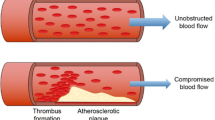
Globally, the number of deaths caused by various diseases varies according to geographical distribution, gender, and age. Among all types of noncommunicable diseases, cardiovascular diseases such as atherosclerosis, thrombosis, acute myocardial infarction, stroke cause the largest number of deaths, which brings huge health and economic burdens to patients, their families, and the entire society. In clinic, rapid diagnosis and effective therapeutic intervention of cardiovascular diseases are the key to save patients’ lives. However, the conventional diagnosis technology and treatment methods are facing many bottlenecks. There is an urgent need to develop novel theranostic strategies. As a multidisciplinary discipline, the development of nanomaterials and nanostructure-based nanotechnology may provide an alternative and novel direction for the early diagnosis and research of cardiovascular diseases. The application of technologies such as multimodal molecular imaging, ultra-sensitive biosensing, targeted drug delivery, minimally invasive intervention has effectively improved the efficiency of diagnosis and treatment of cardiovascular diseases. This chapter will cover the latest applications and prospects of nanotechnology in the diagnosis and treatment of cardiovascular diseases.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
Reference
Diseases GBD, Injuries C (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396:1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9
Fonarow GC et al (2014) Door-to-needle times for tissue plasminogen activator administration and clinical outcomes in acute ischemic stroke before and after a quality improvement initiative. JAMA 311:1632–1640. https://doi.org/10.1001/jama.2014.3203
Menees DS et al (2013) Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med 369:901–909. https://doi.org/10.1056/NEJMoa1208200
Park HB et al (2015) Atherosclerotic plaque characteristics by CT angiography identify coronary lesions that cause ischemia: a direct comparison to fractional flow reserve. JACC Cardiovasc Imaging 8:1–10. https://doi.org/10.1016/j.jcmg.2014.11.002
Lohrke J et al (2016) 25 years of contrast-enhanced MRI: developments, current challenges and future perspectives. Adv Ther 33:1–28. https://doi.org/10.1007/s12325-015-0275-4
Rodriguez-Luna D, Molina CA (2016) Vascular imaging: ultrasound. Handb Clin Neurol 136:1055–1064. https://doi.org/10.1016/B978-0-444-53486-6.00055-7
Demchuk AM, Menon BK, Goyal M (2016) Comparing vessel imaging: noncontrast computed tomography/computed tomographic angiography should be the new minimum standard in acute disabling stroke. Stroke 47:273–281. https://doi.org/10.1161/STROKEAHA.115.009171
Yaghi S et al (2017) Treatment and outcome of hemorrhagic transformation after intravenous alteplase in acute ischemic stroke: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 48:e343–e361. https://doi.org/10.1161/STR.0000000000000152
Wiendl H et al (2015) Gaps between aims and achievements in therapeutic modification of neuronal damage (“neuroprotection”). Neurotherapeutics 12:449–454. https://doi.org/10.1007/s13311-015-0348-8
Muthu MS, Leong DT, Mei L, Feng SS (2014) Nanotheranostics – application and further development of nanomedicine strategies for advanced theranostics. Theranostics 4:660–677. https://doi.org/10.7150/thno.8698
Cheng Z, Al Zaki A, Hui JZ, Muzykantov VR, Tsourkas A (2012) Multifunctional nanoparticles: cost versus benefit of adding targeting and imaging capabilities. Science 338:903–910. https://doi.org/10.1126/science.1226338
Singh P et al (2016) Biomedical perspective of electrochemical nanobiosensor. Nano Lett 8:193–203. https://doi.org/10.1007/s40820-015-0077-x
Jatzkewitz H (1954) Incorporation of physiologically-active substances into a colloidal blood plasma substitute. I. Incorporation of mescaline peptide into polyvinylpyrrolidone. Hoppe Seylers Z Physiol Chem 297:149–156
De La Vega JC, Hafeli UO (2015) Utilization of nanoparticles as X-ray contrast agents for diagnostic imaging applications. Contrast Media Mol Imaging 10:81–95. https://doi.org/10.1002/cmmi.1613
Lee N, Choi SH, Hyeon T (2013) Nano-sized CT contrast agents. Adv Mater 25:2641–2660. https://doi.org/10.1002/adma.201300081
Hainfeld JF, Slatkin DN, Focella TM, Smilowitz HM (2006) Gold nanoparticles: a new X-ray contrast agent. Br J Radiol 79:248–253. https://doi.org/10.1259/bjr/13169882
Chhour P et al (2016) Labeling monocytes with gold nanoparticles to track their recruitment in atherosclerosis with computed tomography. Biomaterials 87:93–103. https://doi.org/10.1016/j.biomaterials.2016.02.009
Kim JY et al (2015) Direct imaging of cerebral thromboemboli using computed tomography and fibrin-targeted gold nanoparticles. Theranostics 5:1098–1114. https://doi.org/10.7150/thno.11679
Beard P (2011) Biomedical photoacoustic imaging. Interface Focus 1:602–631. https://doi.org/10.1098/rsfs.2011.0028
Weber J, Beard PC, Bohndiek SE (2016) Contrast agents for molecular photoacoustic imaging. Nat Methods 13:639–650. https://doi.org/10.1038/nmeth.3929
Yang L et al (2020) Indocyanine green assembled Nanobubbles with enhanced fluorescence and Photostability. Langmuir 36:12983–12989. https://doi.org/10.1021/acs.langmuir.0c02288
Li W, Chen X (2015) Gold nanoparticles for photoacoustic imaging. Nanomedicine (Lond) 10:299–320. https://doi.org/10.2217/nnm.14.169
Varna M, Xuan HV, Fort E (2018) Gold nanoparticles in cardiovascular imaging. Wiley Interdiscip Rev Nanomed Nanobiotechnol 10. https://doi.org/10.1002/wnan.1470
Agrawal A et al (2006) Quantitative evaluation of optical coherence tomography signal enhancement with gold nanoshells. J Biomed Opt 11:041121. https://doi.org/10.1117/1.2339071
Lopez-Chaves C et al (2018) Gold nanoparticles: distribution, bioaccumulation and toxicity. In vitro and in vivo studies. Nanomedicine 14:1–12. https://doi.org/10.1016/j.nano.2017.08.011
Saam T et al (2007) The vulnerable, or high-risk, atherosclerotic plaque: noninvasive MR imaging for characterization and assessment. Radiology 244:64–77. https://doi.org/10.1148/radiol.2441051769
Merino JG, Warach S (2010) Imaging of acute stroke. Nat Rev Neurol 6:560–571. https://doi.org/10.1038/nrneurol.2010.129
Vazquez-Prada KX et al (2021) Targeted molecular imaging of cardiovascular diseases by iron oxide nanoparticles. Arterioscler Thromb Vasc Biol 41:601–613. https://doi.org/10.1161/ATVBAHA.120.315404
Dadfar SM et al (2019) Iron oxide nanoparticles: diagnostic, therapeutic and theranostic applications. Adv Drug Deliv Rev 138:302–325. https://doi.org/10.1016/j.addr.2019.01.005
Chen B et al (2018) Ferumoxytol of ultrahigh magnetization produced by hydrocooling and magnetically internal heating co-precipitation. Nanoscale 10:7369–7376. https://doi.org/10.1039/c8nr00736e
Chen B et al (2020) Moderate cooling coprecipitation for extremely small iron oxide as a pH dependent T-1-MRI contrast agent. Nanoscale 12:5521–5532. https://doi.org/10.1039/c9nr10397j
Bai C et al (2018) Time-dependent t-1-t-2 switchable magnetic resonance imaging realized by c(rgdyk) modified ultrasmall Fe3O4 nanoprobes. Adv Funct Mater 28. https://doi.org/10.1002/adfm.201802281
Zhang H et al (2017) Ultrasmall ferrite nanoparticles synthesized via dynamic simultaneous thermal decomposition for high-performance and multifunctional T1 magnetic resonance imaging contrast agent. ACS Nano 11:3614–3631. https://doi.org/10.1021/acsnano.6b07684
Liu Y, Li M, Yang F, Gu N (2017) Magnetic drug delivery systems. Sci China Mater 60:471–486. https://doi.org/10.1007/s40843-017-9049-0
Faust O et al (2017) Computer aided diagnosis of coronary artery disease, myocardial infarction and carotid atherosclerosis using ultrasound images: a review. Phys Med 33:1–15. https://doi.org/10.1016/j.ejmp.2016.12.005
Darmoch F et al (2020) Intravascular ultrasound imaging-guided versus coronary angiography-guided percutaneous coronary intervention: a systematic review and meta-analysis. J Am Heart Assoc 9:e013678. https://doi.org/10.1161/JAHA.119.013678
Rix A, Curaj A, Liehn E, Kiessling F (2020) Ultrasound microbubbles for diagnosis and treatment of cardiovascular diseases. Semin Thromb Hemost 46:545–552. https://doi.org/10.1055/s-0039-1688492
Partovi S et al (2012) Contrast-enhanced ultrasound for assessing carotid atherosclerotic plaque lesions. AJR Am J Roentgenol 198:W13–W19. https://doi.org/10.2214/AJR.11.7312
Schumann PA et al (2002) Targeted-microbubble binding selectively to GPIIb IIIa receptors of platelet thrombi. Investig Radiol 37:587–593. https://doi.org/10.1097/00004424-200211000-00001
Wang X et al (2012) Novel single-chain antibody-targeted microbubbles for molecular ultrasound imaging of thrombosis: validation of a unique noninvasive method for rapid and sensitive detection of thrombi and monitoring of success or failure of thrombolysis in mice. Circulation 125:3117–3126. https://doi.org/10.1161/CIRCULATIONAHA.111.030312
Unger E, Porter T, Lindner J, Grayburn P (2014) Cardiovascular drug delivery with ultrasound and microbubbles. Adv Drug Deliv Rev 72:110–126. https://doi.org/10.1016/j.addr.2014.01.012
Qian L et al (2018) The present and future role of ultrasound targeted microbubble destruction in preclinical studies of cardiac gene therapy. J Thorac Dis 10:1099–1111. https://doi.org/10.21037/jtd.2018.01.101
Fix SM, Borden MA, Dayton PA (2015) Therapeutic gas delivery via microbubbles and liposomes. J Control Release 209:139–149. https://doi.org/10.1016/j.jconrel.2015.04.027
Chandan R, Mehta S, Banerjee R (2020) Ultrasound-responsive carriers for therapeutic applications. ACS Biomater Sci Eng 6:4731–4747. https://doi.org/10.1021/acsbiomaterials.9b01979
Deprez J, Lajoinie G, Engelen Y, De Smedt SC, Lentacker I (2021) Opening doors with ultrasound and microbubbles: beating biological barriers to promote drug delivery. Adv Drug Deliv Rev 172:9–36. https://doi.org/10.1016/j.addr.2021.02.015
Tu Y, Sun Y, Fan Y, Cheng Z, Yu B (2018) Multimodality molecular imaging of cardiovascular disease based on nanoprobes. Cell Physiol Biochem 48:1401–1415. https://doi.org/10.1159/000492251
Yang F et al (2009) Superparamagnetic iron oxide nanoparticle-embedded encapsulated microbubbles as dual contrast agents of magnetic resonance and ultrasound imaging. Biomaterials 30:3882–3890. https://doi.org/10.1016/j.biomaterials.2009.03.051
Yang F et al (2012) A hydrogen peroxide-responsive O(2) nanogenerator for ultrasound and magnetic-resonance dual modality imaging. Adv Mater 24:5205–5211. https://doi.org/10.1002/adma.201202367
Yang F et al (2013) Silver nanoparticle-embedded microbubble as a dual-mode ultrasound and optical imaging probe. ACS Appl Mater Interfaces 5:9217–9223. https://doi.org/10.1021/am4029747
Liu Y et al (2017) Magnetic nanoliposomes as in situ microbubble bombers for multimodality image-guided cancer theranostics. ACS Nano 11:1509–1519. https://doi.org/10.1021/acsnano.6b06815
Ding J et al (2013) CT/fluorescence dual-modal nanoemulsion platform for investigating atherosclerotic plaques. Biomaterials 34:209–216. https://doi.org/10.1016/j.biomaterials.2012.09.025
Nahrendorf M et al (2009) Hybrid in vivo FMT-CT imaging of protease activity in atherosclerosis with customized nanosensors. Arterioscler Thromb Vasc Biol 29:1444–1451. https://doi.org/10.1161/ATVBAHA.109.193086
Altintas Z, Fakanya WM, Tothill IE (2014) Cardiovascular disease detection using bio-sensing techniques. Talanta 128:177–186. https://doi.org/10.1016/j.talanta.2014.04.060
Zong C et al (2018) Surface-enhanced Raman spectroscopy for bioanalysis: reliability and challenges. Chem Rev 118:4946–4980. https://doi.org/10.1021/acs.chemrev.7b00668
Fu X et al (2019) A graphene oxide/gold nanoparticle-based amplification method for SERS immunoassay of cardiac troponin I. Analyst 144:1582–1589. https://doi.org/10.1039/c8an02022a
Laing S, Jamieson LE, Faulds K, Graham D (2017) Surface-enhanced Raman spectroscopy for in vivo biosensing. Nat Rev Chem 1. https://doi.org/10.1038/s41570-017-0060
Henry AI, Sharma B, Cardinal MF, Kurouski D, Van Duyne RP (2016) Surface-enhanced raman spectroscopy biosensing: in vivo diagnostics and multimodal imaging. Anal Chem 88:6638–6647. https://doi.org/10.1021/acs.analchem.6b01597
McQueenie R et al (2012) Detection of inflammation in vivo by surface-enhanced Raman scattering provides higher sensitivity than conventional fluorescence imaging. Anal Chem 84:5968–5975. https://doi.org/10.1021/ac3006445
Ahammad AJS et al (2011) Electrochemical detection of cardiac biomarker troponin I at gold nanoparticle-modified ? To electrode by using open circuit potential. Int J Electrochem Sci 6:1906–1916
Periyakaruppan A, Gandhiraman RP, Meyyappan M, Koehne JE (2013) Label-free detection of cardiac troponin-I using carbon nanofiber based nanoelectrode arrays. Anal Chem 85:3858–3863. https://doi.org/10.1021/ac302801z
Suprun E et al (2010) Electrochemical nanobiosensor for express diagnosis of acute myocardial infarction in undiluted plasma. Biosens Bioelectron 25:1694–1698. https://doi.org/10.1016/j.bios.2009.12.009
Metkar SK, Girigoswami K (2019) Diagnostic biosensors in medicine – a review. Biocatal Agric Biotechnol 17:271–283. https://doi.org/10.1016/j.bcab.2018.11.029
Regan B, Boyle F, O’Kennedy R, Collins D (2019) Evaluation of molecularly imprinted polymers for point-of-care testing for cardiovascular disease. Sensors (Basel) 19. https://doi.org/10.3390/s19163485
Vasantham S et al (2019) Paper based point of care immunosensor for the impedimetric detection of cardiac troponin I biomarker. Biomed Microdevices 22:6. https://doi.org/10.1007/s10544-019-0463-0
Phonklam K, Wannapob R, Sriwimol W, Thavarungkul P, Phairatana T (2020) A novel molecularly imprinted polymer PMB/MWCNTs sensor for highly-sensitive cardiac troponin T detection. Sensors Actuators B Chem 308. https://doi.org/10.1016/j.snb.2019.127630
Mansuriya BD, Altintas Z (2020) Applications of graphene quantum dots in biomedical sensors. Sensors (Basel) 20. https://doi.org/10.3390/s20041072
Mukherjee A, Shim Y, Myong Song J (2016) Quantum dot as probe for disease diagnosis and monitoring. Biotechnol J 11:31–42. https://doi.org/10.1002/biot.201500219
Yola ML, Atar N (2019) Development of cardiac troponin-I biosensor based on boron nitride quantum dots including molecularly imprinted polymer. Biosens Bioelectron 126:418–424. https://doi.org/10.1016/j.bios.2018.11.016
Sun J et al (2018) Comet-like heterodimers “gold nanoflower @graphene quantum dots” probe with fret “off” to DNA circuit signal “on” for sensing and imaging microrna in vitro and in vivo. Anal Chem 90:11538–11547. https://doi.org/10.1021/acs.analchem.8b02854
Jain KK (2008) Drug delivery systems – an overview. Methods Mol Biol 437:1–50. https://doi.org/10.1007/978-1-59745-210-6_1
El-Say KM, El-Sawy HS (2017) Polymeric nanoparticles: promising platform for drug delivery. Int J Pharm 528:675–691. https://doi.org/10.1016/j.ijpharm.2017.06.052
Banik BL, Fattahi P, Brown JL (2016) Polymeric nanoparticles: the future of nanomedicine. Wiley Interdiscip Rev Nanomed Nanobiotechnol 8:271–299. https://doi.org/10.1002/wnan.1364
Larson N, Ghandehari H (2012) Polymeric conjugates for drug delivery. Chem Mater 24:840–853. https://doi.org/10.1021/cm2031569
Shamay Y, Paulin D, Ashkenasy G, David A (2009) E-selectin binding peptide-polymer-drug conjugates and their selective cytotoxicity against vascular endothelial cells. Biomaterials 30:6460–6468. https://doi.org/10.1016/j.biomaterials.2009.08.013
Ward MA, Georgiou TK (2011) Thermoresponsive polymers for biomedical applications. Polymers-Basel 3:1215–1242. https://doi.org/10.3390/polym3031215
Alvarez-Lorenzo C, Bromberg L, Concheiro A (2009) Light-sensitive intelligent drug delivery systems. Photochem Photobiol 85:848–860. https://doi.org/10.1111/j.1751-1097.2008.00530.x
Ge J, Neofytou E, Cahill TJ 3rd, Beygui RE, Zare RN (2012) Drug release from electric-field-responsive nanoparticles. ACS Nano 6:227–233. https://doi.org/10.1021/nn203430m
Thevenot J, Oliveira H, Sandre O, Lecommandoux S (2013) Magnetic responsive polymer composite materials. Chem Soc Rev 42:7099–7116. https://doi.org/10.1039/c3cs60058k
Hernot S, Klibanov AL (2008) Microbubbles in ultrasound-triggered drug and gene delivery. Adv Drug Deliv Rev 60:1153–1166. https://doi.org/10.1016/j.addr.2008.03.005
Wang J, Kaplan JA, Colson YL, Grinstaff MW (2017) Mechanoresponsive materials for drug delivery: harnessing forces for controlled release. Adv Drug Deliv Rev 108:68–82. https://doi.org/10.1016/j.addr.2016.11.001
Korin N et al (2012) Shear-activated nanotherapeutics for drug targeting to obstructed blood vessels. Science 337:738–742. https://doi.org/10.1126/science.1217815
Gao W, Chan JM, Farokhzad OC (2010) pH-responsive nanoparticles for drug delivery. Mol Pharm 7:1913–1920. https://doi.org/10.1021/mp100253e
Huo M, Yuan J, Tao L, Wei Y (2014) Redox-responsive polymers for drug delivery: from molecular design to applications. Polym Chem 5:1519–1528. https://doi.org/10.1039/c3py01192e
de la Rica R, Aili D, Stevens MM (2012) Enzyme-responsive nanoparticles for drug release and diagnostics. Adv Drug Deliv Rev 64:967–978. https://doi.org/10.1016/j.addr.2012.01.002
Hu X, Li FY, Wang SY, Xia F, Ling DS (2018) Biological stimulus-driven assembly/disassembly of functional nanoparticles for targeted delivery, controlled activation, and bioelimination. Adv Healthc Mater 7. https://doi.org/10.1002/adhm.201800359
Cheng R, Meng FH, Deng C, Klok HA, Zhong ZY (2013) Dual and multi-stimuli responsive polymeric nanoparticles for programmed site-specific drug delivery. Biomaterials 34:3647–3657. https://doi.org/10.1016/j.biomaterials.2013.01.084
Yu MM et al (2015) Recent advances in dendrimer research for cardiovascular diseases. Biomacromolecules 16:2588–2598. https://doi.org/10.1021/acs.biomac.5b00979
Pradhan D et al (2019) Dendrimer grafted albumin nanoparticles for the treatment of post cerebral stroke damages: a proof of concept study. Colloid Surf B 184. https://doi.org/10.1016/j.colsurfb.2019.110488
Won YW et al (2013) Post-translational regulation of a hypoxia-responsive VEGF plasmid for the treatment of myocardial ischemia. Biomaterials 34:6229–6238. https://doi.org/10.1016/j.biomaterials.2013.04.061
Bader H, Ringsdorf H, Schmidt B (1984) Watersoluble polymers in medicine. Angew Makromol Chem 123:457–485. https://doi.org/10.1002/apmc.1984.051230121
Yokoyama M (2014) Polymeric micelles as drug carriers: their lights and shadows. J Drug Target 22:576–583. https://doi.org/10.3109/1061186x.2014.934688
Jin Q et al (2017) Edaravone-encapsulated agonistic micelles rescue ischemic brain tissue by tuning blood-brain barrier permeability. Theranostics 7:884–898. https://doi.org/10.7150/thno.18219
Bangham AD, Standish MM, Watkins JC (1965) Diffusion of univalent ions across lamellae of swollen phospholipids. J Mol Biol 13:238-+. https://doi.org/10.1016/S0022-2836(65)80093-6
Bowey K, Tanguay JF, Tabrizian M (2012) Liposome technology for cardiovascular disease treatment and diagnosis. Expert Opin Drug Deliv 9:249–265. https://doi.org/10.1517/17425247.2012.647908
Saxena V et al (2015) Temperature-sensitive liposome-mediated delivery of thrombolytic agents. Int J Hyperth 31:67–73. https://doi.org/10.3109/02656736.2014.991428
Wang HJ et al (2020) Liposomal 9-aminoacridine for treatment of ischemic stroke: from drug discovery to drug delivery. Nano Lett 20:1542–1551. https://doi.org/10.1021/acs.nanolett.9b04018
Tapeinos C, Battaglini M, Ciofani G (2017) Advances in the design of solid lipid nanoparticles and nanostructured lipid carriers for targeting brain diseases. J Control Release 264:306–332. https://doi.org/10.1016/j.jconrel.2017.08.033
Tan ME et al (2017) Development of solid lipid nanoparticles containing total flavonoid extract from Dracocephalum moldavica L. and their therapeutic effect against myocardial ischemia-reperfusion injury in rats. Int J Nanomedicine 12:3253–3265. https://doi.org/10.2147/Ijn.S131893
Banskota S, Yousefpour P, Chilkoti A (2017) Cell-based biohybrid drug delivery systems: the best of the synthetic and natural worlds. Macromol Biosci 17. https://doi.org/10.1002/mabi.201600361
Song YA et al (2019) Platelet membrane-coated nanoparticle-mediated targeting delivery of rapamycin blocks atherosclerotic plaque development and stabilizes plaque in apolipoprotein E-deficient (ApoE(-/-)) mice. Nanomed-Nanotechnol 15:13–24. https://doi.org/10.1016/j.nano.2018.08.002
Zhang C et al (2017) Direct macromolecular drug delivery to cerebral ischemia area using neutrophil-mediated nanoparticles. Theranostics 7:3260–3275. https://doi.org/10.7150/thno.19979
Li M et al (2018) Platelet bio-nanobubbles as microvascular recanalization nanoformulation for acute ischemic stroke lesion theranostics. Theranostics 8:4870–4883. https://doi.org/10.7150/thno.27466
Li M et al (2020) Platelet membrane biomimetic magnetic nanocarriers for targeted delivery and in situ generation of nitric oxide in early ischemic stroke. ACS Nano 14:2024–2035. https://doi.org/10.1021/acsnano.9b08587
Xu JP et al (2019) Sequentially site-specific delivery of thrombolytics and neuroprotectant for enhanced treatment of ischemic stroke. ACS Nano 13:8577–8588. https://doi.org/10.1021/acsnano.9b01798
Tang J et al (2017) Therapeutic microparticles functionalized with biomimetic cardiac stem cell membranes and secretome. Nat Commun 8:13724. https://doi.org/10.1038/ncomms13724
Tang J et al (2018) Targeted repair of heart injury by stem cells fused with platelet nanovesicles. Nat Biomed Eng 2:17–26. https://doi.org/10.1038/s41551-017-0182-x
Batrakova EV, Kim MS (2015) Using exosomes, naturally-equipped nanocarriers, for drug delivery. J Control Release 219:396–405. https://doi.org/10.1016/j.jconrel.2015.07.030
Yang JL, Zhang XF, Chen XJ, Wang L, Yang GD (2017) Exosome mediated delivery of mir-124 promotes neurogenesis after ischemia. Mol Ther–Nucleic Acids 7:278–287. https://doi.org/10.1016/j.omtn.2017.04.010
Khan M et al (2015) Embryonic stem cell-derived exosomes promote endogenous repair mechanisms and enhance cardiac function following myocardial infarction. Circ Res 117:52–64. https://doi.org/10.1161/Circresaha.117.305990
Tian T et al (2018) Surface functionalized exosomes as targeted drug delivery vehicles for cerebral ischemia therapy. Biomaterials 150:137–149. https://doi.org/10.1016/j.biomaterials.2017.10.012
Lu ZR (2014) Theranostics: fusion of therapeutics and diagnostics. Pharm Res 31:1355–1357. https://doi.org/10.1007/s11095-014-1343-1
Yang F et al (2016) Glucose and magnetic-responsive approach toward in situ nitric oxide bubbles controlled generation for hyperglycemia theranostics. J Control Release 228:87–95. https://doi.org/10.1016/j.jconrel.2016.03.002
Huang P et al (2011) Folic acid-conjugated silica-modified gold nanorods for X-ray/CT imaging-guided dual-mode radiation and photo-thermal therapy. Biomaterials 32:9796–9809. https://doi.org/10.1016/j.biomaterials.2011.08.086
Lovell JF et al (2011) Porphysome nanovesicles generated by porphyrin bilayers for use as multimodal biophotonic contrast agents. Nat Mater 10:324–332. https://doi.org/10.1038/Nmat2986
Bao G, Mitragotri S, Tong S (2013) Multifunctional nanoparticles for drug delivery and molecular imaging. Annu Rev Biomed Eng 15:253–282. https://doi.org/10.1146/annurev-bioeng-071812-152409
Li S, Sengupta D, Chien S (2014) Vascular tissue engineering: from in vitro to in situ. WIREs Syst Biol Med 6:61–76. https://doi.org/10.1002/wsbm.1246
Gruntzig AR, Senning A, Siegenthaler WE (1979) Nonoperative dilatation of coronary-artery stenosis – percutaneous trans-luminal coronary angioplasty. N Engl J Med 301:61–68. https://doi.org/10.1056/Nejm197907123010201
Bagheri M, Mohammadi M, Steele TWJ, Ramezani M (2016) Nanomaterial coatings applied on stent surfaces. Nanomedicine 11:1309–1326. https://doi.org/10.2217/nnm-2015-0007
Goh D et al (2013) Nanotechnology-based gene-eluting stents. Mol Pharm 10:1279–1298. https://doi.org/10.1021/mp3006616
Palmerini T et al (2014) Clinical outcomes with bioabsorbable polymer-versus durable polymer-based drug-eluting and bare-metal stents evidence from a comprehensive network meta-analysis. J Am Coll Cardiol 63:299–307. https://doi.org/10.1016/j.jacc.2013.09.061
Im SH, Jung Y, Kim SH (2017) Current status and future direction of biodegradable metallic and polymeric vascular scaffolds for next-generation stents. Acta Biomater 60:3–22. https://doi.org/10.1016/j.actbio.2017.07.019
Pashneh-Tala S, MacNeil S, Claeyssens F (2016) The tissue-engineered vascular graft-past, present, and future. Tissue Eng Part B Rev 22:68–100. https://doi.org/10.1089/ten.teb.2015.0100
Ren XK et al (2015) Surface modification and endothelialization of biomaterials as potential scaffolds for vascular tissue engineering applications. Chem Soc Rev 44:5680–5742. https://doi.org/10.1039/C4CS00483C
Zhuang Y et al (2021) Challenges and strategies for in situ endothelialization and long-term lumen patency of vascular grafts. Bioact Mater 6:1791–1809. https://doi.org/10.1016/j.bioactmat.2020.11.028
Ghorbani F, Zamanian A, Shams A, Shamoosi A, Aidun A (2019) Fabrication and characterisation of super-paramagnetic responsive PLGA-gelatine-magnetite scaffolds with the unidirectional porous structure: a physicochemical, mechanical, and in vitro evaluation. IET Nanobiotechnol 13:860–867. https://doi.org/10.1049/iet-nbt.2018.5305
Ishii M et al (2011) Enhanced angiogenesis by transplantation of mesenchymal stem cell sheet created by a novel magnetic tissue engineering method. Arterioscler Thromb Vasc Biol 31:2210–2215. https://doi.org/10.1161/Atvbaha.111.231100
Liu X et al (2022) Novel magnetic silk fibroin scaffolds with delayed degradation for potential long-distance vascular repair. Bioact Mater 7:126–143. https://doi.org/10.1016/j.bioactmat.2021.04.036
Flores D, Yu XJ (2017) Innovative tissue-engineered and synthetic vascular graft models for the treatment of PAD in small-diameter arteries. Regen Eng Transl Med 3:215–223. https://doi.org/10.1007/s40883-017-0040-0
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 Springer Nature Singapore Pte Ltd.
About this entry
Cite this entry
Li, M., Yang, F. (2023). Cardiovascular Nanotechnology. In: Gu, N. (eds) Nanomedicine. Micro/Nano Technologies. Springer, Singapore. https://doi.org/10.1007/978-981-16-8984-0_12
Download citation
DOI: https://doi.org/10.1007/978-981-16-8984-0_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-8983-3
Online ISBN: 978-981-16-8984-0
eBook Packages: EngineeringReference Module Computer Science and Engineering